Abstract
Objectives:
To determine the association of the frailty phenotype with subsequent healthcare costs and utilization.
Design:
Prospective cohort study (Osteoporotic Fracture in Men [MrOS]).
Setting:
Six U.S. sites.
Participants:
1,514 community-dwelling men (mean age 79.3 years) participating in the MrOS Year 7 (Y7) examination linked with their Medicare claims data.
Measurements:
At Y7, the frailty phenotype was operationalized using five components and categorized as robust, pre-frail or frail. Multimorbidity and a frailty indicator (approximating the deficit accumulation index) were derived from claims data. Functional limitations were assessed by asking about difficulty performing instrumental activities of daily living. Total direct healthcare costs and utilization were ascertained during 36 months following Y7.
Results:
Mean (SD) of total annualized costs (2018 dollars) was $5,707 (8,800) among robust, $8,964 (18,156) among pre-frail and $20,027 (27,419) among frail men. Compared with robust men, frail (cost ratio [CR] 2.35 [95% CI 1.88-2.93]) and pre-frail (CR 1.28 [95% CI 1.11-1.48) men incurred greater total costs after adjustment for demographics, multimorbidity and cognitive function. Associations of phenotypic pre-frailty and frailty with higher total costs were somewhat attenuated, but persisted after further consideration of functional limitations and a claims-based frailty indicator. Each individual frailty component was also associated with higher total costs. Frail vs. robust men had higher odds of hospitalization (odds ratio [OR] 2.62 [95% CI 1.75-3.91]) and skilled nursing facility stay (OR 3.36 [95% CI 1.83-6.20]). A smaller but significant effect of the pre-frail category on skilled nursing facility stay was present.
Conclusions:
Phenotypic pre-frailty and frailty were associated with higher subsequent total healthcare costs in older community-dwelling men after accounting for a claims-based frailty indicator, functional limitations, multimorbidity, cognitive impairment and demographics. Assessment of the frailty phenotype or individual components such as slowness may improve identification of older community-dwelling adults at risk for costly, extensive care.
Keywords: frailty, multimorbidity, functional limitations, healthcare utilization, healthcare costs
INTRODUCTION
Frailty, as defined using the phenotypic approach1, is a geriatric syndrome characterized by markers (or components) of limited physiologic reserve across multiple organ systems including slowness, weakness, shrinking, poor energy and low physical activity. Compared with robust older adults, pre-frail and frail individuals are more likely to become disabled, have progression of chronic medical conditions and experience falls, fractures and mortality.2 While fewer studies have examined associations of the frailty phenotype or its individual components with healthcare costs, we previously reported that phenotypic frailty and pre-frailty were associated with higher subsequent healthcare expenditures in community-dwelling older women after accounting for traditional indicators including demographics and multimorbidity.3
The frailty phenotype depends on measurement of physical performance and assessment of activity level and energy. While these components are not routinely assessed in the practice setting or available in administrative data, there is a growing interest in capturing the construct of frailty using administrative data alone to select a target population for interventions including coordinated care to reduce subsequent healthcare utilization. Most claims-based frailty indicators4–8 have been developed using the deficit accumulation approach9,10 as a model since diagnosis and procedure codes in healthcare service claims can serve as health deficit variables. In particular, the claim-based frailty index (CFI) developed by Kim and colleagues was designed to approximate a survey-based deficit accumulation index and was found to be associated with a higher risk of adverse outcomes and healthcare utilization after adjustment for demographics and a multimorbidity index.6,11
To determine the association of the frailty phenotype with subsequent total direct healthcare costs and utilization in community-dwelling older men, we used a unique longitudinal data set comprised of 1,514 men (mean age 79.3 years) participating in the Year 7 (Y7) examination of the Osteoporotic Fractures in Men (MrOS) Study who were linked to their Medicare claims data. Of importance, we evaluated whether any associations persisted after considering demographics, multimorbidity, cognitive function, functional limitations and the Kim CFI.
METHODS
Study Population and Linkage to Inpatient Claims
We studied participants enrolled in MrOS, a prospective cohort study of community-dwelling older men.12,13 From 2000 to 2002, 5,994 men ≥65 years old and able to walk unassisted were recruited for participation from six geographic areas in the US. Detailed study information may be found at the MrOS Online website (http://mrosdata.sfcc-cpmc.net). Human subjects review committees at each participating institution reviewed and approved the study. Each participant provided written informed consent.
There were 3,601 men from the original cohort who completed a Y7 in-clinic examination including assessment of the frailty phenotype (Supplementary Figure S1). Of these men, the analytic cohort included 1,514 men who were also enrolled in the Medicare Fee-For-Service (FFS) program (Parts A and B [and not Part C, Medicare Advantage]) from 12 months prior to the Y7 examination until 36 months following the Y7 examination (or up until death within this period).
Measurements
Participants were asked about education, smoking status and physical activity. Depressive symptoms were evaluated using the Geriatric Depression Scale.14 Cognitive function was assessed using the Modified Mini-Mental State Exam (3MS).15 Tests of physical performance included grip strength (Jamar handheld dynamometer16) and usual gait speed (average speed at usual pace in 2 trials over a 6 m course). Body weight and height were measured; body mass index (BMI) was calculated. Men were asked if they had difficulty performing any of five instrumental activities of daily living (IADL) (see footnote Table 1). Functional limitations were categorized as none, 1 or ≥2 IADL impairments.
Table 1.
