Abstract
Objective
Given the strong push to empower patients and make them partners in their health care, we evaluated the current capability of hospitals to offer health information technology that facilitates patient engagement (PE).
Materials and Methods
Using an ontology mapping approach, items from the American Hospital Association Information Technology Supplement were mapped to defined levels and categories within the PE Framework. Points were assigned for each health information technology function based upon the level of engagement it encompassed to create a PE-information technology (PE-IT) score. Scores were divided into tertiles, and hospital characteristics were compared across tertiles. An ordered logit model was used to estimate the effect of characteristics on the adjusted odds of being in the highest tertile of PE-IT scores.
Results
Thirty-six functions were mapped to specific levels and categories of the PE Framework, and adoption of each item ranged from 23.5 to 96.7%. Hospital characteristics associated with being in the highest tertile of PE-IT scores included medium and large bed size (relative to small), nonprofit (relative to government nonfederal), teaching hospital, system member, Midwest and South regions, and urban location.
Discussion
Hospital adoption of PE-oriented technology remains varied, suggesting that hospitals are considering how technology can create partnerships with patients. However, PE functionalities that facilitate higher levels of engagement are lacking, suggesting room for improvement.
Conclusion
While hospitals have reached modest levels of adoption of PE technologies, consistent monitoring of this capacity can identify opportunities to use technology to facilitate engagement.
Keywords: patient engagement, health information technology, patient portals, electronic health record
BACKGROUND
In response to several components of the Affordable Care Act that aim to improve overall population health, including case management, care coordination, and patient communication, health systems are seeking new ways to increase their level of patient engagement (PE). Definitions of PE vary by discipline but share a common focus on the degree to which patients actively participate in their care.1,2 More engaged patients can better advocate for themselves and more actively participate in their care, potentially increasing patient satisfaction, improving outcomes, and lowering costs, particularly for patients with chronic diseases.3 Thus, efforts to increase engagement of patients in their care have received significant attention in recent years, and evidence suggests that patients are indeed becoming more active participants in their care.4
Health systems view health information technology (HIT) as one means to improve PE, resulting in a rapid increase in the number and types of tools available to facilitate engagement. For example, patient portals, a class of electronic personal health records (PHRs), provide access to information in patients’ electronic health records (EHRs) (eg, test results), often in concert with other functions such as scheduling appointments and communicating securely with providers.5 These tools are a central component of PE, particularly for patients attempting to self-manage chronic conditions,6 because they allow patients to input and track health information. Such tools also facilitate communication between patients and providers, as well as offer patients access to consumer-friendly information about diseases.7–14 More advanced PHRs enable bidirectional communication and can further support physician-patient relationships and enhanced chronic disease self-management.11–14 The secure messaging embedded within patient portals has been found to contribute to positive results in areas including patient outcomes, disease management, and satisfaction with care in ambulatory settings.15
While both EHRs and PHRs can facilitate increased PE, these tools are not all created equal. The diversity of features that these technologies possess may play an important role in successfully influencing PE. However, it remains unclear to what extent existing HIT infrastructure in hospitals is designed to engage patients. To date, researchers have focused closely on how hospitals have adopted EHRs16–19 or PHRs20 and their impact on quality, cost, and efficiency.21–23 Prior work, however, has largely assessed adoption based on the depth and breadth of technology available, or on the ability to meet Meaningful Use (MU) Stage 1 or Stage 2 criteria. This focus alone does not fully capture the range or diversity of HIT tools available to assist health systems in engaging patients in their care, nor does it address the variety of ways that patients may be engaged.
Studies measuring PE relative to HIT face methodological challenges and have been limited. Furukawa et al. examined PE related to EHR adoption in office settings and found low levels of technology adoption for the purpose of PE.24 However, that study only used 4 measures of PE and lacked theoretical underpinnings. A study conducted by Kim et al. on HIT adoption in community health centers in California measured PE dichotomously based on only 2 factors, availability of PHR and of electronic clinical care summaries.25 While we understand the practical limitations that exist in such evaluation efforts, we sought a more holistic framework to examine HIT functionalities specific to PE.
SIGNIFICANCE
In order to assess hospitals’ ability to use HIT to engage patients using a patient-centric perspective, we applied the PE Framework (PEF) to hospital technology adoption. Our analysis highlights the strengths and weaknesses of the current level of hospital IT adoption and seeks to identify opportunities to develop technology that can better engage patients. Moreover, our approach of applying a scoring system may help spur research efforts to evaluate how well HIT infrastructure can support PE.
CONCEPTUAL MODEL
For this study, we applied the PEF originally developed in 2012 by the National eHealth Collaborative, which later merged with the Health Information Management Systems Society (see Figure 1 ).26 The PEF was created by a group of over 150 health care providers, health services researchers, and sociotechnical experts to provide guidance to health care organizations as they develop and deploy HIT aimed at involving patients in their care process, and has previously been used to evaluate patient portal applications.27,28 The framework was originally designed so that the definitions of the 5 levels of engagement activities aligned with MU standards. However, while MU provides a useful starting place, its criteria were designed to broadly incentivize adoption of HIT by hospitals and are not necessarily patient-centered. The PEF has the advantage of not only incorporating MU components, but also extending beyond MU to incorporate HIT tools that promote engagement.
