Abstract
Objectives
The incidence of cardiovascular diseases is increasing and there is a growing need to provide access to quality cardio drugs in Africa. In the SEVEN study, we analysed 1530 cardiovascular drug samples randomly collected from 10 African countries. By that time, of the seven drugs products analysed, only those containing amlodipine and captopril had very low assay values with active substance contents that could be less than 75% of those expected. In this article we investigate complementary aspects of the amlodipine and captopril samples so to explain the previously observed low assays for these two drugs.
Design
Post hoc analysis of the captopril and amlodipine drugs samples and their packages collected in the context of the SEVEN study.
Setting
10 countries were concerned: Benin, Burkina Faso, Congo, Democratic Republic of the Congo, Guinea, Côte d’Ivoire, Mauritania, Niger, Senegal and Togo.
Participants
Local scientists and hospital practitioners collected the drug samples in the 10 African countries.
Outcome measures
The drug amount and the relative amounts of drug impurities, as well as the main compounds of the drugs packaging, were analysed.
Results
Identification of the blister packaging of the samples led to separate both amlodipine and captopril drug samples in two groups. Mann Whitney’s bilateral test showed a significant difference (p<0.0001) between the median value of the captopril dosage when tablets are packaged in blisters providing higher protection to humidity (n=105) as opposed to the tablets packaged in blisters providing lower humidity protection (n=130).
Conclusion
Based on these results, particular attention should be paid to the materials and types of packaging used in order to minimise the lack of control over the exposures and drug circuits present in these different countries.
Keywords: quality in health care, public health, toxicity, cardiology
Strengths and limitations of this study.
Captopril-based and amlodipine-based drug samples were randomly collected in licensed and unlicensed places of sale in Africa to be analysed.
The countries involved in this study were Benin, Burkina Faso, Congo, Democratic Republic of the Congo, Guinea, Côte d’Ivoire, Mauritania, Niger, Senegal and Togo.
Assay and impurity profile were performed for quality and stability assessment considering, where applicable, the type of primary packaging used.
Introduction
Substandard drugs generally pose a serious health concern from several perspectives and this is particularly prevalent in developing countries where control regulations are poorly developed. Numerous cases of quality defects have been reported,1 2 mostly in connection with anti-infective drugs.3 However, since cardiovascular diseases are currently the most important non-communicable diseases in most low- and middle-income countries, it is critical to ensure that these diseases are addressed in a comprehensive manner.4 Thus, under the initiative of X. Jouven, the study named SEVEN has been set up with the aim of evaluating the quality of the cardiovascular drugs present in 10 African countries,5–7 by exploring the case of seven commonly used cardiac drugs, namely acenocoumarol, simvastatin, furosemide, hydrochlorothiazide, captopril, atenolol and amlodipine. It was showed that branded drugs were less likely to be of poor quality compared with generic or medicines with unknown version (p<0.001); conversely place of sale was not significantly associated with the proportion of poor quality (p=0.29).6 Examination of the identity and assay of the active substances in the various samples collected revealed that among the products tested, only those based on amlodipine and captopril had very low active substance content that could be less than 75% of those expected.6 The observation that the biggest quality defects were highlighted and circumscribed around these two molecules motivated the team to search for additional information in particular regarding their stability.
For drugs where the quality defect is unintentional, according to Johnston and Holt, low dosage levels of active substance may be the result of a variety of factors, including inadequate package design or quality.2 Yet, despite the fact that the influence of packaging changes on the stability of medicinal products is now well established,8 9 to the best of our knowledge, the studies of the quality of real field samples have so far focused only on dosage units without taking into account the type of packaging used or their chemical composition.3 However, the concept of packaging is equally important to assess, especially since the drug products need to be kept stable in difficult climatic conditions, where, for example, residual moisture can reach 88% in sub-Saharan Africa10 and the ability of a plastic blister pack to protect a drug from moisture is highly dependent on its design and composition.11
It is in this context that this study was taking place considering samples of captopril and amlodipine products, collected as part of the SEVEN study,5–7 as tracer products. On these various samples was carried out the search for degradation products and/or chromatographic-related substances as well as the identification of the packaging actually present on the products collected in several African countries, by trying, where possible and relevant, to reconcile the different data and make them meaningful in relation to the potential causes of underdosing previously highlighted for these two drugs.