Characteristics of Participants by Category of Frailty Phenotype
| Overall | Robust | Pre-frail | Frail | ||
|---|---|---|---|---|---|
| Characteristica | N=1514 | N=429 | N=886 | N=199 | P |
| Age, years, mean (SD) | 79.3 (5.17) | 78.1 (4.73) | 79.0 (4.98) | 83.0 (5.26) | <0.001 |
| White race, n (%) | 1394 (92.1) | 394 (91.8) | 810 (91.4) | 190 (95.5) | 0.16 |
| Ever smoker, n (%) | 899 (59.4) | 244 (56.9) | 526 (59.4) | 129 (64.8) | 0.17 |
| Years of Education, n (%) | <0.001 | ||||
| High school or less | 255 (16.8) | 52 (12.1) | 148 (16.7) | 55 (27.6) | |
| College/grad school | 1259 (83.2) | 377 (87.9) | 738 (83.3) | 144 (72.4) | |
| Multimorbidityb, n (%) | <0.001 | ||||
| None (0-1 conditions) | 351 (23.2) | 137 (31.9) | 185 (20.9) | 29 (14.6) | |
| Mild (2-4 conditions) | 663 (43.8) | 199 (46.4) | 401 (45.3) | 63 (31.7) | |
| At least moderate (≥5 conditions) | 500 (33.0) | 93 (21.7) | 300 (33.9) | 107 (53.8) | |
| GDS score (0-15), mean (SD) | 1.8 (2.06) | 0.6 (0.86) | 2.0 (1.91) | 3.6 (2.77) | <0.001 |
| 3MS (0-100), mean (SD) | 92.6 (6.53) | 93.7 (5.57) | 92.9 (6.17) | 89.2 (8.63) | <0.001 |
| # IADL impairmentsc (0-5), mean (SD) | 0.4 (0.98) | 0.1 (0.30) | 0.4 (0.84) | 1.6 (1.56) | <0.001 |
| # IADL impairmentsc (0-5), n (%) | <0.001 | ||||
| 0 | 1167 (77.1) | 408 (95.1) | 690 (77.9) | 69 (34.7) | |
| 1 | 179 (11.8) | 15 (3.5) | 123 (13.9) | 41 (20.6) | |
| ≥2 | 168 (11.1) | 6 (1.4) | 73 (8.2) | 89 (44.7) | |
| Kim CFId (0-1) | |||||
| Median (IQR) | 0.13 (0.10-0.17) | 0.12 (0.10-0.15) | 0.13 (0.11-0.17) | 0.18 (0.13-0.23) | |
| Mean (SD) | 0.14 (0.05) | 0.13 (0.04) | 0.14 (0.05) | 0.19 (0.07) | <0.001 |
| Body mass index, mean (SD) | 27.0 (3.75) | 26.4 (3.17) | 27.4 (3.75) | 26.7 (4.65) | <0.001 |
| Total annual healthcare costs, USD | |||||
| Median (IQR) | $3,681 (1,686-9,626) | $2,695 (1,347-6,295) | $3,577 (1,672-8,776) | $10,606 (4,120-27,244) | |
| Mean (SD) | $9,496 (18,219) | $5,707 (8,800) | $8,964 (18,156) | $20,027 (27,419) | <0.001 |
| Incident hospitalization, n (%) | 631 (41.7) | 136 (31.7) | 358 (40.4) | 137 (68.8) | <0.001 |
| Incident SNF stay, n (%) | 147 (9.7) | 19 (4.4) | 80 (9.0) | 48 (24.1) | <0.001 |
| Annual outpatient costs, USD | |||||
| Median (IQR) | $2,519 (1,399-4,192) | $2,126 (1,290-3,329) | $2,479 (1,418-4,192) | $3,673 (2,198-5,620) | |
| Mean (SD) | $3,442 (3,916) | $2,916 (3,373) | $3,305 (3,436) | $5,187 (6,005) | <0.001 |
| Died during follow-up, n (%) | 139 (9.2) | 15 (3.5) | 59 (6.7) | 65 (32.7) | <0.001 |
Note: GDS, Geriatric Depression Scale; 3MS, Modified Mini Mental State Examination; IADL, instrumental activities of daily living; CFI, claims-based frailty index; IQR, interquartile range; USD, U.S. 2018 dollars; SNF, skilled nursing facility
Participant characteristics assessed at MrOS Year 7 examination; total costs, hospitalizations, SNF stays, and outpatient care costs ascertained during 36 month period after MrOS Year 7 examination
Multimorbidity quantified using diagnoses in inpatient and outpatient claims data
Participants were queried about the following: difficulty walking 2-3 blocks on level ground, climbing up 10 steps without resting, doing heavy housework such as scrubbing floors or washing windows, preparing own meals, and doing own shopping for groceries or clothes
Kim CFI calculated using diagnosis and procedure codes in healthcare services claims in Medicare files in the year prior to the MrOS Year 7 examination
Multimorbidity was ascertained with count summarizing the presence or absence of each of 27 conditions selected by the CMS Chronic Conditions Data Warehouse (CCW)17 to facilitate studies of chronic medical conditions in the Medicare population.18 Existing CCW algorithms were used to identify the presence or absence of each condition using diagnosis codes in Medicare inpatient and outpatient files in the reference period prior to the Y7 examination. Multimorbidity was categorized as 0-1 condition, 2-4 conditions or ≥5 conditions. The Kim CFI6 that approximates the deficit accumulation index9,10 was calculated using diagnosis and procedure codes in Medicare healthcare services claims files in the year prior to the Y7 examination.
Frailty Phenotype
The frailty phenotype was operationalized using criteria similar to those proposed by Fried and colleagues1:
Shrinking: weight loss of ≥5% or ≥10 lbs between Y5 and Y7 examinations (mean 2.2 years between examinations) or BMI <18.5 kg/m2 at the Y7 examination.
Weakness: Y7 grip strength <32 kg.19
Poor energy: answered “no” to the question “Do you feel full of energy?” on the Y7 Geriatric Depression Scale.
Slowness: Y7 gait speed <0.8 m/s20,21 or use of a walking aid.
Low physical activity: reporting never walking for exercise and not engaging in moderate or vigorous activity on Y7 questionnaire.22
Men were robust if no frailty components were present, pre-frail if 1 or 2 components were present, and frail if ≥3 components were present.