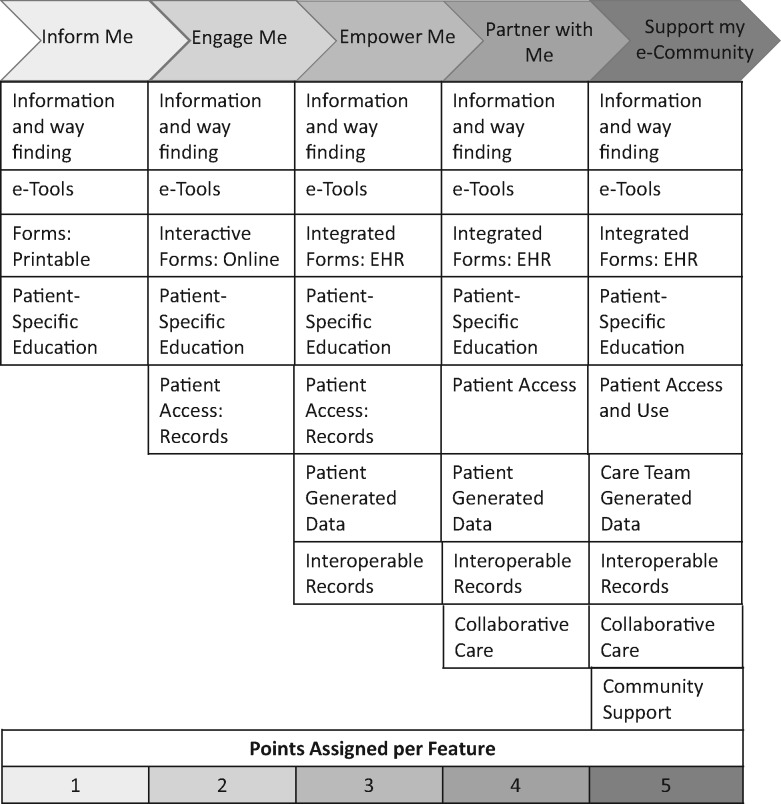
Figure 1.
Information technology functions organized by increasing level of patient engagement and corresponding scores assigned for each component. Adapted from the Patient Engagement Framework.26,27
Given its focus on how particular technological functions support healthy behaviors and communication with health care providers, the PEF organizes PE offerings into 5 increasing levels of progressively greater partnership.28 Each successive level of the PEF – (1) inform me, (2) engage me, (3) empower me, (4) partner with me, (5) support my e-community – reflects greater access to and control of patients’ information, which should facilitate greater communication and interaction with their health care providers.
The PEF has defined categories delineating tangible features that comprise each of the 5 levels of engagement (see Figure 1). This framework is cumulative in nature; offering HIT capabilities in more categories is therefore required to obtain a higher level of engagement via HIT. Importantly, the categories generally pertain to how HIT can be patient-centric rather than focus on actions patients can take or applications they use. For example, the “interoperable records,” which spans the “empower me,” “partner with me,” and “support my e-community” domains, does not explicitly entail any involvement from the patient, but rather engages the patient by enabling the data to follow him or her. As a result, the patient is at the center of the flow of information across the health care system.
METHODS
Study design
The aim of this study was to use the PEF to evaluate the current state of hospitals in the United States and their use of HIT to engage patients. To accomplish this aim, we first reviewed a published survey of information technology capabilities and mapped applicable survey items to levels and categories of the PEF. Second, we created a PE-information technology (PE-IT) score for each hospital by assigning points based on the level of engagement activities of each capability.27 Third, we used these scores to assess the characteristics of hospitals that are relatively more oriented toward PE using HIT.
Data
We employed a cross-sectional design using data from 2 matched surveys, the 2015 American Hospital Association (AHA) Annual Survey (organizational and service characteristics) and the 2015 AHA Information Technology (IT) Supplement. The AHA Annual Survey is administered to a census list of hospitals in the United States; the response rate for this survey in 2015 was 90%. The Annual Survey requests information regarding hospital organizational and service characteristics, while the IT Supplement is administered to respondents of the Annual Survey. The 2015 IT Supplement had a 63% response rate and reported information regarding the adoption and use of 161 aspects of HIT; it has been widely used to evaluate IT capacity. Hospitals achieve these capacities through 3 technologies: EHRs, health information exchange (HIE), and patient portals. We limited our analysis to acute-care general hospitals in the United States that responded to both surveys.
