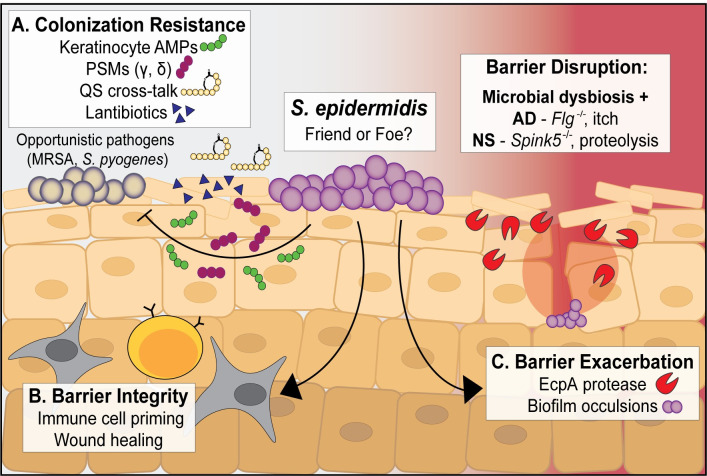
Fig 1. The ubiquitous skin commensal S. epidermidis positively and negatively impacts barrier homeostasis and integrity.
(A) S. epidermidis phenol soluble modulins PSMγ and PSMδ can synergize with keratinocyte-derived AMPs to kill opportunistic skin pathogens like MRSA and Streptococcus pyogenes. S. epidermidis also makes anti-MRSA quorum sensing inhibitor peptides and a variety of small antimicrobials known as lantibiotics to mediate skin colonization resistance. (B) S. epidermidis lipoteichoic acid and some lipopeptides can dampen the inflammatory response to skin injury, accelerating wound healing. Early skin colonization with S. epidermidis is crucial for development of immune cell subsets including effector T cells and MAIT cells, and long-term S. epidermidis skin colonization may help the cutaneous immune system distinguish between commensal and pathogenic bacteria. (C) Certain S. epidermidis strains can “bloom” and exacerbate AD or NS skin lesions through production of the EcpA protease. Inflammatory S. epidermidis biofilms that occlude sweat glands have also been shown to exacerbate some AD lesions. AD, atopic dermatitis; AMPs, antimicrobial peptides; MAIT cells, mucosal-associated invariant T cells; MRSA, methicillin-resistant Staphylococcus aureus; NS, Netherton syndrome; PSM, phenol soluble modulins; QS, quorum sensing.