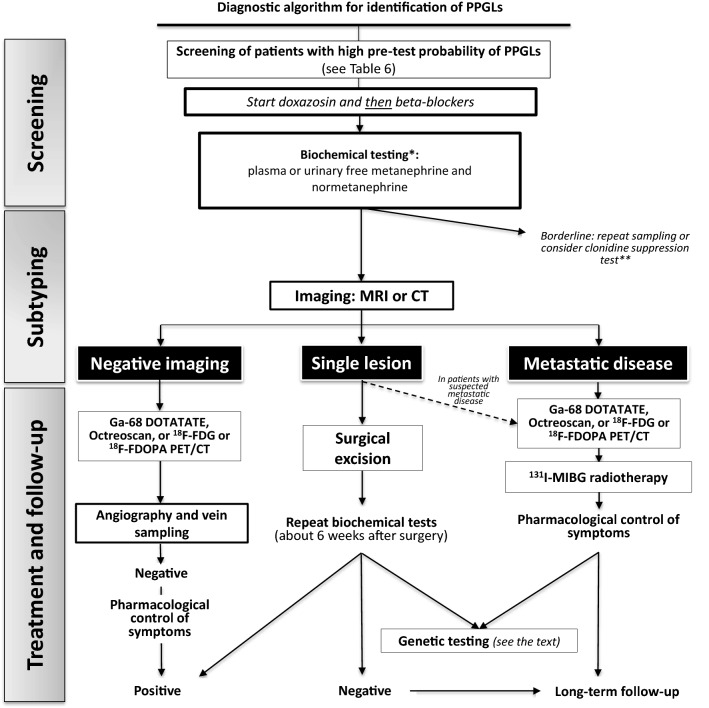
Fig. 3.
A schematic algorithm suggested for diagnosis and treatment of hypertensive patients with suspected of pheochromocytoma and paraganglioma. CT has been suggested as the first-choice imaging modality because of its excellent spatial resolution for thorax, abdomen, and pelvis. MRI is recommended in patients with metastatic PPGLs, for detection of skull base and neck paragangliomas. *Biochemical screening should be performed after withdrawing of interfering drugs and substances, including acetaminophen, labetalol, sotalol, α-methyldopa, tricyclic antidepressants, MAO-inhibitors, sympathomimetics, cocaine. **A quarter of patients with PPGLs show borderline biochemical results, likely due to inappropriate sampling. If results remain elevated after repeating the measurement, the clonidine suppression test with detecting of plasma normetanephrine can be used. This test has been claimed to have a 100% diagnostic specificity with a 97% sensitivity; however, it has not been validated in prospective studies. HT hypertension, CT computed tomography, MRI magnetic resonance imaging, MIBG metaiodobenzylguanidine, 18F-FDG [18F]-fluoro-fluorodeoxyglucose, 18F-FDOPA 6-[18F]-l-fluoro-l-3,4-dihydroxyphenylalanine, PET positron-emission tomography