Patient engagement-information technology scores
Guided by ontology mapping,29,30 a team of 3 reviewers, 1 expert in the field of PE research (initials withheld for peer review) and 2 experts in the field of HIT research (initials withheld for peer review), reviewed the IT Supplement to identify survey items that mapped to specific levels and categories within the PEF. Each item was evaluated based on prior research that described the attributes of the categories and levels.27 The survey and the PEF were not developed to align with each other and, as a result, survey items did not always map directly to specific cells within the PEF. To achieve a balance between maximum inclusivity and high discrimination, we conservatively categorized items that did not clearly match to a specific level within the PEF to the lowest possible level. One survey item (“Do you currently have an electronic system to identify and provide patient generated data?”) was particularly unclear given its representation in each level of the PEF without much discrimination. For this item, we counted it in each level, thereby spreading any effects due to miscategorization equally across all hospitals. Borrowing from previous work,16,18 we also noted whether the survey item was included as an MU Stage 1 or Stage 2 criterion. For most survey items, the difference between a Stage 1 or Stage 2 criterion has to do with the breadth of adoption across a hospital. Survey items align with the Stage 1 criterion of a hospital being considered as having adopted a given technological feature if it has it in any part of the hospital, rather than the Stage 2 criterion of having the technology across the entire hospital. When possible, MU criteria or pre-existing approaches to combining items were used to combine items that might represent a single functionality.31
We borrowed our scoring approach from Geng and Myeni,27 assigning a hospital 1 to 5 points, based on increasing level of engagement, for each feature available in that hospital to generate a cumulative PE-IT score for each hospital. The distribution of this score was tested for normality using the joint skewness and kurtosis test and was found to be negatively skewed. Logarithmic, square-root, square, and inverse transformations were attempted, but each failed to normalize the score. To resolve this concern with the distribution of PE-IT scores, the scores were divided into low, medium, and high tertiles based on percentiles. As a sensitivity analysis, we also tested quartiles and quintiles and found no differences in our results, so we chose the most parsimonious division of scores.
Analysis
To determine hospital characteristics associated with an orientation toward HIT to facilitate PE, we compared hospital and market characteristics across the tertiles of PE-IT scores. Hospital characteristics included bed size, ownership type, system member, teaching status, rural/urban location, census region, and a Hirschman-Herfindahl Index calculated from bed size within each core-based statistical area. Our choice to operationalize these hospital characteristics follows commonly used approaches in the HIT literature.16,32 These characteristics were included as independent variables in a multivariate ordered logit model to evaluate the effects of hospital and market characteristics on the likelihood of a hospital being in the highest tertile of PE-IT scores.
Additionally, previous research identified differences between IT supplement responders and nonresponders. To address this source of bias, we applied inverse probability weights.33,34 This approach calculates the predicted probability of responding to the survey based on a set of hospital characteristics (bed size, ownership type, system member, teaching status, rural/urban location, census region). The inverses of these probabilities were then used as weights in all analyses. All analyses were done using Stata 14.35
RESULTS
PEF mapping
Of the 161 survey items, we identified 43 items that aligned with specific levels and categories within the PEF (see Table 1). In 4 instances, items were combined based on either MU or pre-existing scales: 3 items (computerized physician order entry [CPOE] for labs, radiology, and medications) were merged into a CPOE function based on MU criteria; 2 items (radiology imaging and diagnostic test images) were combined into an Electronic Imaging function based on MU criteria; 3 items (send summary of care through secure message, provider portal, or HIE) were combined into a Send Summary of Care Record function; and 3 items (receive summary of care through secure message, provider portal, or HIE) were combined into a single Receive Summary of Care Record function. This categorization process yielded a final total of 36 PE-related HIT functions. Fourteen of the 36 functions aligned with MU Stage 1 or 2, as either a core or menu item. Of the functions that aligned with MU (n = 12), the mean percent of adoption was 83.3%; the mean percent adoption for non-MU (n = 24) aligned functions was 51.7%. Patient-specific education was the only survey item that mapped to the “inform me” level, though this item was included in all levels due to its lack of specificity in the survey. The “empower me” level was the only level to have IT functions represented in each category.
Table 1.