Outcome Measures
The primary outcome was annualized total direct healthcare costs for the 36 months following the Y7 examination. Total costs were calculated as the sum of costs for acute hospital stays, skilled nursing facility (SNF) stays paid under Medicare part A, inpatient rehabilitation facility (IRF) stays, outpatient care, durable medical equipment (DME) and home healthcare for that time period. Acute hospital stays, SNF stays, and IRF stays were identified in the Medical Provider Analysis and Review (MedPAR) file. Standardized costs for acute short hospital stays, SNF stays and IRF stays were estimated using a previously published and validated method.23,24 Standardized costs for ambulatory care services were based on the allowable charges in the Carrier, Outpatient, DME and Home Health Care Medicare claims files.25 The costs of all units of utilization were adjusted for healthcare cost inflation to U.S. 2018 dollars.23
Statistical Analysis
Generalized linear models (GLMs) were used to estimate the association of the Y7 frailty phenotype and each individual frailty component with annualized total direct healthcare costs (primary outcome) over the subsequent 36 months. Gamma distributions with log links were chosen based on Modified Park26 and Pregibon link tests.27 Logistic models were used to estimate the associations of the frailty phenotype with risks of ≥1 hospitalization and ≥1 SNF stay. Robust men were the referent group.
Base models included age, race and study enrollment site. Potential confounders (Table 1) were screened for inclusion in multivariable models. Candidate covariates were included in multivariable models as confounders if they were associated with frailty phenotype and were independently related to total healthcare costs after adjustment for age, race, site and frailty phenotype. Initially, multivariable models were further adjusted for multimorbidity and cognitive function. To determine if the association of the frailty phenotype with outcomes was explained by greater self-reported functional limitations among pre-frail and frail men, IADL limitations was then added to multivariable models. We also further adjusted multivariable models for the Kim CFI to determine if any association was independent of a claims-based measure of frailty. Finally, models were simultaneously adjusted for demographics, multimorbidity, cognitive function, functional limitations and the Kim CFI. Since healthcare utilization is higher during the final few months of life28 and frailty may be a marker of imminent mortality, we also performed sensitivity analyses for total costs excluding the 139 (9.2%) men who died during the 36-month follow-up period.
RESULTS
The study cohort at Y7 included 1,514 community-dwelling men with mean (SD) age of 79.3 (5.2) years (Table 1). Among these men, 199 (13.1%) were classified as frail and 886 (58.5%) were classified as pre-frail using the phenotypic definition. Frail men had a greater burden of co-existing medical conditions; 21.7% of robust men, 33.9% of pre-frail men and 53.8% of frail men had 5 or more conditions. Frail men were also likely to report functional limitations; 1.4% of robust men, 8.2% of pre-frail men and 44.7% of frail men reported 2 or more limitations. Mean Kim CFI was 0.13 among men classified as robust by the phenotypic definition increasing to 0.19 among men classified as frail by the phenotypic approach.
Among the overall cohort, the median (interquartile range [IQR]) annualized total healthcare costs (2018 U.S. dollars) were $3,681 (1,686-9,626) and mean (SD) annualized costs were $9,496 (18,219) during the 36 months following Y7. A total of 631 men (41.7%) had at least 1 hospitalization, 147 (9.7%) had at least 1 SNF stay and 139 (9.2%) died.
Characteristics (including the distribution of the frailty phenotype) of the men in the analytical cohort were similar to those of the MrOS men attending the Y7 examination who were excluded from analyses because they were not enrolled in a FFS plan (Supplementary Table S1). While differences in race, educational status and 3MS score were statistically significant, these differences were small in magnitude.
Association of the Frailty Phenotype with Total Healthcare Costs
Mean and median annualized total healthcare costs in the 36 months after Y7 exam were higher with greater degree of frailty at Y7 (Table 1). Mean (SD) costs increased from $5,707 (8,800) among robust men to $8,964 (18,156) among pre-frail men to $20,027 (27,419) among frail men (p<0.001). The presence of frailty was also associated with a higher likelihood of incurring very high costs; the proportion of men with costs in the highest decile ($22,174-$278,300) was 4.4% among robust men, 8.6% among pre-frail men and 28.6% among frail men (Figure 1).
