Graphical abstract
Keywords: Cancer patients, Coronavirus (COVID-19), Prevention, Oncology ward
Highlights
-
•
During COVID-19 pandemic cancer patients are a vulnerable category.
-
•
Few data about control infection strategy to ensure a COVID-19 free Oncology ward.
-
•
The essence of our protocol: triage, risk zones, traffic control and surveillance.
-
•
This strategy could be a practical contribution to control nosocomial COVID-19.
Abstract
The Coronavirus Disease-2019 (COVID-19) pandemic is spreading in Italy and Lombardy is one of the most affected region. Cancer patients are higher risk of complication from COVID-19 complications; therefore they should be protected from contagion while still ensuring access to cancer care.
The aim of this article is to suggest a strategy to reorganize hospital spaces and Healthcare Professionals (HCPs) staff in order to avoid COVID-19 nosocomial infection in an Oncology ward. SARS-CoV-2 is primarily transmitted through respiratory droplets and by contact. We speculated that precautions against droplet and contact transmission should be the proper way to preserve ward from COVID-19.
The essence of our protocol involves: triage outside of the ward, identification of risk zones, traffic control, surveillance of all the involved subjects. Whoever attends the ward must follow the general risk prevention and mitigation measures. The application of this practical strategy can contribute to breaking the cycle of community-hospital-community transmission.
1. Introduction
The Coronavirus Disease - 2019 (COVID-19) pandemic started in Italy on February 21, 2020. Lombardy was the most affected region, with a total of 130.479 cases and 17.103 deaths by October 20 (Anon., 2020d).
Luigi Sacco Hospital is a well known national infectious disease center. During the highest influx it increased the number of beds dedicated to COVID-19 patients up to a total of 280, 30 of which in the Intensive Care Unit (ICU).
Strict measures have been adopted by the Italian Government to deal with the emergency and to contain the exponential transmission of the disease.
On March 9, 2020 the so-called lockdown was imposed: all non-essential business activities, stores, schools and public places were shut down and restrictive measures were put in place to limit the mobility of people. Social distancing, which means keeping a safe distance from others and avoiding crowded spaces, has been required and limitations in contacts between people were strongly encouraged.(Signorelli et al., 2020)
The high contagiousness of COVID-19 due to direct transmission through respiratory droplets and to indirect propagation through contaminated surfaces has favored the rapid spread of the pandemic.(World Health Organization, 2020)
In this dramatic setting, specific attention should be paid to cancer patients, who have a higher infection rate and a higher incidence of severe events or death related to COVID-19 compared to the general population. (Jing et al., 2020; Liang et al., 2020a)
In Italy the prevalence of cancer in 2019 was 3.460.025 (5,3% of the entire population), with an incidence of 371.000 new cases; in Lombardy 60.000 new cancer diagnosis were estimated (Anon., 2020a).
All the efforts should be made to limit the risk of contagion in these patients, but at the same time it is mandatory to guarantee appropriate oncological care in order to avoid the risk of cancer progression. (Cortiula et al., 2020; Burki, 2020)
Different international scientific societies of medical oncology, such as National Comprehensive Cancer Network (NCCN), European Society of Medical Oncology (ESMO) and Italian Association of Medical Oncology (AIOM), provided recommendations for clinical activities during the pandemic: for instance, they suggested postponing follow up visits, to prioritizing treatments, balancing the cost/benefit ratio and adapting therapies in the effort to reduce the number of visit in the hospital. (NCCN (National Comprehensive Cancer Network), 2020; ASCO (American Society of Clinical Oncology), 2020; ESMO (European Society for Medical Oncology), 2020; AIOM (Associazione Italiana di Oncologia Medica), 2020a, b)
Nevertheless, some cancer patients need hospitalization, which is often an unavoidable step in their pathway of care with different purposes: the treatment of refractory symptoms, the management toxicities, the execution of complex diagnostic procedures, the administration of multiday chemotherapy, etc. (Numico et al., 2015)
Limited suggestions are available for the management of an Oncology Department during the COVID-19 pandemic regarding the prevention of infection and control procedures.(Al-Shamsi et al., 2020)
The aim of this article is to suggest a practical strategy to reorganize spaces and Health Care Professionals (HCPs), in order to avoid COVID-19 nosocomial infection in an Oncology ward.