Characterization of information technology function from the Patient Engagement Framework and frequency of adoption, ordered by level of engagement
| Function | PEF Level | Category | MU Requirement | % Adopted (n = 2780) |
|---|---|---|---|---|
| Patient-Specific Education | All Levels | Patient-Specific Education | Stages 1 and 2 Core | 95.5 |
| Schedule Appointments Online | Engage Me | Interactive Forms | NA | 46.7 |
| Pay Bills | Engage Me | Interactive Forms | NA | 76.8 |
| Request Prescription Refill | Engage Me | Interactive Forms | NA | 46.4 |
| View Record | Engage Me | Patient Access | Stages 1 and 2 Core | 96.7 |
| Download Record | Engage Me | Patient Access | Stages 1 and 2 core | 89.0 |
| Provider Performance Profile | Empower Me | Quality | NA | 61.5 |
| Hospital Quality Measures | Empower Me | Quality | MU Stage 1 | 89.2 |
| Physician-Specific Quality Measures | Empower Me | Quality | MU Stage 1 | 78.6 |
| Secure Messaging | Empower Me | e-Tools | NA | 66.2 |
| Advanced Directives (e-Documentation) | Empower Me | Integrated Forms | Stage 2 Menu | 85.8 |
| Request Change to Record | Empower Me | Integrated Forms | NA | 79.6 |
| Transmit Record | Empower Me | Patient Access | Stages 1 and 2 Core | 74.2 |
| Designate Family/Caregiver Access | Empower Me | Patient Access | NA | 84.8 |
| Submit Patient-Generated Data | Empower Me and Partner w/ Me | Patient-Generated Data | NA | 39.5 |
| Electronic Images | Empower Me | Interoperable Records | Stage 2 Menu | 78.8 |
| CPOE for Labs, Radiology, Medications | Empower Me | Interoperable Records | Stages 1 and 2 Core | 96.5 |
| Find (Query) Information from Outside System | Empower Me | Interoperable Records | NA | 54.9 |
| Send Summary of Care Record | Empower Me | Interoperable Records | Stages 1 and 2 Core | 85.5 |
| Receive Summary of Care Record | Empower Me | Interoperable Records | Stages 1 and 2 Core | 64.7 |
| Integrate Information from Outside System | Empower Me | Interoperable Records | NA | 24.5 |
| Health Information Exchange | Empower Me | Interoperable Records | NA | 64.1 |
| Send Information to Hospitals Outside Of System | Empower Me | Interoperable Records | NA | 60.5 |
| Send Information to Ambulatory Outside Of System | Empower Me | Interoperable Records | NA | 62.4 |
| Receive Information from Hospitals Outside Of System | Empower Me | Interoperable Records | NA | 41.5 |
| Receive Information from Ambulatory Outside of System | Empower Me | Interoperable Records | NA | 38.3 |
| Identify High Risk Patients | Partner w/Me | Analytics/ Quality | NA | 55.1 |
| Immunization Registries | Partner w/Me | Interoperable Records | Stages 1 and 2 core | 91.0 |
| Reportable Lab Results | Partner w/Me | Interoperable Records | Stages 1 and 2 core | 86.1 |
| Syndromic Surveillance | Partner w/ Me | Interoperable Records | Stages 1 and 2 core | 83.4 |
| Primary Care Notification | Partner w/Me | Collaborative Care | NA | 61.3 |
| Adherence to Clinical Guidelines | Support My e-Community | Care Team Generated Data | NA | 54.2 |
| Send Information to Long-term/Post-Acute Inside or Outside of System | Support My e-Community | Interoperable Records | NA | 50.6 |
| Send Information to Behavioral Health Inside or Outside of System | Support My e-Community | Interoperable Records | NA | 36.5 |
| Receive Information from Long-Term/Post-Acute Inside or Outside of System | Support My e-Community | Interoperable Records | NA | 23.8 |
| Receive Information from Behavioral Health Inside or Outside of System | Support My e-Community | Interoperable Records | NA | 23.5 |
Notes: PEF: Patient Engagement Framework; MU: Meaningful Use; NA: not applicable; her: electronic health record.
Evaluation of PE-IT scores
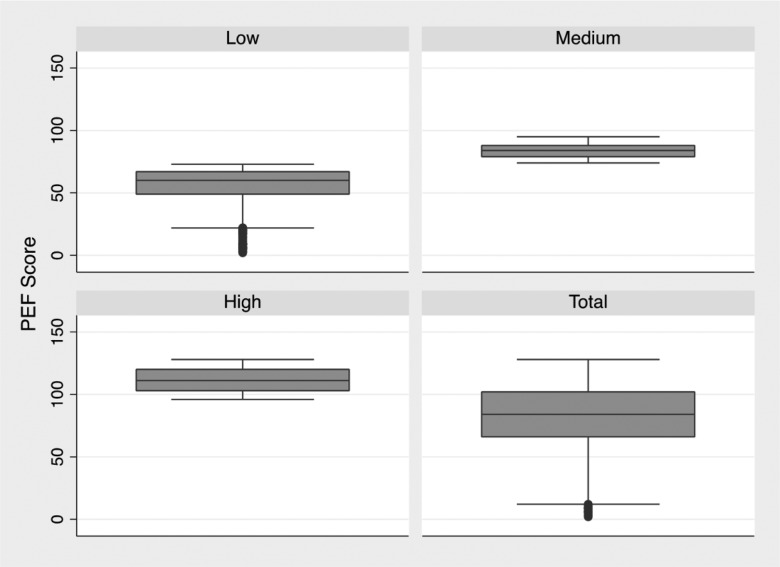
For the 2780 nonfederal acute-care hospitals that responded to both surveys, points were assigned for each IT component according to level of engagement, with a maximum possible score of 128 points. Scores were then divided into tertiles. The distribution of the tertiles and overall scores are presented in Figure 2 . Hospital characteristics for the overall sample as well as within each tertile of PE-IT score are presented in Table 2. Hospitals in the high tertile were disproportionately large, nonprofit, system members, teaching institutions, located in the Midwest, and located in urban areas, relative to hospitals in the low and medium tertiles.
Figure 2.
Box plot of each tertile of the Patient Engagement-Information Technology scores and the full sample.
Table 2.