Figure 1.
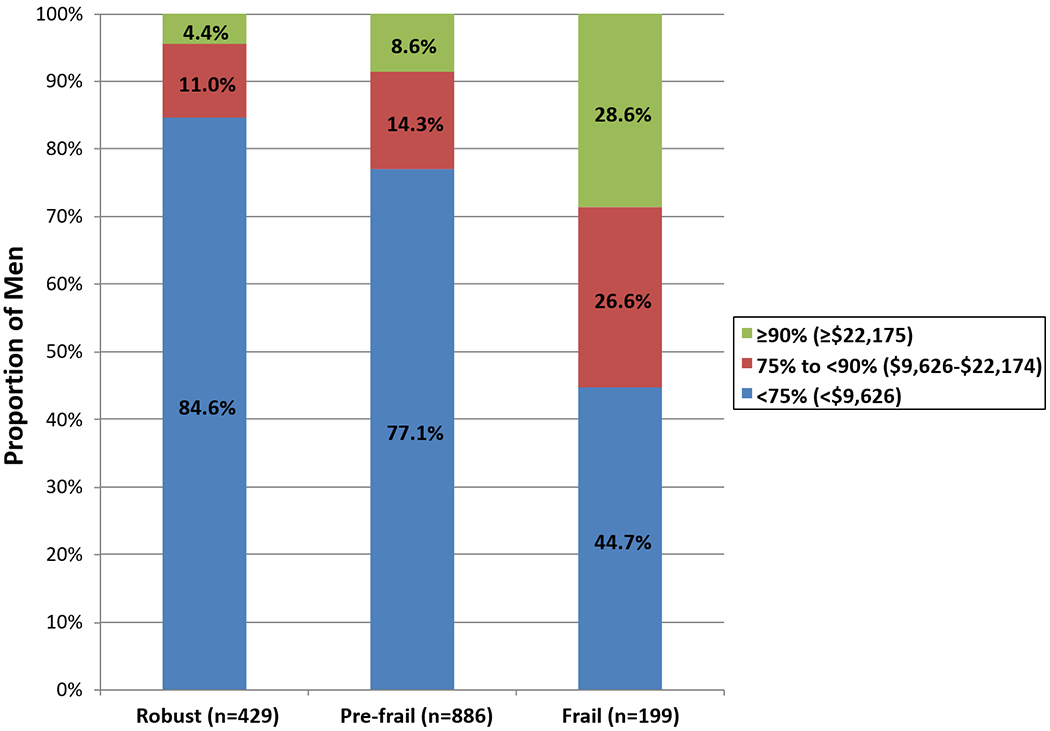
Distribution of Total Healthcare Costs According to Category of Frailty Phenotype
After adjustment for age, race and enrollment site, mean total costs were 2.7-fold higher among frail vs. robust men (cost ratio [CR] 2.72 [95% CI 2.19-3.37]) and 1.4-fold higher among pre-frail vs. robust men (CR 1.42 [95% CI 1.23-1.64]) (Table 2). After further accounting for multimorbidity and cognition, these associations were slightly attenuated but remained significant (CR 2.35 [95% CI 1.88-2.93] among frail vs. robust men and 1.28 [95% CI 1.11-1.48] among pre-frail vs. robust men). The associations were in part (but not entirely) mediated by poorer self-reported functional status among men in these phenotypic categories. After further consideration of functional limitations, costs were approximately 2-fold higher among frail vs. robust men (CR 1.99 [95% CI 1.56-2.52]) and 1.2-fold higher among pre-frail vs. robust men (CR 1.20 [95% CI 1.04-1.38]). Further adjustment for the Kim CFI did not substantially alter the associations of pre-frailty and frailty with total costs (CR 1.87 [95% CI 1.47-2.39] among frail vs. robust men and 1.18 [95% CI 1.02-1.36] among pre-frail vs. robust men).
Table 2.
Association of Frailty Phenotype with Total Healthcare Costs
| Total healthcare costs |
||
|---|---|---|
| Frailty phenotype | Cost ratio (95% CI) | P |
| Base modela | ||
| Robust | 1.00 (referent) | <0.001 |
| Pre-frail | 1.42 (1.23-1.64) | |
| Frail | 2.72 (2.19-3.37) | |
| Multivariable (MV) modelb | ||
| Robust | 1.00 (referent) | <0.001 |
| Pre-frail | 1.28 (1.11-1.48) | |
| Frail | 2.35 (1.88-2.93) | |
| MV model + functional limitationsc | ||
| Robust | 1.00 (referent) | <0.001 |
| Pre-frail | 1.20 (1.04-1.38) | |
| Frail | 1.99 (1.56-2.52) | |
| MV model + Kim CFI | ||
| Robust | 1.00 (referent) | <0.001 |
| Pre-frail | 1.23 (1.07-1.42) | |
| Frail | 2.07 (1.65-2.60) | |
| MV model + functional limitations + Kim CFI | ||
| Robust | 1.00 (referent) | <0.001 |
| Pre-frail | 1.18 (1.02-1.36) | |
| Frail | 1.87 (1.47-2.39) | |
Note: CFI, claims-based frailty index
adjusted for age, race, and site
adjusted for age, race, site, multimorbidity burden, and cognitive function
functional limitations defined by number of IADL impairments
In contrast, total costs in the fully adjusted model were about 1.4-fold higher (CR 1.37 [95% CI 1.17-1.61]) among men with 2-4 chronic medical conditions and 1.7-fold higher (CR 1.73 [95% CI 1.43-2.11]) among men with at least 5 conditions vs. men without multimorbidity. Costs were nearly 1.4-fold higher among men with 1 vs. no functional limitations (CR 1.35 [95% CI 1.11-1.65]), but costs among men with ≥2 limitations did not differ from that among men with no limitations (CR 1.19 [95% CI 0.96-1.49]). Each 1 SD increase in the Kim CFI was associated with 20% increase in total costs (CR 1.19 [95% CI 1.10-1.28]).
When analyses were restricted to the 1375 men (90.8%) who survived the entire 36 month follow-up period, the frailty phenotype remained associated with higher subsequent total costs after consideration of demographics, multimorbidity and cognition, but the relationships were somewhat reduced in magnitude compared with those for the entire cohort (CR 1.17 [95% CI 1.02-1.33] for pre-frail vs. robust survivors and 1.64 [95% CI 1.31-2.05] for frail vs. robust survivors). The association of phenotypic frailty with costs persisted among survivors after additional consideration of functional limitations (CR 1.34 [95% CI 1.05-1.70 for frail vs. robust men] or the Kim CFI (CR 1.46 [95% CI 1.16-1.83 for frail vs. robust men]).
Association of the Frailty Phenotype with Hospitalization and Skilled Nursing Facility Stay
After consideration of demographics, multimorbidity and cognition, the frailty phenotype was associated with a higher risk of subsequent hospitalization (odds ratio [OR] 2.62 [95% CI 1.75-3.91] for frail vs. robust men and OR 1.20 [95% CI 0.92-1.55] for pre-frail vs. robust men) (Table 3). After further adjustment for functional limitations and the Kim CFI, a 1.8-fold higher risk of hospitalization among frail vs. robust men remained. Frail and pre-frail men had higher odds of subsequent SNF stay after consideration of demographics, multimorbidity and cognition (OR 3.36 [95% CI 1.83-6.20] among frail vs. robust men and 1.76 [95% CI 1.04-2.99] among pre-frail vs. robust men). These associations were not substantially altered by further adjustment for the Kim CFI, but were attenuated and not significant after further consideration of functional limitations.
Table 3.