2. General consideration
To date the modality of SARS-CoV-2 transmission is only partially known. According to current evidence, the COVID-19 virus is primarily transmitted between people through respiratory droplets but also by contact routes. The latter can consist of direct contact with infected people or indirect contact with contaminated surfaces in the immediate environment or with objects used by the infected person.(Liu et al., 2020)
Based on this assumption, we speculated that droplets and contact isolation precautions were the proper way to protect patients and HCPs who attend an Oncology ward. A lot of recommendations and scientific reports are available on the procedures to follow for the correct management of a COVID-19 ward (Anon., 2020b) but there are very little and fragmentary data on infection control strategies aimed to ensure a COVID-19 free ward. (He et al., 2020; Givi et al., 2020)
This is a key point especially in the management of particularly vulnerable categories of patients, such as those with cancer. Moreover, the importance of identifying suitable strategies will become even more necessary over time, considering that epidemiological data do not predict a rapid resolution of the pandemic. (He et al., 2020; Givi et al., 2020)
3. Materials and methods
3.1. Patients’ selection
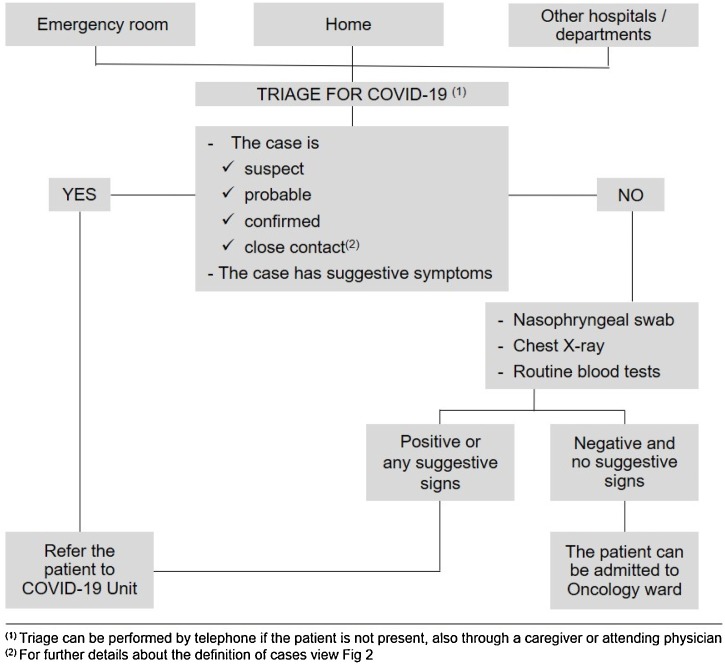
The first step in order to avoid the spread of COVID-19 infection inside a ward is the proper selection of patients (Fig. 1 ).
Fig. 1.
Pathway of patient selection.
All patients who had close contact with suspect, probable or confirmed cases are not eligible for admission to Oncology ward (Table 1 ).
Table 1.
Definition of a suspect, probable, confirmed and close contact case, according to the World Health Organization (WHO).
| SUSPECT CASE | Patient with severe acute respiratory infection (fever and at least one sign / symptom of respiratory disease - e.g. cough, dyspnea), without an etiology that fully explains the clinical presentation and that requires hospitalization |
| PROBABLE CASE | Patient defined as suspect but with a doubtful or inconclusive result at a SARS-CoV-2 test performed in a Regional Reference laboratory using a specific SARS-CoV-2 Real Time PCR protocol or a positive result using a pan-coronavirus test. |
| CONFIRMED CASE | A case with a confirmed SARS-CoV-2 infection, tested in a Regional Reference laboratory, regardless of clinical signs and symptoms. |
| CLOSE CONTACT CASE |
|
Patients who are admitted to the oncology ward can come from:
-
-
Emergency room (ER): all patients undergo a specific triage, performed by HCPs using a form with close questions (Table 2 ), a chest x-ray without any sign suggestive for interstitial/inflammatory lung disease and a nasopharyngeal swab, that must be negative for COVID-19.