Hospital characteristics based on tertile of PE-IT score derived from the Patient Engagement Framework
| Hospital Characteristic | PE-IT Score Tertile |
Total | ||
|---|---|---|---|---|
| Low (n = 955) (%) | Medium (n = 921) (%) | High (n = 904) (%) | Overall (n = 2780) (%) | |
| PE-IT Score (mean ± SE) | 55.1 ± 0.51 | 83.9 ± 0.19 | 111.6 ± 0.32 | 83.0 ± 0.49 |
| Bed Size | ||||
| Small (<99) | 60.9 | 42.5 | 32.5 | 45.6 |
| Medium (100–399) | 34.0 | 45.1 | 46.2 | 41.6 |
| Large (>400) | 5.03 | 12.4 | 21.2 | 12.7 |
| Ownership | ||||
| Government nonfederal | 33.4 | 19.9 | 12.9 | 22.3 |
| Nonprofit | 50.6 | 61.2 | 84.3 | 65.1 |
| For-profit | 16.0 | 18.8 | 2.8 | 12.6 |
| Teaching Status | 1.99 | 4.56 | 14.7 | 6.98 |
| System Member | 47.4 | 63.6 | 80.8 | 63.7 |
| Region | ||||
| Northeast | 11.3 | 14.8 | 12.7 | 12.9 |
| Midwest | 21.1 | 36.0 | 39.0 | 31.9 |
| South | 44.8 | 33.3 | 32.6 | 37.0 |
| West | 22.6 | 15.8 | 15.6 | 18.1 |
| Urban | 64.0 | 80.9 | 88.2 | 77.6 |
| HHI (mean ± SE) | 0.14 + 0.003 | 0.14 + 0.003 | 0.13 + 0.004 | 0.14 + 0.002 |
Note: PE-IT: patient engagement-information technology; SE: standard error; HHI: Hirschman-Herfindahl Index.
To determine the hospital and market characteristics associated with the greatest PE-IT scores, we estimated an adjusted ordered logit model to evaluate the odds of being in the high tertile (see Table 3). Our results from the adjusted model revealed that medium (odds ratio [OR]: 1.33; 95% Confidence Interval [CI] 1.11–1.61) and large (OR: 1.89, 95% CI 1.43–2.51) hospitals have the highest likelihood of being in the high tertile of PE-IT scores, as well as nonprofit (OR: 1.75; 95% CI 1.43–2.14) hospitals relative to government nonfederal hospitals. Conversely, for-profit hospitals have a lower likelihood of being in the highest tertile (OR: 0.39; 95% CI 0.30–0.51). Additionally, teaching institutions (OR: 2.67; 95% CI 1.81–3.93), system members (OR: 2.66; 95% CI 2.25–3.15), Midwestern (OR: 1.96; 95% CI 1.55–2.48), Southern (OR: 1.46; 95% CI 1.14–1.86), and urban hospitals (OR: 1.87; 95% CI 1.51–2.32) all had greater adjusted odds of being in the highest tertile of PE-IT scores.
Table 3.
Organizational factors associated with high levels of patient engagement–focused health information technology
| Hospital Characteristic | High PE-ITa |
|---|---|
| Bed Size | |
| Small (<99) | Ref. |
| Medium (100–399) | 1.33 (1.11–1.61)** |
| Large (>400) | 1.89 (1.43–2.51)*** |
| Ownership | |
| Government nonfederal | Ref. |
| Nonprofit | 1.75 (1.43–2.14)*** |
| For-profit | 0.39 (0.30–0.51)*** |
| Teaching Status | 2.67 (1.81–3.93)*** |
| System Member | 2.66 (2.25–3.15)*** |
| Region | |
| Northeast | Ref. |
| Midwest | 1.96 (1.55–2.48)*** |
| South | 1.46 (1.14–1.86)** |
| West | 1.08 (0.83–1.42) |
| Urban | 1.87 (1.51–2.32)*** |
| HHI | 0.73 (0.37–1.44) |
Note: ***P < .001; **P < .01; *P < .05.
aOdds ratios of being in the highest tertile of patient engagement-information technology scores, relative to the low and medium tertiles. IT: information technology; HHI: Hirschman-Herfindahl Index.
DISCUSSION
The ongoing interest in fostering PE has been met with a challenge to identify how to best achieve this goal. Meanwhile, the rapid adoption of HIT has presented an opportunity to utilize this technology as a means to engage patients. Indeed, recent evidence suggests that a variety of HIT components can serve this goal and enable patients to better access their health records and communicate with their providers, thereby allowing them to become better partners in their care. This study evaluated the current ability of hospitals to use HIT toward this goal of engaging patients and identify opportunities to develop technologies that facilitate this connection between patients and their providers.
One of our primary study goals was to apply a more refined measure of PE-related HIT than existing research in order to better evaluate how technology is being used to promote patient-centered care. In this respect, our approach to identifying PE-related HIT functions and scoring them based on the PEF represents a significant step forward in terms of the breadth of HIT functions considered related to PE. The results of our study offer an in-depth description of the current state of PE activities related to HIT functionality offered by health systems, and present a benchmark against which organizations can compare and a scoring approach that can be applied in future research.
