Figure 2. Rotations of cardiology fellows in training (FIT) during stage 1 to 3 of the coronavirus disease 2019 (COVID‐19) crisis (as indicated by the red boxes).
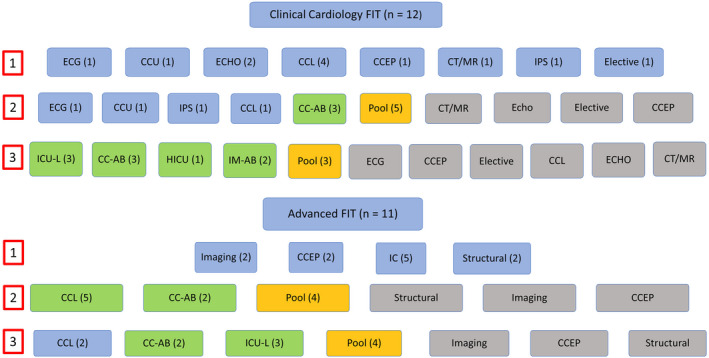
Stage 1 represents “business as usual.” Although stage 2 is characterized as minimal disruption of educational activities, hospital and departmental mitigation strategies required that FIT in “nonessential” activities shelter at home. Stage 3 is characterized by complete disruption of educational activities, mandated by the surge in COVID‐19 admissions that overwhelmed existing manpower. Cardiology FIT (C‐FIT) in the “pool” had several responsibilities, including backup for others in case of absence, remote services (adjudicate need for ECGs or echocardiograms and evaluate corrected QT interval for COVID‐19 patients), participate in C‐FIT deployment decisions, and participate in research or quality assurance projects. FIT assigned to coronary care unit (CCU) and inpatient service (IPS) were reassigned to COVID‐19 cardiology consultation teams (CCs) A and B. Blue indicates usual fellowship rotations; gray, inactive fellowship rotations; green, COVID‐19 patient care responsibilities; and yellow, pool. CCEP indicates clinical cardiac electrophysiology; CCL, cardiac catheterization laboratory; CT/MR, cardiac computed tomography/magnetic resonance imaging; ECHO, echocardiogram; HICU, hybrid intensive care unit; IC, interventional cardiology; ICU‐L, intensive care unit team for central lines (all intensive care units were COVID‐19 intensive care units); and IM‐AB, internal medicine teams A and B.