Associations of Frailty Phenotype with Odds of Hospitalization and SNF Stay
| ≥1 Acute hospital stay | ≥1 SNF stay | |||
|---|---|---|---|---|
| Frailty phenotype | Odds ratio (95% CI) | P | Odds ratio (95% CI) | P |
| Base modela | ||||
| Robust | 1.00 (referent) | <0.001 | 1.00 (referent) | <0.001 |
| Pre-frail | 1.35 (1.05-1.73) | 1.93 (1.14-3.25) | ||
| Frail | 3.39 (2.31-4.97) | 4.17 (2.29-7.60) | ||
| Multivariable (MV) modelb | ||||
| Robust | 1.00 (referent) | <0.001 | 1.00 (referent) | <0.001 |
| Pre-frail | 1.20 (0.92-1.55) | 1.76 (1.04-2.99) | ||
| Frail | 2.62 (1.75-3.91) | 3.36 (1.83-6.20) | ||
| MV model + functional limitationsc | ||||
| Robust | 1.00 (referent) | 0.006 | 1.00 (referent) | 0.29 |
| Pre-frail | 1.09 (0.84-1.42) | 1.40 (0.81-2.41) | ||
| Frail | 1.98 (1.28-3.06) | 1.72 (0.87-3.41) | ||
| MV model + Kim CFI | ||||
| Robust | 1.00 (referent) | 0.001 | 1.00 (referent) | 0.016 |
| Pre-frail | 1.14 (0.88-1.48) | 1.65 (0.97-2.82) | ||
| Frail | 2.14 (1.42-3.24) | 2.54 (1.34-4.79) | ||
| MV model + functional limitations + Kim CFI | ||||
| Robust | 1.00 (referent) | 0.023 | 1.00 (referent) | 0.43 |
| Pre-frail | 1.06 (0.82-1.39) | 1.38 (0.80-2.37) | ||
| Frail | 1.79 (1.15-2.78) | 1.54 (0.77-3.07) | ||
Note: SNF, skilled nursing facility; CFI, claims-based frailty index
adjusted for age, race, and site
adjusted for age, race, site, multimorbidity burden, and cognitive function
functional limitations defined by number of IADL impairments
Associations of Individual Frailty Components with Total Healthcare Costs
Mean and median total healthcare costs were higher among men with a given frailty component compared to men without that specific component (Supplementary Table S2). Each frailty component was associated with higher subsequent annualized total costs in models accounting for demographics, multimorbidity and cognition (CR [95% CI] 1.52 [1.28-1.80] for shrinking, 1.20 [1.05-1.36] for poor energy, 1.79 [1.44-2.22]) for slowness, 1.52 [1.28-1.80] for weakness and 1.15 [1.00-1.31]) for low physical activity) (Table 4). After further consideration of functional limitations and the Kim CFI, shrinking (CR 1.42 [95% CI 1.20-1.68]), slowness (CR 1.35 [95% CI 1.06-1.72]) and weakness (CR 1.35 [95% CI 1.13-1.61]) were independently associated with higher total costs.
Table 4.
Association of Individual Frailty Components with Total Healthcare Costs
| Cost ratio (95% CI) |
|||||
|---|---|---|---|---|---|
| Frailty component | Base modela | Multivariable (MV) modelb | MV model + functional limitationsc | MV model + Kim CFI | MV model + functional limitations + Kim CFI |
| Shrinking | |||||
| Present (N=254) | 1.61 (1.36-1.90) | 1.52 (1.28-1.80) | 1.44 (1.22-1.71) | 1.46 (1.23-1.72) | 1.42 (1.20-1.68) |
| Absent | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Weakness | |||||
| Present (N=272) | 1.62 (1.37-1.92) | 1.52 (1.28-1.80) | 1.40 (1.17-1.66) | 1.41 (1.18-1.67) | 1.35 (1.13-1.61) |
| Absent | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Poor energy | |||||
| Present (N=742) | 1.35 (1.19-1.53) | 1.20 (1.05-1.36) | 1.11 (0.98-1.26) | 1.14 (1.01-1.30) | 1.09 (0.96-1.24) |
| Absent | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Slowness | |||||
| Present (N=147) | 2.01 (1.62-2.48) | 1.79 (1.44-2.22) | 1.45 (1.14-1.84) | 1.54 (1.24-1.92) | 1.35 (1.06-1.72) |
| Absent | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Low physical activity | |||||
| Present (N=528) | 1.26 (1.10-1.44) | 1.15 (1.00-1.31) | 1.00 (0.87-1.14) | 1.06 (0.93-1.21) | 0.97 (0.85-1.11) |
| Absent | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
Note: CFI, claims-based frailty index
adjusted for age, race, and site
adjusted for age, race, site, multimorbidity burden, and cognitive function
functional limitations defined by number of IADL impairments
DISCUSSION
Phenotypic pre-frailty and frailty in this cohort of older community-dwelling men were associated with higher subsequent total direct healthcare costs even after accounting for demographics, multimorbidity, cognition, functional limitations and a claims-based frailty indicator based on a deficit accumulation index. Of note, almost 3 in 10 frail men (and 1 in 10 pre-frail men) compared with 1 in 25 robust men were among the costliest 10% of individuals. Among frailty phenotype components, shrinking, slowness and weakness were each independently related to higher subsequent total costs. These findings suggest that assessment of the frailty phenotype or individual components of shrinkage, slowness or weakness may improve identification of older community-dwelling adults likely to require costly care and facilitate development and targeting of interventions aimed at reducing costs.
Few studies have determined associations of the frailty phenotype with healthcare costs in older community-dwelling populations. Our findings in men confirm and extend the results of our previous study of 2,150 older women (mean age 80.2 years)3 that reported that subsequent total direct healthcare expenditures were higher among women with phenotypic pre-frailty and frailty after accounting for demographics, multimorbidity, cognitive function and functional limitations. Greater evidence of frailty (defined by number of phenotypic components present) was associated with increased healthcare costs derived based on participant recall of healthcare use independent of age and multimorbidity in cross-sectional29 and longitudinal30 studies of German adults aged 57 to 84 years. A cross-sectional survey in 1284 French adults aged ≥65 years (that modified phenotypic criteria of slowness and weakness based on questionnaire contents) reported that pre-frailty and frailty had an incremental effect on ambulatory healthcare expenditures after adjustment for selected medical conditions and functional limitations.31 A prospective study of 830 Spanish adults ≥70 years32 reported that participants with pre-frailty and frailty defined by phenotypic criteria had higher subsequent hospital healthcare costs after consideration of demographics and a comorbidity index.