A unique feature of the PEF is that it encompasses the availability of both patient- and provider-related HIT functions. Many HIT functions available to patients through a patient portal or PHR, such as secure messaging, require physician activity in addition to PE in order to fully realize their potential. Still other functions make the care experience more patient-centered, but in fact are completely dependent on physician engagement with the technology, such as CPOE. Thus, physician engagement with patient-centered HIT and dedication to patient-centeredness is at the crux of increased adoption and use of HIT for purposes of enhanced PE.
Yet while physician engagement with patient-centered HIT is critical, financial, technical, and political barriers exists that may limit physicians’ interaction with the technology.36 Further, physicians may have low expectations around the benefits of engaging patients in their health care through technology, and may actually see the technology as creating problems.37 As physician support for PE-related HIT is necessary to realize the potential benefits of the technology moving forward, how to support this engagement remains an important area for future research. Our approach of categorizing HIT functionalities within an engagement framework provides a useful means by which systems can assess their ability to encourage engagement via HIT.
Our findings suggest room for improvement in how hospitals design HIT to facilitate PE by identifying engagement categories for which only limited HIT features exist. For example, HIT functions for each category of the “empower me” level were identified, while functions in only 2 of the 9 categories were identified for the “support my e-community” level. Hospitals are slowly moving in this direction, for example, by adopting patient portals designed for the inpatient environment that connect with ambulatory portals.38 These systems offer greater opportunity across the care continuum to deploy several features that may increase the patient orientation of technology, such as secure messaging, e-visits, or access to shared care plans. Still, more effort can be made to increase interoperability at all points of care, such as with chiropractors, dentists, or home health providers. Incorporating more elements of the health care system into the ecosystem of digital records will serve to put patients at the center of the system as their data follow them across the care continuum.
Establishing robust health information exchanges offers one approach to increasing interoperability and providing several features of a patient portal.39 The interoperability inherent in this approach can support PE by providing greater access and sharing of information. However, there has been limited success of widespread participation in HIEs, particular in non–acute-care settings.18 While new approaches to HIE are emerging, such as vendor-mediated models, these have limited appeal to collaborative care providers that operate on limited budgets.40 As a result, these approaches to increasing interoperability may limit the patient-centeredness of HIT. Nonetheless, as the link between quality measures and reimbursement (eg, accountable care organizations) becomes more common in the health care environment, we could realize results indirectly by encouraging the organic expansion of PE HIT functionalities to meet quality goals.41
Moreover, while interoperability among health care providers is necessary, it is insufficient to orient the health care system more toward patient-centered deployment of HIT. Greater patient access and control of health records are also needed. The Veterans Affairs Blue Button technology is an example of how offering patients access to their health records can improve the movement of information across the health care system and empower patients with greater control.42,43 Other HIT systems can also give patients the ability to control who sees certain parts of their health record.44 These approaches augment exchange networks by giving patients greater control and access to their digital records and enabling them to be at the center of the flow of information.
In addition to interoperability, our results regarding hospital characteristics associated with higher PE-IT scores corroborate earlier studies reporting that small non-system members and non-teaching and rural hospitals are falling behind in their adoption of HIT in general.16,33 Not only are these hospitals falling behind with regard to their own operational abilities, but they also appear to lack the capacity to engage their patient population via HIT. This combination could increase existing disparities in the care these institutions offer to underserved populations and is an important issue to monitor.
Limitations
This study has inherent limitations of scope, given the data sources used. First, the granularity in the survey might limit our ability to accurately map survey items to the PEF. For example, advanced health directives was categorized as an integrated form under “empower me,” given that the AHA IT Supplement asks whether the hospital has electronic clinical documentation of advanced directives. However, the survey cannot be refined to the level of whether this feature includes advanced care planning, a functionality that should be characterized under “partner with me.” We chose to conservatively characterize the various HIT functions to limit the effect of data granularity, but nonetheless this remains a concern.
Related to this issue, our ability to calculate a PE-IT score was limited to the items present in the survey. The AHA IT Supplement was not designed according to the PEF, and as a result it does not explicitly ask about items in each level/category of the framework. This discordance limits the maximum possible score a hospital can receive to what is known based on the survey, not on what is possible. Furthermore, calculating an ideal maximum score based on each level/category listed in the PEF is not possible, given the breadth of available technologies that could fit into the framework. Thus, our PE-IT scores should be interpreted as relativistic rather than idealistic.
In addition, our study does not assess the impact of PE-IT scores on PE itself. Current evidence supports the concept that these technological tools can indeed engage patients, and we rely on the PEF framework to delineate types and levels of engagement capabilities. Still, without proper testing, this relationship remains unvalidated; rectifying this limitation would require PE assessments across a national sample of hospitals, a task requiring significant resources. Finally, while strong theoretical work45 and early evaluations have identified ways that HIT can improve PE, more research is needed to optimize the mechanisms by which new technologies can transform patient care. Nonetheless, our approach helps to identify gaps in the current available HIT infrastructure oriented toward PE and corresponding opportunities to improve current data collection instruments.