Materials and methods
Sample collection
The methodology and design of the samples collection are described in detail in the articles published in the context of the SEVEN study.5–7 A multidisciplinary collaborative team of epidemiologists, cardiologists and pharmacists from France and Africa conceived and designed the study. It was registered with the French national drug agency (Agence Nationale Sécurité du Médicament ID_RCB:2014-A01275-42).
1530 drugs samples, including 235 captopril and 305 amlodipine drug samples, were collected as per the Guidelines for Field Surveys of the Quality of Medicines.12 10 countries were concerned: Benin, Burkina Faso, Congo, Democratic Republic of the Congo, Guinea, Côte d’Ivoire, Mauritania, Niger, Senegal and Togo. In these countries, samples were obtained from licensed (pharmacy) sources selected randomly and unlicensed (street market) places of sale chosen as per the local investigator’s convenience. Drug samples were purchased in the capital city and when possible in one city located close to the country’s border. Medicines were obtained by the study investigator’s staff who posed as customers. The pharmacies were randomly chosen from a list provided by the Council of the Order of Pharmacists of each country. Unlicensed markets were identified based on the local investigator’s knowledge. For each drug sample, investigators were asked to collect generic versions and brand name versions of the drug if available. After purchase, all drugs were stored at ambient temperature, in a dry place avoiding direct sunlight. Samples were sent via courier to the coordinating centre in France.
Reagents and sample preparation
Amlodipine besylate, captopril, iodine, sodium thiosulfate and triethylamine (>99% pure) were purchased from Sigma Aldrich (St. Quentin Fallavier, France). Analytical grade acetonitrile and methanol came from VWR Prolabo Chemicals (Fontenay-sous-Bois, France). Ultrapure water was produced by the Q-Pod Milli-Q system (Millipore, Molsheim, France). The stationary phase consisted of a Kinetex (Phenomenex, Torrance, USA) C18 column (4.6 mm×250 mm, i.d., 5 µm).
Standard solutions were prepared as per the recommendations provided in the United States Pharmacopoeia (USP) monograph of amlodipine besylate and captopril tablets. Captopril disulfide was obtained by using the protocol proposed in the European Pharmacopoeia (Ph. Eur.) monograph of captopril.
Analytical conditions
Chemical analyses of samples were achieved by the Department of Laboratories in Paris (AGEPS, AP-HP). Chromatographic analyses were performed using a Dionex Ultimate 3000 system (DIONEX, Ulis, France) coupled with a diode array detector. Chromatographic conditions as well as suitability tests were performed as per the recommendations provided in the monograph of amlodipine tablet (USP) and captopril (Ph. Eur.).
Identification of blisters was achieved using Fourier transformed infrared spectroscopy (FTIR), FTIR Perkin-Elmer Spectrum 2000 spectrometer (Villebon-sur-Yvette, France) with a diamond crystal. Resolution, scan range and number of accumulated scans per spectrum were set to 0.5 cm−1, 4000–400 cm−1 and 3, respectively. Spectrum were acquired on each side of the blisters using attenuated total reflectance mode.
Statistical analysis
All statistical tests were performed using GraphPad Prism V.8.3.1. for Windows (GraphPad Software, La Jolla, California, USA). Non-parametric Spearman’s correlation coefficient (r) was calculated to measure the strength of the association between the peak surface area of captopril and that of captopril disulfide. Mann-Whitney tests were used to compare the median between drugs with lower and those with higher protection from humidity packaging blisters.
Results
Collected drug samples
A total of 305 amlodipine and 235 captopril drug samples were collected in the 10 countries. The amount of drug samples collected as a function of the countries and their place of purchase is summarised in table 1. Overall, 150 of the 305 amlodipine and 140 of the 235 captopril drug samples considered in the study were obtained from licensed places of sale (table 1). In total, 265 and 195 drug samples were, respectively, identified as amlodipine and captopril generic drugs.