-
-
Home: only after a telephone triage (for questions see Table 2) to ensure patients do not have any symptoms suggestive for COVID-19 and didn’t have close contacts with suspect, probable or confirmed cases. Before admission, these patients also have to undergo a nasopharyngeal swab, chest x-ray and routine blood tests
-
-
Other hospital or departments: after a telephone triage (for questions see Table 2) with the physician (exclusion of suspect symptoms and recent close contacts with suspect, probable or confirmed cases) and the execution of a nasopharyngeal swab up to 48 h prior to the transfer, a chest x-ray and blood tests.
Table 2.
Questionnaire used for triage.
| PATIENT/CAREGIVER: Name and Surname ……………………………………………………………………………………………… | |||
|---|---|---|---|
| ASSESSMENT OF SUSPECTED CONTACT WITH CONFIRMED CASE | |||
| 1 | Do you live in the same home with a suspected or confirmed COVID-19 case? | yes | no |
| 2 | Have you been in close contact (face-to-face) or in the same closed space with a suspected (…) or confirmed (…) COVID-19 case? | yes | no |
| 3 | Are you a healthcare professional who has managed a suspected (…) or confirmed (…) case of COVID-19 or a member of laboratory staff involved in the SARS-CoV-2 samples processing? | yes | no |
| 4 | Do you have any of these symptoms? | yes | no |
| Cough - Dyspnea – Sore throat - Myalgia - Diarrhea - Conjunctivitis - Alteration of taste and smell | |||
| 5 | Have you had fever in the past 15 days? | yes | no |
| 6 | Do you have relatives with any of these symptoms? | yes | no |
| Cough - Dyspnea - Sore throat - Myalgia - Diarrhea - Conjunctivitis – Alteration of taste and smell | |||
| 7 | Do you have any relative who has had a fever in the past 15 days? | yes | no |
| 8 | Have you been in emergency room or hospitalized in the past 15 days? | yes | no |
| 9 | Have you already performed swab for the detection of COVID-19? | yes | no |
| PATIENT’S CLINIC EVALUATION | |||
| Normal breathing | yes | no | |
| The patient is able to perform daily activities (dressing, washing, housework) | yes | no | |
| Body temperature | |||
| Oxygen saturation | |||
| Assessor ……………………………….. Date ……………………………… Patient/Caregiver (signature) …………………………………………………. |
|||
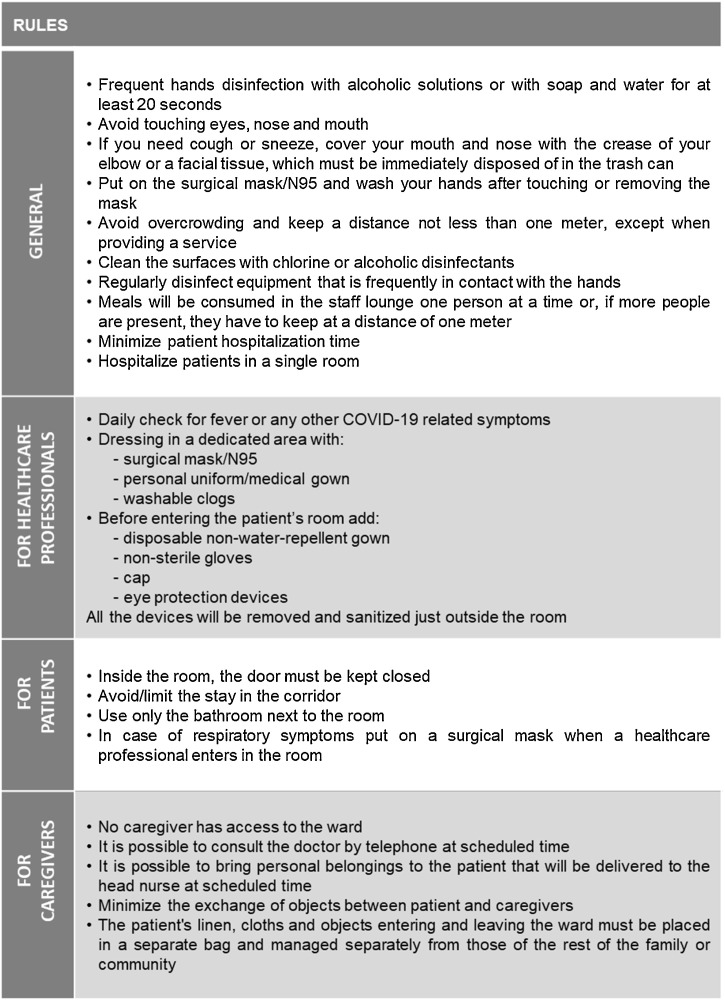
3.2. General rules
Whoever attends the ward must follow the general risk prevention and mitigation measures, that should be explained in detail (Fig. 2 ):
-
-
Frequent disinfection of the hands with alcoholic solutions or with soap and water for at least 20 s. Always wash your hands before having a meal, after using the toilet, after sneezing or coughing and after having contacts with surfaces that could be contaminated;
-
-
avoid touching eyes, nose and mouth;
-
-
if you need to cough or sneeze, cover your mouth and nose with the crease of your elbow or a facial tissue, which must be immediately disposed of in the trash can after being used;
-
-
put on the surgical mask/N95 and wash hands after touching or removing the mask;
-
-
