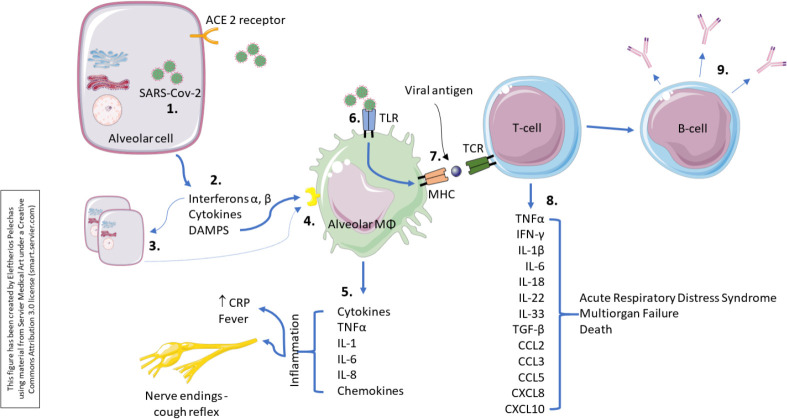
Figure 2.
Immunological response to SARS-CoV-2.
While the virus is self-replicating in the alveolar cells,1 it also damages it, and this will initiate the inflammatory response. Injured alveolar cells release interferons, cytokines as well as its intracellular components.2 Interferons α, β act in a paracrine manner, and have numerous effects on the surrounding cells preparing them for the ongoing infection. The primary function is to induce protection against viruses in neighbouring non-infected cells.3 Alveolar macrophages detect cell injury via damage-associated molecular patterns from the alveolar cells.4 They also respond to the cytokines released by injured alveolar cells. This causes the alveolar macrophages themselves to secrete cytokines such as TNFα, IL-1, IL-6, IL-8, as well as other chemokines.5 The inflammatory process occurring within the lung parenchyma stimulates nerve endings responsible for initiating the cough reflex. Thus, people often present with a dry cough early on. TNFα and IL-1β are pro-inflammatory cytokines and cause increased vascular permeability and increase in expression of adhesion molecules. This allows recruitment of more immune cells including neutrophils and monocytes. The alveolar macrophage can also detect the virus6 using its special receptors, called Toll-like receptors (TLRs). It can engulf the virus particles to phagocytosis, process it, and then present it on its surface.7 Studies have shown that the viral proteins can be presented. By presenting the viral proteins, specific T-cells may recognise them and mount an adaptive immune response8 consisting of T-cell activation and production of a plethora of proinflammatory cytokines and chemokines that may lead to a cytokine storm. In addition, B-cells or the plasma cells will then be activated and produce antibodies against the viral proteins.9