Table 1.
Number of collected amlodipine and captopril drug samples as a function of country and place of purchase (ie, licensed or unlicensed)
| Amlodipine | Captopril | |||||
| Licensed | Unlicensed | Total | Licensed | Unlicensed | Total | |
| Benin | 20 | 30 | 50 | 20 | 30 | 50 |
| Burkina Faso | 10 | NA | 10 | 20 | NA | 20 |
| Congo-Brassaville | NA | 30 | 30 | 10 | 10 | 20 |
| Côte d'Ivoire | 30 | 45 | 75 | 30 | 15 | 45 |
| DRC | 20 | NA | 20 | 10 | NA | 10 |
| Guinea | NA | 10 | 10 | NA | 10 | 10 |
| Mauritania | 20 | 20 | 40 | 30 | NA | 30 |
| Niger | 30 | NA | 30 | NA | 10 | 10 |
| Senegal | NA | 20 | 20 | NA | 20 | 20 |
| Togo | 20 | NA | 20 | 20 | NA | 20 |
| Total | 150 | 155 | 305 | 140 | 95 | 235 |
DRC, Democratic Republic of the Congo; NA, not applicable.
Chromatographic purity profiles of the drugs
Captopril samples
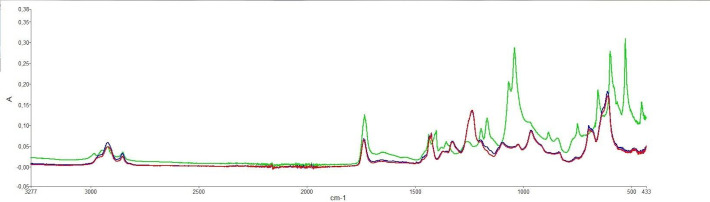
The qualitative study of the chromatograms of the 235 captopril drug samples showed that the 31 samples with drug amounts inferior to 90% (w/w) contained the same impurity (figure 1). The detected impurity was assigned to captopril disulfide as it had the same retention time than this compound.
Figure 1.
Typical chromatographic profiles of captopril solutions: reference active substance standard solution (black), typical substandard drug sample (blue).
Further, for every chromatogram, the sum of the surface of the peak areas corresponding to captopril and that of captopril disulfide led to obtain areas recoveries between 90% and 110% compared with that of the captopril reference solution. Therefore, one could infer that the lack of drug captopril may be linked to the presence of captopril disulfide. As a result, a correlation study between the surface of the peak of captopril and that of captopril disulfide impurity was carried out and yielded a negative Spearman coefficient with a value of −0.613 (p=0.0069).
Amlodipine samples
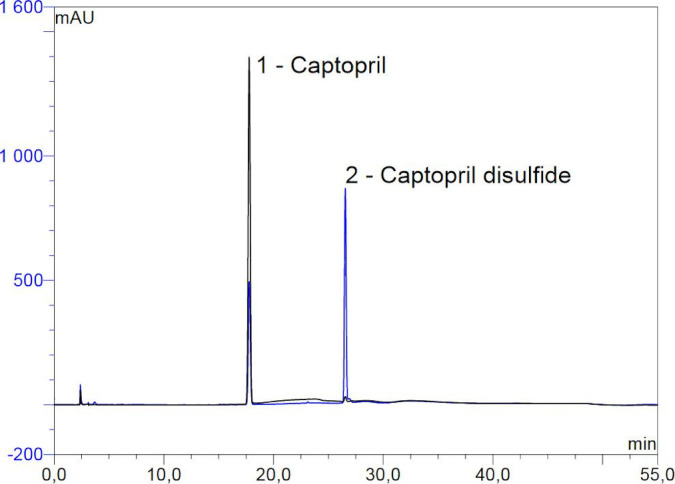
Unlike captopril, the 305 chromatographic profiles obtained for amlodipine samples strongly differed from one to the other, implying that the drugs did not contain the same impurities (figure 2). Indeed, under the analytical conditions recommended in the USP monograph, two categories of chromatographic profiles were obtained as a function of the studied samples.