avoid overcrowding and keep a distance of at least one meter, except when providing a service (medical examination, sampling, patient hygiene, medication, etc …) ;
-
-
clean the surfaces (e.g. toilets, nursing trolleys, tables) with chlorine or alcoholic disinfectants;
-
-
regularly disinfect equipment which is frequently in contact with your hands, such as door knobs, mobile phones, laptops and other facilities;
-
-
reduce the time of patient hospitalization to minimize the risk of possible exposure to infection;
-
-
hospitalize each patient in an individual room.
Fig. 2.
Rules for the practical organization of the Oncology ward.
In order to facilitate the application of the rules, especially for those who attend the ward only occasionally, the distribution of brochures and the display of a poster with a summary can help.
4. Rules for the healthcare professionals
HCPs should be the first to comply with behavioral rules and set a good example for patients. For this reason, training on the correct use of personal protective equipment (PPE) is essential and should be frequently repeated. The employment of these procedures has led to increased workloads and anxiety of HCPs. Despite the great effort required, all HCPs should continue to work with maximum care and professionalism, keeping in mind the important goal that needs to be achieved. Support from managers, workplace culture and facilities can positively influence the ability and willingness of HCPs to follow guidelines.(Houghton et al., 2020)
Every day all the staff should be checked before entering the ward for fever or any other COVID-19 related symptoms: in the case of suspected infection, the HCP should be immediately referred to the COVID-19 care unit.
The dressing takes place at the entrance of the department at the beginning of the work shift, in a dedicated area; each HCP must wear:
-
-
surgical mask/N95;
-
-
personal uniform/medical gown;
-
-
washable clogs.
HCP should wear clean PPE before entering each room to perform health care duties:
-
-
disposable no water-repellent gown (e.g. no woven surgical gowns);
-
-
non-sterile gloves;
-
-
cap;
-
-
eye protection devices.
Once patient assistance is finished, it is possible to proceed with the undressing, always remaining in the anteroom:
-
-
remove and sanitize eye protection devices;
-
-
throw cap, disposable gown and non-sterile gloves in a special container;
-
-
sanitize hands.
Another important goal is PPE preservation. All the devices should be used with attention and sparingly: for example only the HCPs dedicated to the assistance of patients with respiratory symptoms unable to wear surgical masks (altered cognitive state, O2 therapy in progress, tracheostomy) could be equipped with N95 mask.
5. Rules for patients
Upon arriving in the ward, patients and caregivers should be promptly informed by the head nurse or by the attending physician about the current standard of behavior. To avoid misunderstanding, it can be useful to provide patients with educational pamphlets written in a clear, brief and easy manner.