Conclusion
Our intention in grounding our study in the PEF was threefold: to describe engagement activities that extend beyond the functions of a patient portal alone, including care team activities and community support; to apply a framework that hospitals can use to assess their specific activities related to PE; and to propose a means to advance HIT’s ability to contribute to PE efforts. Our findings regarding hospitals’ HIT orientation toward PE showed wide variation in their adoption of the technology features identified as contributing to PE, suggesting that hospitals are likely not ignoring PE as they invest in new innovative tools to provide health care. However, room for improvement exists, particularly with regard to technologies that facilitate higher levels of engagement. PE has great potential to tip the scale for health care and contribute to improved cost and quality, and HIT provides a platform to empower patients. Continued assessment of hospitals’ ability to utilize these technologies is necessary to identify opportunities to develop new technologies that foster partnerships with patients.
FUNDING
No funding was received for this work.
COMPETING INTERESTS
The authors report no competing interests related to this work.
ACKNOWLEDGMENTS
The authors would like to thank Alison Aldrich for her assistance in preparing the literature review for this manuscript.
References
- 1. Barello S, Triberti S, Graffigna G. et al. eHealth for patient engagement: a systematic review. Front Psychol. 2015;6:2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Carman KL, Dardess P, Maurer M. et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff (Millwood). 2013;322:223–31. [DOI] [PubMed] [Google Scholar]
- 3. Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012;275:520–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Menichetti J, Libreri C, Lozza E, Graffigna G. Giving patients a starring role in their own care: a bibliometric analysis of the on-going literature debate. Health Expect. 2016;193:516–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wald JS, Middleton B, Bloom A. et al. A patient-controlled journal for an electronic medical record: issues and challenges. Stud Health Technol Inform. 2004;107(Pt 2):1166–70. [PubMed] [Google Scholar]
- 6. Snyder CF, Wu AW, Miller RS, Jensen RE, Bantug ET, Wolff AC. The role of informatics in promoting patient-centered care. Cancer J (Sudbury, Mass.). 2011;174:211–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Emont S. Measuring the Impact of Patient Portals: What the Literature Tells Us. Oakland, CA: California HealthCare Foundation; 2011. [Google Scholar]
- 8. Halamka JD, Mandl KD, Tang PC. Early experiences with personal health records. J Am Med Inform Assoc. 2008;151:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hess R, Bryce CL, Paone S. et al. Exploring challenges and potentials of personal health records in diabetes self-management: implementation and initial assessment. Telemed J E-Health. 2007;135:509–17. [DOI] [PubMed] [Google Scholar]
- 10. Kaelber D, Pan EC. The value of personal health record (PHR) systems. AMIA Annual Symposium Proceedings/AMIA Symposium. 2008;2008:343–47. [PMC free article] [PubMed] [Google Scholar]
- 11. Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. New Engl J Med. 2010;3636:501–04. [DOI] [PubMed] [Google Scholar]
- 12. Murphy J. Patient as center of the health care universe: a closer look at patient-centered care. Nurs Econ. 2011;291:35–37. [PubMed] [Google Scholar]
- 13. Nelson JA. Personal Health Records. Home Healthcare Manag Pract. 2009;212:141–42. [Google Scholar]
- 14. Wilson ML, Murphy LS, Newhouse RP. Patients’ access to their health information: a meaningful-use mandate. J Nursing Admin. 2012;4211:493–96. [DOI] [PubMed] [Google Scholar]
- 15. Osborn CY, Mayberry LS, Mulvaney SA, Hess R. Patient web portals to improve diabetes outcomes: a systematic review. Curr Diabetes Reports. 2010;106:422–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Adler-Milstein J, DesRoches CM, Kralovec P. et al. Electronic health record adoption In US hospitals: progress continues, but challenges persist. Health Aff (Millwood). 2015;3412:2174–80. [DOI] [PubMed] [Google Scholar]
- 17. Mennemeyer ST, Menachemi N, Rahurkar S, Ford EW. Impact of the HITECH Act on physicians’ adoption of electronic health records. J Am Med Inform Assoc. 2016;232:375–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Walker D, Mora A, Demosthenidy MM, Menachemi N, Diana ML. Meaningful use of EHRs among hospitals ineligible for incentives lags behind that of other hospitals, 2009–13. Health Aff (Millwood). 2016;353:495–501. [DOI] [PubMed] [Google Scholar]
- 19. Walker DM, Diana ML. Hospital adoption of health information technology to support public health infrastructure. J Public Health Manag Pract. 2016;222:175–81. [DOI] [PubMed] [Google Scholar]
- 20. Ford EW, Hesse BW, Huerta TR. Personal health record use in the United States: forecasting future adoption levels. J Med Internet Res. 2016;183:e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rudin RS, Motala A, Goldzweig CL, Shekelle PG. Usage and effect of health information exchange: a systematic review. Ann Intern Med. 2014;16111:803–11. [DOI] [PubMed] [Google Scholar]
- 22. Rahurkar S, Vest JR, Menachemi N. Despite the spread of health information exchange, there is little evidence of its impact on cost, use, and quality of care. Health Aff (Millwood). 2015;343:477–83. [DOI] [PubMed] [Google Scholar]
- 23. Appari A, Johnson ME, Anthony DL. Meaningful use of electronic health record systems and process quality of care: Evidence from a panel data analysis of U.S. acute-care hospitals. Health Services Research. 2013;482:354–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Furukawa MF, King J, Patel V, Hsiao CJ, Adler-Milstein J, Jha AK. Despite substantial progress in EHR adoption, health information exchange and patient engagement remain low in office settings. Health Aff (Millwood). 2014;339:1672–79. [DOI] [PubMed] [Google Scholar]
- 25. Kim KK, Rudin RS, Wilson MD. Health information technology adoption in California community health centers. Am J Manag Care. 2015;2112:e677–83. [PMC free article] [PubMed] [Google Scholar]
- 26. HIMSS Foundation, National eHealth Collaborative. Patient Engagement Framework. Secondary Patient Engagement Framework. 2014. http://www.himss.org/himss-patient-engagement-framework. Accessed April 4, 2016.