Figure 2.
Typical chromatographic profiles for samples containing impurity A (A) and samples containing amlodipine-lactose interaction product (B).
A first category of chromatographic profiles consisted of samples containing an impurity with a relative retention time of about 0.5 (figure 2A) as compared with amlodipine, referred in the USP as amlodipine related compound A. In 10 chromatograms, the surface of the peak of this impurity exceeded the USP acceptance criteria for this impurity (<1.0%, w/w).
The second category of chromatographic profiles comprised a peak with a relative retention time of about 0.8 (figure 2B) corresponding to a degradation related impurity, namely an amlodipine-lactose interaction product. For 30 sample solutions, the area of the peak of this impurity compared with that of amlodipine exceeded the USP acceptance criteria for this impurity (<0.5%, w/w).
Blisters identification
The identity and aspect of the blisters materials strongly differed between amlodipine and captopril and within drug samples of the same drug.
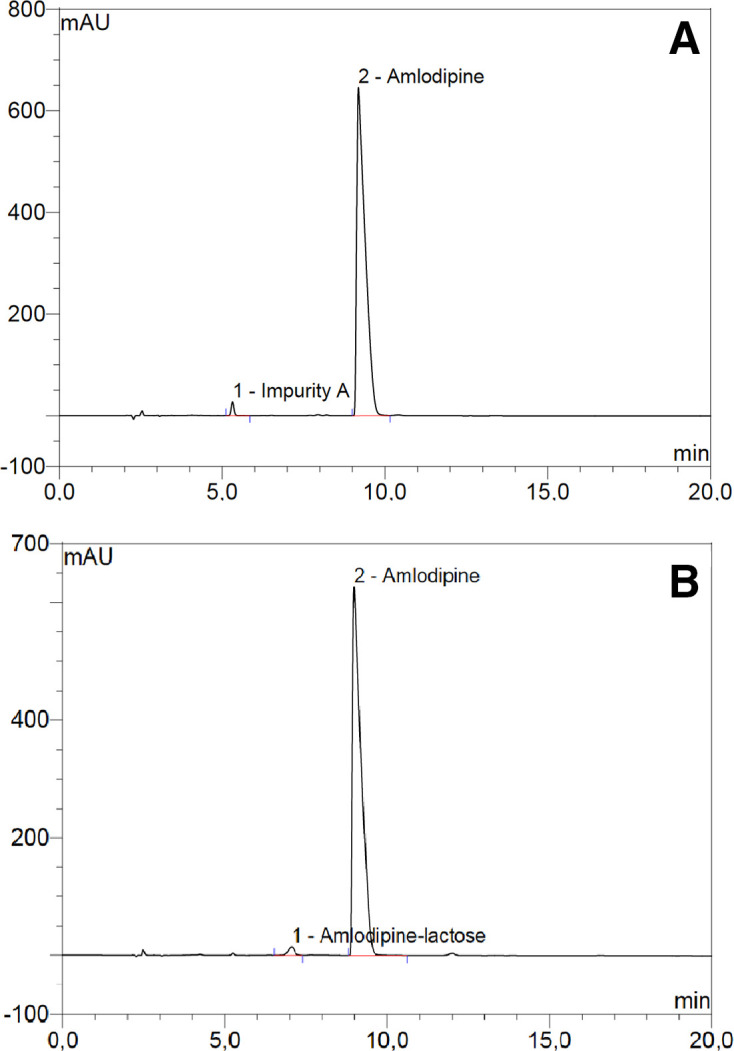
FTIR analysis were performed on each side of the plastic blisters in order to identify its main compounds. Based on the analysis, two groups could be established: those with a spectrum corresponding to polyvinyl-chloride’s one (PVC, red and blue spectrum, figure 3) and those which have two spectral bands (597 and 527 cm−1) characteristic of the polyvinylidine-chloride presence13 (PVDC, green spectrum, figure 3).