Each individual phenotypic frailty component was associated with higher subsequent total direct healthcare costs in this cohort of community-dwelling older men after adjustment for demographics, multimorbidity and cognition. After further consideration of functional limitations and a claims-based measure of deficit accumulation, associations of shrinking, slowness and weakness with higher total costs remained. These results are in general agreement with those of our prior study in older US women3 that found that shrinking, poor energy, slowness and low physical activity (but not weakness) were each associated with associated with higher subsequent total healthcare costs after consideration of demographics, multmorbidity and cognitive function. In contrast, a longitudinal study of German older adults30 reported that the onset of exhaustion (but not weight loss, slowness, weakness or low physical activity) was associated with an increase in total healthcare costs estimated based on self-reported healthcare use. Differences in results between US-based studies and the German investigation may in part reflect differences in criteria used to define frailty components, methods used to estimate healthcare costs, adjustment for potential confounders, or healthcare systems.
Phenotypic frailty in this cohort of community-dwelling older men was an independent risk factor for subsequent hospitalization after accounting for demographics, multimorbidity, cognitive function, self-reported functional limitations and a claims-based measure of deficit accumulation. Several prior studies in unselected community-dwelling older adults have reported associations of phenotypic frailty with past hospitalization.1,22,33–35 However, retrospective studies cannot establish the temporality of this relationship because admission to an acute care hospital may also result in the onset of frailty. A previous longitudinal study of older adults residing in Boston36 found that pre-frail and frail participants were more likely to report hospitalization during the subsequent 10 months, but only accounted for demographics and cardiovascular risk factors. Our results confirm and extend findings from our previous investigation in women3 that reported an association of phenotypic frailty with risk of subsequent hospitalization after consideration of demographics, multimorbidity, cognitive function and functional limitations.
Among this cohort of community-dwelling men, associations of phenotypic pre-frailty and frailty with higher subsequent post-acute care utilization were explained by greater self-reported functional limitations among pre-frail and frail men. In contrast, self-reported functional limitations did not explain associations of phenotypic pre-frailty and frailty with risk of a SNF stay in our previous study of older women.3 Reasons for these discrepant results are uncertain but may include temporal differences in the utilization of post-acute care facilities between studies37,38 or sex differences (higher prevalence of frailty among women2 and under-reporting of functional limitations among men39,40).
Our results suggest that phenotypic pre-frailty and frailty are risk factors for higher subsequent total healthcare costs in older community-dwelling adults above and beyond that explained by demographics, burden of chronic medical conditions, cognitive impairment, self-reported functional limitations and a claims-based measure of deficit accumulation. Thus, measurement of the phenotype or selected individual components such slow gait may more accurately identify older community-dwelling individuals who are at higher risk of subsequent healthcare use. While it has been suggested that health systems might rely on a claims-based frailty indicator to select a vulnerable population for targeted resource-intensive treatments11, our findings suggest that assessment of the frailty phenotype is capturing characteristics distinct from multimorbidity to a greater degree than the Kim CFI that approximates the deficit accumulation index. Thus, assessment of the frailty phenotype may be necessary to identify high risk older adults without overt disability or severe frailty still living in the community to better inform appropriate selection and targeting of interventions and resources aimed at reducing costs in this patient population. Additional research is warranted to determine if frailty phenotype assessment in the clinical practice setting is feasible, will better direct shared clinical-decision making regarding targeted treatments aimed at reducing subsequent healthcare burden41 and has a favorable cost/benefit ratio.
This study has several strengths including its prospective design; comprehensive participant characteristics available in cohort study data; linkage of participants to their Medicare claims to determine co-existing chronic medical conditions, estimate accumulated deficits and quantify subsequent healthcare expenditures and utilization; and consideration of traditional predictors of healthcare costs. However, this study has limitations. The cohort was comprised of relatively well-functioning community-dwelling predominantly white older men. Results are similar to previous findings in a similar cohort of women3, but may not be generalizable to other racial/ethnic groups or those with overt disability or severe frailty such as nursing home residents. However, community-dwelling older adults without frank disability or advanced frailty may be most amenable to interventions aimed at lowering subsequent healthcare burden. Future studies are warranted to replicate our findings in other patient populations. Cost and utilization data were limited to participants enrolled in FFS plans. However, characteristics of participants who were excluded based on not participating in FFS were similar to those included. Furthermore, evidence from the recent decade42 indicates that Medicare FFS enrollees and enrollees in Medicare Advantage have similar healthcare expenditures. Our analyses expressed the frailty phenotype using criteria similar to those proposed by Fried and colleagues, but we used population-independent cutoffs for identification of weakness, slowness and low physical activity. Other instruments have been developed to operationalize the construct of the frailty phenotype. Thus, future research is needed to standardize and cross-validate frailty instruments and determine whether results are consistent when the frailty phenotype is assessed using simpler instruments43 that are feasible to use in the time-limited busy clinical practice setting. Finally, we utilized a comprehensive measure of co-existing chronic medical conditions developed for use in the Medicare population and a commonly cited claims-based frailty indicator. However, alternative claims-based measures of multimorbidity44–46 and frailty4,5,7,8 have been developed.
In conclusion, older community-dwelling men with phenotypic frailty and those with pre-frailty are at increased risk of higher subsequent healthcare expenditures, even after accounting for conventional predictors of healthcare costs. These findings suggest that assessment of the frailty phenotype or selected components may improve identification of older community-dwelling adults at risk of costly, intensive care to better facilitate targeting of interventions aimed at reducing future healthcare burden.