- 27. Geng Y, Myneni S. Patient engagement in cancer survivorship care through mHealth: a consumer-centered review of existing mobile applications. AMIA Annu Symp Proc. 2015;2015:580–88. [PMC free article] [PubMed] [Google Scholar]
- 28. Shapiro-Mathews E, Barton AJ. Using the patient engagement framework to develop an institutional mobile health strategy. Clin Nurse Spec. 2013;275:221–23. [DOI] [PubMed] [Google Scholar]
- 29. Ding Y, Foo S. Ontology research and development. Part 2: a review of ontology mapping and evolving. J Inform Sci. 2002;285:375–88. [Google Scholar]
- 30. Ding Y, Foo S. Ontology research and development. Part 1: a review of ontology generation. J Inform Sci. 2002;282:123–36. [Google Scholar]
- 31. Holmgren AJ, Patel V, Charles D, Adler-Milstein J. US hospital engagement in core domains of interoperability. Am J Manag Care. 2016;2212:e395–402. [PubMed] [Google Scholar]
- 32. Jha AK, DesRoches CM, Campbell EG. et al. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;36016:1628–38. [DOI] [PubMed] [Google Scholar]
- 33. DesRoches CM, Worzala C, Joshi MS, Kralovec PD, Jha AK. Small, nonteaching, and rural hospitals continue to be slow in adopting electronic health record systems. Health Aff (Millwood). 2012;315:1092–99. [DOI] [PubMed] [Google Scholar]
- 34. Wooldridge JM. Inverse probability weighted estimation for general missing data problems. J Econometrics. 2007;141:1281–301. [Google Scholar]
- 35. Stata Statistical Software: Release 14 [program]. College Station, TX: StataCorp; 2015. [Google Scholar]
- 36. Gold M, Hossain M, Mangum A. Consumer engagement in health IT: distinguishing rhetoric from reality. EGEMS (Wash DC). 2015;31:1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Archer N, Fevrier-Thomas U, Lokker C, McKibbon KA, Straus SE. Personal health records: a scoping review. J Am Med Inform Assoc. 2011;184:515–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. McAlearney AS, Sieck CJ, Hefner JL. et al. High Touch and High Tech (HT2) Proposal: transforming patient engagement throughout the continuum of care by engaging patients with portal technology at the bedside. JMIR Res Protoc. 2016;54:e221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Otte-Trojel T, de Bont A, van de Klundert J, Rundall TG. Characteristics of patient portals developed in the context of health information exchanges: early policy effects of incentives in the meaningful use program in the United States. J Med Internet Res. 2014;1611:e258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Vest JR, Kash BA. Differing strategies to meet information-sharing needs: publicly supported community health information exchanges versus health systems’ enterprise health information exchanges. Milbank Q. 2016;941:77–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Walker DM, Mora AM, Scheck McAlearney A. Accountable care organization hospitals differ in health IT capabilities. Am J Manag Care. 2016;2212:802–07. [PubMed] [Google Scholar]
- 42. Klein DM, Fix GM, Hogan TP, Simon SR, Nazi KM, Turvey CL. Use of the Blue Button online tool for sharing health information: qualitative interviews with patients and providers. J Med Internet Res. 2015;178:e199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Turvey C, Klein D, Fix G. et al. Blue Button use by patients to access and share health record information using the Department of Veterans Affairs’ online patient portal. J Am Med Inform Assoc. 2014;214:657–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Li M, Yu S, Ren K, Lou W, editors. Securing personal health records in cloud computing: Patient-centric and fine-grained data access control in multi-owner settings. International Conference on Security and Privacy in Communication Systems. Springer; 2010. [Google Scholar]
- 45. Otte-Trojel T, de Bont A, Rundall TG, van de Klundert J. How outcomes are achieved through patient portals: a realist review. J Am Med Inform Assoc. 2014;214:751–57. [DOI] [PMC free article] [PubMed] [Google Scholar]