Figure 3.
Typical Fourier transformed infrared spectroscopy of a polyvinyl-chloride polymer packaging with (green spectrum) and without (blue and red spectrum) polyvinylidine-chloride.
The analysis highlighted that 105 out of the 235 captopril drug samples were packaged in blisters containing PVDC and 130 in blisters only composed of PVC. In the case of amlodipine, none of the plastic blisters used to package the 245 amlodipine samples contained PVDC (table 2). A total of 60 amlodipine samples were packaged in blisters consisting of foil–foil sealed aluminium (table 2).
Table 2.
Number of amlodipine and captopril drug samples as a function of blister identity
| Blister identity | Amlodipine | Captopril |
| PVC only | 245 | 130 |
| Aluminium only | 60 | None |
| PVC-PVDC | None | 105 |
PVC, polyvinyl-chloride; PVDC, polyvinylidine-chloride.
Drugs assays as a function of blister identifications
From the results obtained in the Chromatographic purity profiles of the drugs section, captopril assays results were separated based on the presence of PVDC or not (PVC only). Amlodipine assay results were divided in two groups: the group of samples packaged in foil–foil sealed aluminium blisters and the one packaged in PVC blisters (PVC only). The results are provided in figure 4.
Figure 4.
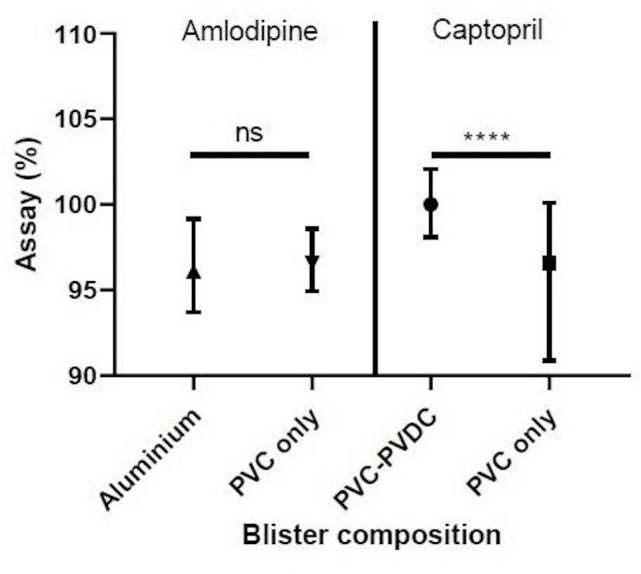
Medians of drug assays with IQRs as a function of the drug and the blister composition; ****p<0.0001. PVC, polyvinyl-chloride; PVDC, polyvinylidine-chloride; ns, non-statistically significant.
For amlodipine, no statistical difference in dosage (p=0.7684) was observed between the group with foil–foil aluminium packaging (median=96.10, n=60) and the group with PVC blister packaging (median=96.60, n=245).
For captopril, on the other hand, a statistical difference (p<0.0001) was found between the group of samples stored in blisters containing only PVC (median=96.60, n=130) and those stored in blisters containing PVC/PVDC (median=100.0, n=105).
Discussion
Substandard cardiac medicines represent a serious health hazard and result in significant morbidity and mortality.4 The SEVEN study was the first major study of cardiovascular drugs in Sub-Saharan Africa.5–7 The analysis of samples collected in Africa and through various sales spots of all kinds showed that among the products used in cardiovascular diseases, about 15%–20% were of low quality, and the prevalence of poor quality is higher for the products containing amlodipine and captopril. Given this observation and the fact that these two active substances are particularly sensitive to humidity and heat, the question arose as to whether the intrinsic stability of the latter had contributed more to the quality defects highlighted at the time. So, in this follow-up study, we have sought to provide some answers to this question by focusing on the search of associated degradation products and the nature of the packaging used at the time of the onsite collections.