Patients should comply with the contact isolation protocol and moreover:
-
-
stay inside the rooms keeping the door closed (see-through doors if possible);
-
-
avoid/limit the stay in the corridor;
-
-
use exclusively the bathroom next to the room;
-
-
put on a surgical mask when a HCP enters the room in the case of respiratory symptoms.
If during the hospitalization period a patient develops suggestive symptoms, he/she will be treated as per World Health Organization (WHO) guidelines as a COVID-19 suspect patient.(WHO, 2020) A nasopharyngeal swab will be performed wearing appropriate PPE.
6. Rules for caregivers
In order to avoid the spread of contagion, no unauthorized person can enter the ward.
Visits of relatives and friends are forbidden.
It is possible to bring items to the patient, that will be delivered to the head nurse at a scheduled time, however the exchange of objects between patient and caregivers should be minimized.
The patient's linen, cloths and objects entering and leaving the ward must be placed in a separate bag (provided at the time of collection from the head nurse) and managed separately from those of the rest of the family or community (linen and cloths can be washed in the washing machine using common detergent at 60 °C for at least thirty minutes or for a shorter times at higher temperatures).
We recommend only one person to be designated as the caregiver.
It is possible to consult the physician by telephone at a scheduled time.
Of course, these restrictive rules negatively impact on peacefulness and psychological well-being of patients and relatives but are necessary. To overcome the problem, it can be useful identify and also provide alternative tools (like tablets, mobile phones) to keep patients in contact with other people.(Lima et al., 2020)
7. Rules for the management of the environment
7.1. Patient room
-
-
The area in front of the room will be equipped with a section with all the necessary items for dressing and for the sanitization of hands and medical equipment.
-
-
Each room will be sanitized before the arrival of a new patient.
-
-
Each room will be equipped with containers for waste and biological material, dedicated medical and nursing devices for exclusive use (e.g. sphygmomanometer, pulse oximeter, stethoscope), while other equipment will be sanitized after use.
-
-
It is appropriate to ensure adequate air exchange (if an air-purifying system is not available by periodically opening the windows).
7.2. Common areas
In these areas (corridors, wound dressing rooms, soiled and clean utility room, nursing, dispensary, medical offices, lounge room, toilets) the general risk prevention and mitigation measures will be observed (see general rules paragraph), moreover:
-
-
meals will be consumed in the staff lounge one person at a time or any case in a way that guarantees the adequate distance of at least 1 m; surfaces and objects will be sanitized after use;
-
-
to facilitate the sanitizing, common areas will be equipped with alcohol-based solution dispensers and all the necessary items for disinfecting hands and surfaces.
7.3. Access routes to the ward and patient transport
In order to guarantee patient and staff safety, it’s important to define different pathways to keep infected and non-infected peoples separate. Patients and staff enter / leave the ward through previously identified paths (stairs, elevators, corridors), through which COVID-19 patients / staff cannot pass. Each transition zone between dirty/hot zone and clean zone must be clearly marked.(Schwartz et al., 2020)
When a patient needs to be transported outside the ward for procedures or visits:
-
-
the patient must wear surgical mask, disposable cap and gown, non-sterile gloves when leaving the room. All the devices must be removed and thrown in special containers when he/she comes back into the room;
-
-
the HCPs must put on the same devise plus eye protection in a dedicated filter area (e.g patient anteroom); they will be removed and sanitized once back in the ward;
-
-
mobile and non-mobile devices (e.g. wheelchair, walker, stretcher, etc.) used during the transport will be sanitized when returning to the ward.
8. Surveillance
It is necessary to plan scheduled educational sessions in order to update all the staff on the newest information available and on any guideline variation.
The goal of maintaining a COVID-19-free department and avoiding contagion, cannot be achieved without the implementation of a strict active surveillance protocol that includes the execution of nasopharyngeal swab, associated with other validated methods when available. The surveillance must be performed periodically on HCPs and on patients whenever a confirmed COVID-19 case occurs in the ward.
9. Discussion
Oncologists have no reliable data about susceptibility to COVID-19 and on morbidity and mortality specifically in cancer patients. Our limited knowledge is made up of assumptions extrapolated from past experiences with other infectious diseases, the non-specific definition of immunocompromised state in cancer (caused by malignancy or therapy) and a small amount of pathogenic and epidemiologic data regarding COVID-19 in cancer patients.
