Figure 5.
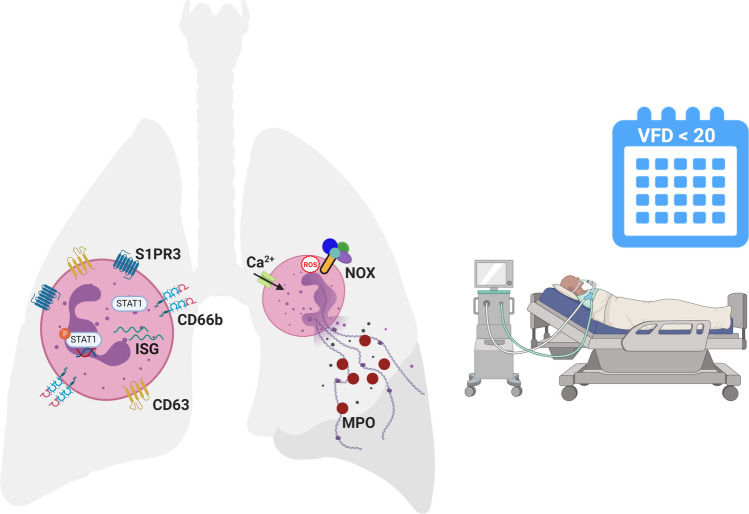
Airway neutrophils are activated in intubated children with compared to children without PARDS. Surface expression of the primary granule exocytosis marker, CD63, and the lipid signaling G protein-coupled receptor, sphingosine-1-phosphate receptor 3 (S1PR3), are higher in children with versus without PARDS. The type I interferon (IFN) signaling pathway transcription factor, STAT1, is upregulated and phosphorylated, and transcript levels of ISG15 is increased in children with versus without PARDS. Neutrophil extracellular trap (NET) release is regulated by a NADPH oxidase (NOX) respiratory burst (reactive oxygen species (ROS) triggered mechanism and an intracellular calcium-dependent trigger. It is not known which trigger dominates in the airways of children with PARDS. Children with PARDS have elevated levels of NETs in their airways as detected by myeloperoxidase (MPO)-DNA complexes in our study. Elevated NET levels are associated with a higher number of ventilator-free days (VFD) over 20 days in a 28-day period (i.e. if the child survived, then they were more likely to spend ≥ 7 days endotracheally intubated and mechanically ventilated). Created with BioRender.com using the web version, which may be accessed at https://biorender.com/, with a paid individual subscription granting permission to publish in journals.