We, therefore, sought to supplement the assay results with chromatographic purity studies on samples of the various cardiological drugs samples collected during the SEVEN study. We noted that the levels of impurities are particularly high for captopril and amlodipine samples (>0.5% compared with the considered active substance), as is their high prevalence of underdosing relative to other products, as previously mentioned. Of course, this problem could have been caused by the use of poor-quality active ingredient. But the fact that it is specific to these two active substances did not allow us to limit to this aspect alone. We, therefore, also turned our attention to the stability issue and to what goes hand in hand with this aspect. The identification of chromatographic impurities present concomitantly with the active substance was carried out to support our hypotheses related to the degradation of these compounds.
In the case of the captopril drug samples, the compound detected (figure 1) in addition to captopril was identified as captopril disulfide, a well-known degradation product of captopril that is prompt to be formed under moisture and heat.14 In other words, this would mean that the underdoses initially observed in the captopril products6 could be attributed to the poor quality of the active substance used and/or, to a larger extent, to degradation occurring either during manufacture and/or during improper storage. However, as it is well depicted that captopril is far more susceptible to degradation in the presence of some excipients than alone,15 16 one can fathom that the presence of captopril disulfide may more likely result from degradation due to uncontrolled exposure. As for amlodipine, chromatographic analyses showed in 30 samples the presence of an impurity due to amlodipine-lactose interaction (figure 2B). Such interaction was shown to occur in time and mostly under high humidity conditions,17 which could, to some extent, explain the poor assays observed in SEVEN study.7
These results are consistent with data in the literature in that the moisture vapour transmission rate18 (MVTR) must be controlled as it is critical to the stability of captopril14 and amlodipine.19 The corollary is that we have indeed shown, in the case of captopril, a significant difference (p<0.0001, figure 4) in active substance content between tablets extracted from PVC blisters and those from PVC-PVDC blisters that exhibit lower MVTR.18 The results for amlodipine are not statistically conclusive, but somehow the trend is noticeable since samples with a peak area of the amlodipine-lactose interaction product greater than 0.5% (w/w) were exclusively from the blisters with higher MVTR that is, the blisters composed of PVC as opposed to the foil–foil aluminium ones.18 Accordingly, it can be seen that the use of low moisture barrier packaging for these two products among the different cardiac drugs tested appears to have contributed to their low assay values.
This poor quality, represented by both a lower active substance content and the presence of degradation products, subjects the patient to safety risks. On the one hand, any dose lower than the dose to which the body has developed tolerance may induce an effect that is difficult to predict and may even be contrary to the action of the usual dose.20 On the other hand, the degradation products formed may be toxic.21
Captopril disulfide is a well-known metabolite of captopril, which can reversibly interconvert into captopril in the blood.22 However, in human pharmacokinetic studies, the amount of captopril disulfide in the blood never exceeds 8% of that of captopril.22 23 Therefore, clinical consequences of exposure to higher amounts of captopril disulfide are unknown. This is to be considered because the disulfide metabolites of sulfur-based drugs were 50–100 times more toxic on hepatocytes from isolated rats than the parent drugs.24
In some amlodipine samples, two main degradation products were detected as mentioned earlier, amlodipine impurity A that corresponds to the oxidation of its dihydropyridine ring and the amlodipine-lactose interaction product. Impurity A has been reported to be among the most found metabolites in urines (7%).25 As its level was always inferior to 2% relative to the active substance in the samples analysed, one can assume that this presence may have a limited impact to the patients. As for the amlodipine-lactose interaction product, no data are currently available on its fate in the body and its toxicity, which makes it a risk to consider.
Overall, on the basis of these additional results from the study of the chromatographic profiles of the collected samples, significant quantities of cardio drugs sold on African soil may not only present a lack of efficacy but also safety issues, due to the presence of impurities and/or degradation products resulting from poor storage and packaging conditions.
Limitations of the study
This study is of an observational type and even if as much information as possible has been collected for the research and attribution of causes likely to be at the origin of the active substance dosage defect, other factors than those related to packaging and storage problems may be involved. The lack of active substance is most likely multi-factorial and it may be useful to explore with more samples when applicable.
