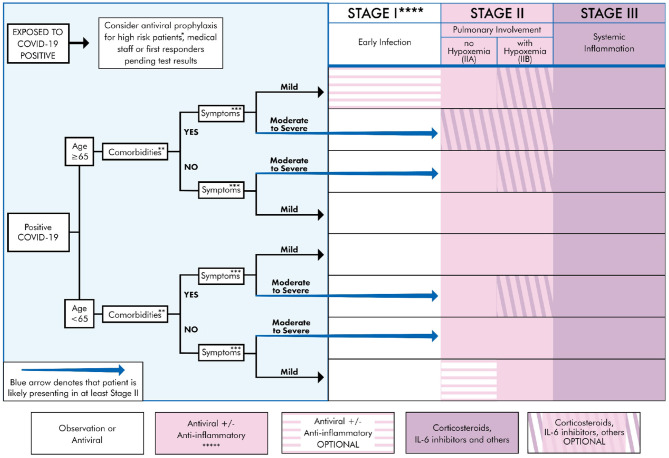
Figure 3.
Treatment algorithm for COVID-19+ patients based on clinical presentation and therapeutic staging. *High risk patient: Anyone that is ≥65 y/o or meets comorbidities criteria as defined below. **Comorbidities: Defined as any two of the following: HTN, DM, CVD, CKD, Pre-existing lung disease, CHF, diabetes >7.6%, use of biologicals, HIV+, history of transplant, morbid obesity (BMI ≥ 40) (21, 22). ***Symptoms Mild: Fever, cough, fatigue, myalgia, headache, anosmia. Rarely, patients may also present with diarrhea, nausea, and vomiting (8, 21, 23). Moderate: Symptomatic viral pneumonia with possible hypoxemia (PaO2/FiO2 < 300). Confirmed by chest imaging (CXR or CT) which demonstrate bilateral infiltrates or ground glass opacities (21). Severe symptoms: Systemic (extra-pulmonary) hyperinflammation with one of the following: respiratory rate > 30 or SpO2 < 92% on room air (11, 17). Will also include abnormal chest imaging (CXR, CT scan, or lung ultrasound) characterized by bilateral opacities that are not primarily due to volume overload or lung collapse (partial or full). Echocardiogram can be used rule out of primary cardiac causes (24, 25). ****See Table 1 for appropriate Rx for stage. Treatment must be individualized to the patient by considering risks, benefits, and contraindications of the particular Rx. Note: there may be a potential for combining multiple agents if no drug interaction exists, as there are pleural mechanisms of actions. *****Convalescent plasma can be used during any stage, though likely more beneficial earlier in the disease course (63).