Supplementary Material
Supplementary Figure S1. Participant Flow Diagram
Supplementary Table S1. Characteristics by Medicare Fee-For-Service Enrollment Status
Supplementary Table S2. Healthcare Costs Among Women With or Without Specific Frailty Components
ACKNOWLEDGMENTS
Conflict of Interest
Dr. Ensrud has received grant support from the NIH (and supporting agencies) grant as listed under Funding Sources on the title page. Dr. Cawthon has consulted with BioAge Labs, and has received research support to her institution from Nestle and Abbott, both for work outside of this project.
Source of Funding: The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute on Aging (NIA), the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Center for Advancing Translational Sciences (NCATS), and NIH Roadmap for Medical Research under the following grant numbers: U01 AG027810, U01 AG042124, U01 AG042139, U01 AG042140, U01 AG042143, U01 AG042145, U01 AG042168, U01 AR066160, and UL1 TR000128.
Sponsor’s Role: The funding agencies had no direct role in the conduct of the study; the collection, management, analyses and interpretation of the data; or preparation or approval of the manuscript. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs or the United States government.
REFERENCES
- 1.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–156. doi: 10.1093/gerona/56.3.m146 [DOI] [PubMed] [Google Scholar]
- 2.Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. 2019;394(10206):1365–1375. doi: 10.1016/S0140-6736(19)31786-6 [DOI] [PubMed] [Google Scholar]
- 3.Ensrud KE, Kats AM, Schousboe JT, et al. Frailty Phenotype and Healthcare Costs and Utilization in Older Women. J Am Geriatr Soc. 2018;66(7):1276–1283. doi: 10.1111/jgs.15381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clegg A, Bates C, Young J, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing. 2016;45:353–360. doi: 10.1093/ageing/afw039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Faurot KR, Jonsson FM, Pate V, et al. Using claims data to predict dependency in activities of daily living as a proxy for frailty. Pharmacoepidemiol Drug Saf. 2015;24:59–66. doi: 10.1002/pds.3719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim DH, Schneeweiss S, Glynn RJ, Lipsitz LA, Rockwood K, Avorn J. Measuring frailty in Medicare data: development and validation of a claims-based frailty index. J Gerontol A Biol Sci Med Sci. 2018;73(7):980–987. doi: 10.1093/gerona/glx229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Orkaby AR, Nussbaum L, Ho YL, et al. The burden of frailty among U.S. veterans and its association with mortality, 2002–2012. J Gerontol A Biol Sci Med Sci. 2019;74(8):1257–1264. doi: 10.1093/gerona/gly232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Segal JB, Chang H-Y, Du Y, Walston JD, Carlson MC, Varadhan R. Development of a claims-based frailty indicator anchored to a well-established frailty phenotype. Med Care. 2017;55:716–722. doi: 10.1097/MLR.0000000000000729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62:722–727. [DOI] [PubMed] [Google Scholar]
- 10.Rockwood K Conceptual models of frailty: accumulation of deficits. Can J Cardiol. 2016;32(9):1046–1050. doi: 10.1016/j.cjca.2016.03.020 [DOI] [PubMed] [Google Scholar]
- 11.Kim DH, Glynn RJ, Avorn J, et al. Validation of a Claims-Based Frailty Index Against Physical Performance and Adverse Health Outcomes in the Health and Retirement Study. J Gerontol A Biol Sci Med Sci. 2019;74(8):1271–1276. doi: 10.1093/gerona/gly197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blank JB, Cawthon PM, Carrion-Petersen ML, et al. Overview of recruitment for the osteoporotic fractures in men study (MrOS). Contemp Clin Trials. 2005;26(5):557–568. doi: 10.1016/j.cct.2005.05.005 [DOI] [PubMed] [Google Scholar]
- 13.Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study--a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26(5):569–585. doi: 10.1016/j.cct.2005.05.006 [DOI] [PubMed] [Google Scholar]
- 14.Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clin Gerontol. 1986;5(1-2):165–173. doi: 10.1300/J018v05n01_09 [DOI] [Google Scholar]
- 15.McDowell I, Kristjansson B, Hill GB, Hébert R. Community screening for dementia: the Mini Mental State Exam (MMSE) and Modified Mini-Mental State Exam (3MS) compared. J Clin Epidemiol. 1997;50(4):377–383. doi: 10.1016/s0895-4356(97)00060-7 [DOI] [PubMed] [Google Scholar]
- 16.Härkönen R, Harju R, Alaranta H. Accuracy of the Jamar dynamometer. J Hand Ther. 1993;6(4):259–262. doi: 10.1016/s0894-1130(12)80326-7 [DOI] [PubMed] [Google Scholar]
- 17.Centers for Medicare & Medicaid Services. Chronic Conditions Data Warehouse. www.ccwdata.org. www.ccwdata.org/web/guest/home. Published 2020. Accessed January 15, 2020. [Google Scholar]
- 18.Schneider KM, O’Donnell BE, Dean D. Prevalence of multiple chronic conditions in the United States’ Medicare population. Health Qual Life Outcomes. 2009;7:82. doi: 10.1186/1477-7525-7-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alley DE, Shardell MD, Peters KW, et al. Grip strength cutpoints for the identification of clinically relevant weakness. J Gerontol A Biol Sci Med Sci. 2014;69(5):559–566. doi: 10.1093/gerona/glu011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abellan van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13(10):881–889. doi: 10.1007/s12603-009-0246-z [DOI] [PubMed] [Google Scholar]