Conclusion
Further studies of captopril and amlodipine samples from Africa showed that their low assays would result in part from the degradation of the active substance, which may indicate that protective measures to avoid degradation of the drug products were not commensurate with their unstable behaviour, particularly in the presence of moisture and heat. FTIR analyses of the samples’ blisters disclosed they differ in material composition for the same active substance. In the case of captopril, statistical analysis has shown that the active substance content of products in tighter blister packs is higher than that of products in less moisture-resistant packaging. In the case of amlodipine, only the samples with low moisture resistant packaging had high amounts (>0.5%, w/w) of degradation products.
Using packaging with elevated moisture barrier properties could be a significant leverage to reduce the prevalence of substandard drugs in countries where medicines circuit and storage are poorly controlled. It is, therefore, also important to make the health authorities in these countries aware that the quality of packaging must also be taken into account when evaluating medicines supplied.
Supplementary Material
Footnotes
Contributors: P-HS, BD, MA and XJ involved in study concept and design. MSI, RN′G, DB, ASA, PZ and JLT are responsible for samples collection. MB, BD, P-HS and NY involved in chemical analysis. P-HS, BD, MCP, MA and XJ involved in statistical analysis. All authors contributed to the interpretation of data, drafting the manuscript and approved the final version to be published.
Funding: The SEVEN Study was exclusively supported by grant AAP-2014-042 from the Agence Nationale de Sécurité du Médicament et des Produits de Santé as well as by Institut National de la Santé et de la Recherche Médicale (grant : N/A), Assistance Publique - Hôpitaux de Paris (grant : N/A), and Paris Descartes University (grant : N/A).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No data are available. No additional data available.
References
- 1.Nayyar GML, Breman JG, Mackey TK, et al. . Falsified and substandard drugs: stopping the pandemic. Am J Trop Med Hyg 2019;100:1058–65. 10.4269/ajtmh.18-0981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnston A, Holt DW. Substandard drugs: a potential crisis for public health. Br J Clin Pharmacol 2014;78:218–43. 10.1111/bcp.12298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Almuzaini T, Choonara I, Sammons H. Substandard and counterfeit medicines: a systematic review of the literature. BMJ Open 2013;3:e002923. 10.1136/bmjopen-2013-002923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bowry ADK, Lewey J, Dugani SB, et al. . The burden of cardiovascular disease in low- and middle-income countries: epidemiology and management. Can J Cardiol 2015;31:1151–9. 10.1016/j.cjca.2015.06.028 [DOI] [PubMed] [Google Scholar]
- 5.Antignac M, Diop BI, Do B, et al. . Quality assessment of 7 cardiovascular drugs in 10 sub-Saharan countries: the seven study. JAMA Cardiol 2017;2:223. 10.1001/jamacardio.2016.3851 [DOI] [PubMed] [Google Scholar]
- 6.Antignac M, Diop BI, Macquart de Terline D, et al. . Fighting fake medicines: first quality evaluation of cardiac drugs in Africa. Int J Cardiol 2017;243:523–8. 10.1016/j.ijcard.2017.04.099 [DOI] [PubMed] [Google Scholar]
- 7.Macquart de Terline D, Diop BI, Bernard M, et al. . Substandard drugs among five common antihypertensive generic medications: an analysis from 10 African countries. J Hypertens 2018;36:395–401. 10.1097/HJH.0000000000001560 [DOI] [PubMed] [Google Scholar]