In the Chinese experience, malignancy is a preexisting comorbidity in 1.4 % of patients affected by COVID-19 and probably it is also a prognostic factor.(Cai et al., 2020) In fact, cancer patients have an estimated 2 fold increased risk of being infected with COVID-19 compared to the general population (World Health Organization (WHO), 2020), and a significantly higher incidence of severe events, e.g. death or ICU admission requiring invasive ventilation (39 % vs 8%; p = .0003). (Liang et al., 2020b)
There’s also lack of data about SARS-CoV-2 transmission by asymptomatic or pre-symptomatic carriers (Hu et al., 2020; Qian et al., 2020) and until a specific therapy or vaccine for SARS-CoV-2 becomes available, prevention is the only silver bullet.
The essence of our protocol involves: triage outside the Oncology ward, identification of risk zones, traffic control through adequate pathways and surveillance of all the subjects involved. It can contribute to reduce infections among patients and HCPs, breaking the cycle of community-hospital-community transmission. A similar tool proved to be effective in dramatically reducing infection rates among HCPs in Taiwan during the SARS (Severe Acute Respiratory Syndrome) outbreak (Schwartz et al., 2020).
Oncologists need to preserve the continuum of care both in their out- and in-patients setting. The new suggestions about the reorganization of activities, such as working in teleconsultation, delaying the follow up visits and customizing treatment delivery, are not enough: some patients need hospitalization (Indini et al., 2020).
In this health emergency the major risk for cancer patients is to contract the infection. There is also the risk of not being able to have access to treatment in an Oncology Unit, not receiving general medical care for other comorbidities (e.g: suspension of elective surgery, surgical theatres transformed into ICUs, departments being closed) or for acute events (the whole hospital or emergency unit is exclusively dedicated to COVID-19 patients). Patients who need simultaneous and palliative care must be considered too. Besides, patients must perceive that the oncological teams still take care of them in order to avoid the so-called phenomenon of the “distraction effect”, in which patients are worried because they think COVID-19 captures the whole HCP’s attention, overshadowing cancer cure and prevention (Anon., 2020c; Cortiula et al., 2020). From patients advocacy associations and oncologists community worrying reports arrive about delay in performing examens, such as CT scan, histological analysis or molecular tests, together with an unprecedented disruption throughout the cancer research community, that can be very dangerous in this pandemic whose duration is unpredictable (Sharpless, 2020).
SARS and MERS (Middle East Respiratory Syndrome) experience taught us that a protocol based on the prevention of contact and droplet transmission should be adequate for fighting nosocomial SARS-CoV-2 infection (where no aerosolization is expected) (Chow, 2004). It is a legitimate compromise between HCPs protection and patient safety, avoiding counterproductive over-protection and allowing to anticipate a shortage in the supply of PPE, ensuring access to the necessary supplies for COVID-19 patient care.
As it happened in many countries, when the SARS-CoV-2 virus spread, many hospitals tried to understand which areas required the greatest amount of aid, with an increase in the number of hospital beds dedicated to COVID-19 patients.
This administrative policy and the isolation precautions (only single rooms allowed) resulted in a decrease in the capacity of the Oncology ward, which will probably be mitigated by the selection of patients and by the attempt to shorten the duration of hospitalization.
The isolation precautions would also cause a significant increase in time dedicated to patient care; it can be balanced out by optimizing the procedures, through better patients and HCPs selection.
Our job and projects are influenced by the absence of models and analyses able to predict the end of the spread of the virus and the possibility of a worsening of the COVID-19 pandemic. It leads us to recommend that all the strategies to contain the SARS-CoV-2 contagion should be relaxed only gradually and maintained at all levels of care for in- and outpatients: it means that the suggested strategy could be adopted and adapted by other medical specialty units too. Considering that pandemic will be in our society for a long time, a plan to prevent crush-down of health care system is required, especially it will be necessary give a priority level to those patients who are elder, who have chronic disease or who need palliative care. We must ensure assistance for clinical and ethical reasons to all these frail patients.
