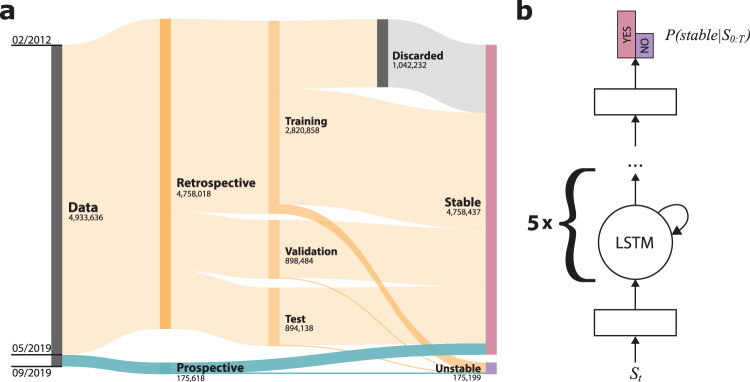
Fig. 2. Data organization and model architecture.
The complete de-identified retrospective and prospective data set contains 2,318,506 inpatient hospital admissions and 26,201,030 records of vital signs (VSs) between 2012 and 2019, yielding 4,933,636 VS input sequences used by our model (shown). The retrospective data set included all data through April 2019, while the prospective collection ranged from May to August 2019. Unrealistic, possibly mistyped VS values and records with any missing data after imputation were discarded. We split the retrospective data into training (70%), validation (15%), and test (15%) sets by patient visit, so the sequences drawn from one visit were only included in one of the groups. Some training data sequences with stable outcomes were discarded to balance the positive and negative cases (a). We used a deep recurrent neural network with two dense layers and five successive long short-term memory (LSTM) cells. After receiving a sequence of samples S0:T, the model predicts the probability of the patient becoming unstable during the night. We inserted a batch norm and dropout layer before the last fully connected layer (b).