- 8.Khan MH, Hatanaka K, Sovannarith T, et al. . Effects of packaging and storage conditions on the quality of amoxicillin-clavulanic acid - an analysis of Cambodian samples. BMC Pharmacol Toxicol 2013;14:33. 10.1186/2050-6511-14-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asafu-Adjaye EB, Carlin AS, Jefferson EH, et al. . Comparative stability study of unit-dose repackaged furosemide tablets. Clin Res Regul Aff 2011;28:38–48. 10.3109/10601333.2011.568492 [DOI] [Google Scholar]
- 10.Ogbonna AC, Harris DJ. Thermal comfort in sub-Saharan Africa: field study report in Jos-Nigeria. Appl Energy 2008;85:1–11. 10.1016/j.apenergy.2007.06.005 [DOI] [Google Scholar]
- 11.Scrivens G, et al. The humidity exposure of packaged products. Accelerated Predictive Stability:105–46. [Google Scholar]
- 12.Newton PN, Lee SJ, Goodman C, et al. . Guidelines for field surveys of the quality of medicines: a proposal. PLoS Med 2009;6:e1000052. 10.1371/journal.pmed.1000052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bower D, Maddams WF. The vibrational spectroscopy of polymers. Cambridge University Press, 1989. [Google Scholar]
- 14.França LdeM, Pimentel MF, Simões SdaS, et al. . Nir hyperspectral imaging to evaluate degradation in captopril commercial tablets. Eur J Pharm Biopharm 2016;104:180–8. 10.1016/j.ejpb.2016.05.005 [DOI] [PubMed] [Google Scholar]
- 15.Tôrres AR, Grangeiro S, Fragoso WD. Multivariate control charts for monitoring captopril stability. Microchemical Journal 2015;118:259–65. 10.1016/j.microc.2014.07.017 [DOI] [Google Scholar]
- 16.Stulzer HK, Rodrigues PO, Cardoso TM, et al. . Compatibility studies between captopril and pharmaceutical excipients used in tablets formulations. J Therm Anal Calorim 2008;91:323–8. 10.1007/s10973-006-7935-1 [DOI] [Google Scholar]
- 17.Abdoh A, Al-Omari MM, Badwan AA, et al. . Amlodipine besylate-excipients interaction in solid dosage form. Pharm Dev Technol 2004;9:15–24. 10.1081/PDT-120027414 [DOI] [PubMed] [Google Scholar]
- 18.Waterman KC, MacDonald BC. Package selection for moisture protection for solid, oral drug products. J Pharm Sci 2010;99:4437–52. 10.1002/jps.22161 [DOI] [PubMed] [Google Scholar]
- 19.Malcolm L. Accelerated stability assessment program (ASAP) applications in a postapproval environment. Accelerated Predictive Stability 2018:287–304. [Google Scholar]
- 20.Peper A. Aspects of the relationship between drug dose and drug effect. Dose Response 2009;7:dose-response.0. 10.2203/dose-response.08-019.Peper [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Melo SRdeO, Homem-de-Mello M, Silveira D, et al. . Advice on degradation products in pharmaceuticals: a toxicological evaluation. PDA J Pharm Sci Technol 2014;68:221–38. 10.5731/pdajpst.2014.00974 [DOI] [PubMed] [Google Scholar]
- 22.Migdalof BH, Antonaccio MJ, McKinstry DN, et al. . Captopril: pharmacology, metabolism and disposition. Drug Metab Rev 1984;15:841–69. 10.3109/03602538409041080 [DOI] [PubMed] [Google Scholar]
- 23.Duchin KL, McKinstry DN, Cohen AI, et al. . Pharmacokinetics of captopril in healthy subjects and in patients with cardiovascular diseases. Clin Pharmacokinet 1988;14:241–59. 10.2165/00003088-198814040-00002 [DOI] [PubMed] [Google Scholar]
- 24.Jatoe SD, Lauriault V, McGirr LG, et al. . The toxicity of disulphides to isolated hepatocytes and mitochondria. Drug Metabol Drug Interact 1988;6:395–412. 10.1515/DMDI.1988.6.3-4.395 [DOI] [PubMed] [Google Scholar]
- 25.Stopher DA, Beresford AP, Macrae PV, et al. . The metabolism and pharmacokinetics of amlodipine in humans and animals. J Cardiovasc Pharmacol 1988;12 Suppl 7:S55–9. 10.1097/00005344-198812007-00012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.