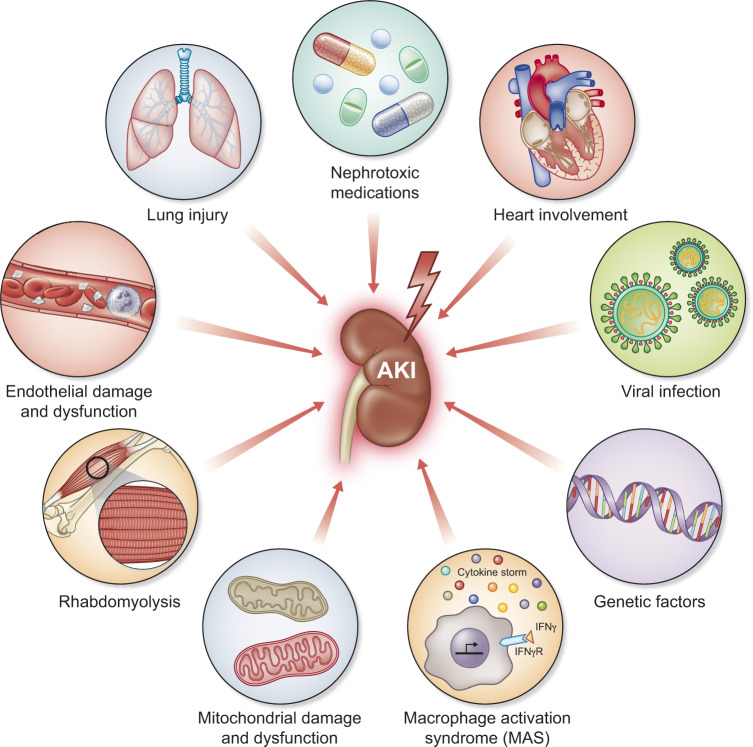
FIGURE 1.
Mechanisms of AKI in patients with COVID-19. Clockwise from the upper left corner: Lung injury releases DAMPs into circulation that are filtered at the glomerulus and bind with pattern recognition receptors on tubular epithelial cells. DAMPs also cause systemic inflammation which injures kidneys and other organs. Potentially nephrotoxic medications are commonly used in critically ill patients. Heart involvement is rare in COVID-19 but can have devastating effects on all organs including the kidney. High right heart pressures can occur from left heart failure but also from high positive end-expiratory pressures on mechanical ventilation. Direct viral infection of renal tubular epithelial cells has been reported. Genetic factors likely modify risk and disease presentation. Genetic variation in ACE receptor expression is one factor but also the APOL1 genotype is a known genetic risk factor for collapsing glomerulopathy that has been reported in some series. In a subset of patients with COVID-19, macrophage activation syndrome may occur resulting in uncontrolled inflammation and multiple organ failure. Mitochondrial damage and dysfunction can result from direct or indirect injury to the kidney. Rhabdomyolysis has been reported in some series resulting in AKI. Finally, endothelial damage and dysfunction appear commonly in COVID-19. Interestingly, disseminated intravascular coagulation is atypical and platelet counts remain normal in most patients suggesting that the kidney is not being damaged by thrombotic microagiopathy.