Even though more comprehensive evaluations will be needed to compare the relative costs and benefits, this simple and pragmatic strategy is meant to be a practical contribution to control nosocomial COVID-19 infection.
Few weapons and poor knowledge of the battlefield make planning and having a good strategy necessary for fighting the virus; but, as they say, "instead of cursing darkness, it's better to light a candle".
-
•
grants from EISAI
-
•
speaker bureau, travel expences for conference from ROCHE , GENTILI
-
•
advisory role from NOVARTIS and CELGENE
-
•
advisor role, travel expences for conference from PFIZER
-
•
advisory board from MSD
Declaration of Competing Interest
Dr. La Verde reports:
Other authors report no declaration of interest
Acknowledgement
The authors thank Joanna Landi for her technical assistance.
References
- (AIOM (Associazione Italiana di Oncologia Medica) 2020. Assicurare il proseguimento delle terapie salva-vita per tutti i pazienti oncologici e onco-ematologici.https://www.aiom.it/wp-content/uploads/2020/04/20200407_appello_AIOM-AIRO-SIE.pdf Available from: [Google Scholar]
- (AIOM (Associazione Italiana di Oncologia Medica) Rischio infettivo da coronavirus covid 19: indicazioni per l’oncologia. https://www.aiom.it/wp-content/uploads/2020/03/20200313_COVID19_indicazioni_AIOM-CIPOMO-COMU.pdf Available from:
- (ASCO (American Society of Clinical Oncology) 2020. ASCO Coronavirus Resources.https://www.asco.org/asco-coronavirus-information Available from: [Google Scholar]
- (ESMO (European Society for Medical Oncology) 2020. ESMO COVID-19 and Cancer.https://www.esmo.org/covid-19-and-cancer Available from: [Google Scholar]
- Al-Shamsi H.O., Alhazzani W., Alhuraiji A., Coomes E.A., Chemaly R.F., Almuhanna M., Wolff R.A., Ibrahim N.K., Chua M.L.K., Hotte S.J., Meyers B.M., Elfiki T., Curigliano G., Eng C., Grothey A., Xie C. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID‐19) pandemic: an international collaborative group. Oncologist. 2020;(April 3) doi: 10.1634/theoncologist.2020-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anon., 2020, https://www.aiom.it/i-numeri-del-cancro-in-italia/.
- Anon., 2020, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance.
- Anon., 2020, https://www.nytimes.com/2020/04/20/health/treatment-delays-coronavirus.html.
- Anon., 2020d, http://www.salute.gov.it/portale/nuovocoronavirus.
- Burki T.K. Cancer guidelines during the COVID-19 pandemic. Lancet Oncol. 2020;(April) doi: 10.1016/S1470-2045(20)30217-5. pii: S1470-2045(20)30217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Q., Huang D., Ou P., Yu H., Zhu Z., Xia Z., Su Y., Ma Z., Zhang Y., Li Z., He Q., Liu L., Fu Y., Chen J. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy. 2020;(April 2) doi: 10.1111/all.14309. [DOI] [PubMed] [Google Scholar]
- Chow C.B. Post-SARS infection control in the hospital and clinic. Paediatr. Respir. Rev. 2004;5(December (4)):289–295. doi: 10.1016/j.prrv.2004.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortiula F., Pettke A., Bartoletti M., Puglisi F., Helleday T. Managing COVID-19 in the oncology clinic and avoiding the distraction effect. Ann. Oncol. 2020;31(May (5)):553–555. doi: 10.1016/j.annonc.2020.03.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Givi B., Schiff B.A., Chinn S.B. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngol. Head Neck Surg. 2020;(March 31) doi: 10.1001/jamaoto.2020.0780. [DOI] [PubMed] [Google Scholar]