- 21.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412–423. doi: 10.1093/ageing/afq034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bandeen-Roche K, Seplaki CL, Huang J, et al. Frailty in older adults: a nationally representative profile in the United States. J Gerontol A Biol Sci Med Sci. 2015;70:1427–1434. doi: 10.1093/gerona/glv133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schousboe JT, Paudel ML, Taylor BC, et al. Estimation of standardized hospital costs from Medicare claims that reflect resource requirements for care: impact for cohort studies linked to Medicare claims. Health Serv Res. 2014;49(3):929–949. doi: 10.1111/1475-6773.12151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schousboe JT, Paudel ML, Taylor BC, et al. Pre-fracture individual characteristics associated with high total health care costs after hip fracture. Osteoporos Int. 2017;28(3):889–899. doi: 10.1007/s00198-016-3803-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schousboe JT, Paudel ML, Taylor BC, et al. Estimating True Resource Costs of Outpatient Care for Medicare Beneficiaries: Standardized Costs versus Medicare Payments and Charges. Health Serv Res. 2016;51(1):205–219. doi: 10.1111/1475-6773.12318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20:461–494. [DOI] [PubMed] [Google Scholar]
- 27.Pregibon D Goodness of link tests for generalized linear models. J R Stat Soc Ser C Appl Stat. 1980;29(1):15–24. [Google Scholar]
- 28.Riley GF, Lubitz JD. Long-term trends in Medicare payments in the last year of life. Health Serv Res. 2010;45:565–576. doi: 10.1111/j.1475-6773.2010.01082.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bock JO, Konig HH, Brenner H, et al. Associations of frailty with health care costs--results of the ESTHER cohort study. BMC Health Serv Res. 2016;16:128. doi: 10.1186/s12913-016-1360-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hajek A, Bock JO, Saum KU, et al. Frailty and healthcare costs-longitudinal results of a prospective cohort study. Age Ageing. 2018;47:233–241. doi: 10.1093/ageing/afx157 [DOI] [PubMed] [Google Scholar]
- 31.Sirven N, Rapp T. The cost of frailty in France. Eur J Health Econ. 2017;18(2):243–253. doi: 10.1007/s10198-016-0772-7 [DOI] [PubMed] [Google Scholar]
- 32.García-Nogueras I, Aranda-Reneo I, Peña-Longobardo LM, Oliva-Moreno J, Abizanda P. Use of Health Resources and Healthcare Costs associated with Frailty: The FRADEA Study. J Nutr Health Aging. 2017;21(2):207–214. doi: 10.1007/s12603-016-0727-9 [DOI] [PubMed] [Google Scholar]
- 33.Ilinca S, Calciolari S. The patterns of health care utilization by elderly Europeans: frailty and its implications for health systems. Health Serv Res. 2015;50:305–320. doi: 10.1111/1475-6773.12211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lahousse L, Maes B, Ziere G, et al. Adverse outcomes of frailty in the elderly: the Rotterdam Study. Eur J Epidemiol. 2014;29:419–427. doi: 10.1007/s10654-014-9924-1 [DOI] [PubMed] [Google Scholar]
- 35.Vaingankar JA, Chong SA, Abdin E, et al. Prevalence of frailty and its association with sociodemographic and clinical characteristics, and resource utilization in a population of Singaporean older adults. Geriatr Gerontol Int. 2017;17:1444–1454. doi: 10.1111/ggi.12891 [DOI] [PubMed] [Google Scholar]
- 36.Kiely DK, Cupples LA, Lipsitz LA. Validation and comparison of two frailty indexes: the MOBILIZE Boston Study. J Am Geriatr Soc. 2009;57:1532–1539. doi: 10.1111/j.1532-5415.2009.02394.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burke RE, Juarez-Colunga E, Levy C, Prochazka AV, Coleman EA, Ginde AA. Rise of post-acute care facilities as a discharge destination of US hospitalizations. JAMA Intern Med. 2015;175:295–296. doi: 10.1001/jamainternmed.2014.6383 [DOI] [PubMed] [Google Scholar]
- 38.Chandra A, Dalton MA, Holmes J. Large increases in spending on postacute care in Medicare point to the potential for cost savings in these settings. Health Aff (Millwood). 2013;32:864–872. doi: 10.1377/hlthaff.2012.1262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jindai K, Nielson CM, Vorderstrasse BA, Quinones AR. Multimorbidity and functional limitations among adults 65 or older, NHANES 2005-2012. Prev Chronic Dis. 2016;13:E151. doi: 10.5888/pcd13.160174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zunzunegui MV, Alvarado BE, Guerra R, Gomez JF, Ylli A, Guralnik JM. The mobility gap between older men and women: the embodiment of gender. Arch Gerontol Geriatr. 2015;61:140–148. doi: 10.1016/j.archger.2015.06.005 [DOI] [PubMed] [Google Scholar]
- 41.Bibas L, Levi M, Bendayan M, Mullie L, Forman DE, Afilalo J. Therapeutic interventions for frail elderly patients: part I. Published randomized trials. Prog Cardiovasc Dis. 2014;57(2):134–143. doi: 10.1016/j.pcad.2014.07.004 [DOI] [PubMed] [Google Scholar]
- 42.Newhouse JP, Price M, Huang J, McWilliams JM, Hsu J. Steps to reduce favorable risk selection in medicare advantage largely succeeded, boding well for health insurance exchanges. Health Aff (Millwood). 2012;31(12):2618–2628. doi: 10.1377/hlthaff.2012.0345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ensrud KE, Ewing SK, Taylor BC, et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med. 2008;168:382–389. doi: 10.1001/archinternmed.2007.113 [DOI] [PubMed] [Google Scholar]
- 44.Chen J, Ellis RP, Toro KH, Ash AS. Mispricing in the medicare advantage risk adjustment model. Inquiry. 2015;52. doi: 10.1177/0046958015583089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Noyes K, Liu H, Temkin-Greener H. Medicare capitation model, functional status, and multiple comorbidities: model accuracy. Am J Manag Care. 2008;14:679–690. [PMC free article] [PubMed] [Google Scholar]
- 46.Perkins AJ, Kroenke K, Unützer J, et al. Common comorbidity scales were similar in their ability to predict health care costs and mortality. J Clin Epidemiol. 2004;57(10):1040–1048. doi: 10.1016/j.jclinepi.2004.03.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure S1. Participant Flow Diagram
Supplementary Table S1. Characteristics by Medicare Fee-For-Service Enrollment Status
Supplementary Table S2. Healthcare Costs Among Women With or Without Specific Frailty Components