- He Y., Lin Z., Tang D., Yang Y., Wang T., Yang M. Strategic plan for management of COVID-19 in paediatric haematology and oncology departments. Lancet Haematol. 2020;(April 1) doi: 10.1016/S2352-3026(20)30104-6. pii: S2352-3026(20)30104-30106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houghton C., Meskell P., Delaney H. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst. Rev. 2020;4(April 21):CD013582. doi: 10.1002/14651858.CD013582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Z., Song C., Xu C., Jin G., Chen Y., Xu X., Ma H., Chen W., Lin Y., Zheng Y., Wang J., Hu Z., Yi Y., Shen H. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci. China Life Sci. 2020;63(May (5)):706–711. doi: 10.1007/s11427-020-1661-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indini A., Aschele C., Cavanna L., Clerico M., Daniele B., Fiorentini G., Fioretto L., Giordano M., Montesarchio V., Ortega C., Pinotti G., Scanni A., Zamagni C., Blasi L., Grossi F. Reorganisation of medical oncology departments during the novel coronavirus disease-19 pandemic: a nationwide Italian survey. Eur. J. Cancer. 2020;6(April (132)):17–23. doi: 10.1016/j.ejca.2020.03.024. [DOI] [PubMed] [Google Scholar]
- Jing Yu, Ouyang Wen, Chua Melvin L.K., Xie Conghua. SARS-CoV-2 transmission in cancer patients of a tertiary hospital in Wuhan. JAMA Oncol. 2020;(March 25) doi: 10.1001/jamaoncol.2020.0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang W., Guan W., Chen R., Wang W., Li J., Xu K., Li C., Ai Q., Lu W., Liang H., Li S., He J. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(March (3)):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang W., Guan W., Chen R., Wang W., Li J., Xu K., Li C., Ai Q., Lu W., Liang H., Li S., He J. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(March (3)):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima C.K.T., Carvalho P.M.M., IAAS Lima, JVAO Nunes, Saraiva J.S., de Souza R.I., da Silva C.G.L., Neto M.L.R. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease. Psychiatry Res. 2020;287(May):112915. doi: 10.1016/j.psychres.2020.112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Liao X., Qian S., Yuan J., Wang F., Liu Y., Wang Z., Wang F.S., Liu L., Zhang Z. Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China. Emerg Infect Dis. 2020;26(June (6)) doi: 10.3201/eid2606.200239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCCN (National Comprehensive Cancer Network) 2020. Coronavirus Disease 2019 (COVID-19) Resources for the Cancer Care Community.https://www.nccn.org/covid-19/ Available from: [Google Scholar]
- Numico G., Cristofano A., Mozzicafreddo A., Cursio O.E., Franco P., Courthod G., Trogu A., Malossi A., Cucchi M., Sirotovà Z., Alvaro M.R., Stella A., Grasso F., Spinazzé S., Silvestris N. Hospital admission of cancer patients: avoidable practice or necessary care? PLoS One. 2015;10(March (3)):e0120827. doi: 10.1371/journal.pone.0120827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian G., Yang N., Ma A.H.Y., Wang L., Li G., Chen X. A COVID-19 transmission within a family cluster by presymptomatic infectors in China. Clin. Infect. Dis. 2020;(March 23) doi: 10.1093/cid/ciaa316. pii: ciaa316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz J., King C.C., Yen M.Y. Protecting health care workers during the COVID-19 coronavirus outbreak–lessons from Taiwan’s SARS response. Clin. Infect. Dis. 2020;(March 12) doi: 10.1093/cid/ciaa255. pii: ciaa255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpless N.E. COVID-19 and cancer. Science. 2020;368(June (6497)):1290. doi: 10.1126/science.abd3377. [DOI] [PubMed] [Google Scholar]
- Signorelli C., Scognamiglio T., Odone A. COVID-19 in Italy: impact of containment measures and prevalence estimates of infection in the general population. Acta Biomed. 2020;91(April (3-S)):175–179. doi: 10.23750/abm.v91i3-S.9511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. WHO Guideline.https://www.who.int/health-topics/coronavirus [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2020. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) Feb 16-24. [Google Scholar]
- World Health Organization (WHO) 2020. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19)https://www.who.int/publications-detail/report-of-the-who-china-joint-missionon-coronavirus-disease-2019-(covid-19) (February 28). Retrieved from. [Google Scholar]