Abstract
DeVilbiss et al. (Am J Epidemiol. 2020;189(10):998–1010) have taken on the noble and worthy cause of improving diversity, inclusion, representation, and participation across the Society for Epidemiologic Research (SER) membership—a reflection/microcosm of society. The objective of this commentary is to underscore the importance of diversity and to offer initiative ideas, which should be centered around inequity stemming from the widespread historical and contemporary maldistribution of power (e.g., decision-making) and resources (e.g., funding) within institutions and organizations. Nonexhaustive strategies could include SER becoming an opportunity and information hub that helps to fill resource gaps. It is also recommended that SER leadership learn from existing associations and scientific initiatives to improve the culture of science in general by equitably incorporating policy, systems, and environmental interventions throughout the career spectrum. Examples include the provision of tools and incentives to address explicit or implicit biases, enhance mentoring skills, and remove predictable barriers (e.g., financial). Explicitly labeling diversity/inclusion efforts should be avoided, and the initiative should be evaluated based on impact rather than intent. Our fates are interconnected, and we can all help increase diversity, inclusion, representation, and participation to improve our science in hopes of equitably improving public health.
Keywords: diversity, inclusion, leadership, mentoring, social identification, social marginalization
Abbreviations
- NIH
National Institutes of Health
- SER
Society for Epidemiologic Research
Editor’s note: The opinions expressed in this article are those of the author and do not necessarily reflect the views of the American Journal of Epidemiology.
As mentioned by a Black male professional focus group participant (C.L.J., unpublished data, 2019):
The problem is that we believe diversity and inclusion are the same thing as equality and justice. And it’s not, right? This is the way that I think about it. Alright, so, one guy’s a vegan, one guy’s a vegetarian, and one guy eats everything. So, the vegan and the vegetarian go to the house of the guy who eats everything, and all he has is meat ’cause he eats meat. Well, everybody got an invite, everybody came to the table, everybody was ready to eat, but I don’t eat that; so, I still go hungry, but I’m at the table. So, you included me, you diversified your table, you did all of that, but there was no equality and there was no justice. I left and went hungry.
DeVilbiss et al. (1) assessed who is currently at the Society for Epidemiologic Research (SER) “table” and unsurprisingly revealed the racial homogeneity that is common across science, technology, engineering, and mathematics. Similar to the food analogy, who—in terms of social identity and lived experience—has and has not served as the executive chef at the SER? Who has owned the table and what are their explicit and implicit preferences? Who determined the invitees? What factors influenced whether invitees felt comfortable joining? What was on the menu of options, and were the offerings sufficient for everyone? Who came malnourished or starving, who had access to just enough nourishment to survive, and who was fed well enough to support elite athleticism (or innovative scholarship)? History informs the answers to these questions, and as the saying goes “if you are not at the table, then you are on the menu.”
IS SER (AND THE FIELD OF EPIDEMIOLOGY) SERVING WHAT EVERYONE WANTS TO CONSUME?
In 2008, Dr. Sherman James was the President of SER, and social determinants of health—my cup of tea—was the conference theme. As a budding epidemiologist, I was the proverbial kid in the candy store. The conference—aligned with the organization’s mission to “keep epidemiologists at the vanguard of scientific developments”—served everything I needed and wanted to consume. There was a smorgasbord of rigorous epidemiologic methods, inspiring and informative scientific content, and networking opportunities with peers, mid-career scientists, and approachable legends in the field. I volunteered so the registration fee was waived, and I shared one hotel room with numerous classmates. Otherwise, the nourishment I received from this meeting would have been inaccessible at a critical developmental period. I overcame structural and social barriers to participate in the meeting. Over the years, how many trainees have not?
AN EVIDENCE-BASED CASE FOR DIVERSITY AND INCLUSION
There is evidence that research teams with greater diversity of backgrounds ask different and broader scientific questions (2). These teams are also more creative and innovative, and they often come up with additional, better solutions to complex problems that enhance organizational outcomes related to performance and success (3). More diverse teams also promote and ensure fairness in our highly diverse nation (4). Additionally, our return on investment is lowered when scientists drop out of the workforce prematurely and less race- or sex/gender-based research is conducted (4). With implications for enhancing global economies, society should leverage the entire pool of intellectual capital by having a diverse scientific workforce, and SER is no exception (5).
As mentioned by DeVilbiss et al. (1), diversity involves a variety of educational backgrounds, personalities, life experiences, and physical abilities; the SER diversity and inclusion committee focused on underrepresented identity groups. Acknowledging that all can experience marginalization based on social identity and lived experience, this commentary focuses on diversity and inclusion based on race/ethnicity as an illustrative example given the historical and contemporary inequities faced by racial/ethnic minorities. Racial/ethnic minorities are not sufficiently represented at the “table” in scientific fields such as medicine and epidemiology (1, 6). Viewing SER as a microcosm of a society with a relatively homogeneous power structure, where disparities in either health or social outcomes are produced through structural and behavioral inequities that lead to differential access to and utilization of resources, the organization should center the developing initiative accordingly.
CURRENT CHALLENGES TO IMPROVE DIVERSITY AND INCLUSION IN EPIDEMIOLOGY
Despite evidence that diversity drives scientific innovation and the diversity efforts of funding agencies, entry and retention in science remain stagnant among disadvantaged populations (1, 7–12). Many reasons for attrition along the pipeline have been identified, including the need for evidence-based recruitment and training along with understanding the impact psychosocial factors have on individuals and institutional climates (13). Being less likely to obtain National Institutes of Health (NIH) funding along with personal values and structural dynamics (e.g., work-life balance) have also been implicated (5, 14, 15). Membership and involvement in professional societies like the SER likely play an important role in professional development and career success through visibility, networking, and opportunities to meet certain productivity metrics.
While the problems are plentiful and complex, the solutions can be simple. The main driver is historical maldistribution of power and resources, resulting in either a lack of diversity and inclusion or a leaky pipeline of career trajectories. Therefore, the potential solutions should center tightly around SER actively working to equitably distribute power and resources by naming and addressing the many barriers to the initiative’s progress. The objective of this commentary is to underscore the importance of diversity in science and offer a nonexhaustive list of SER initiative ideas (see Figure 1).
Figure 1.
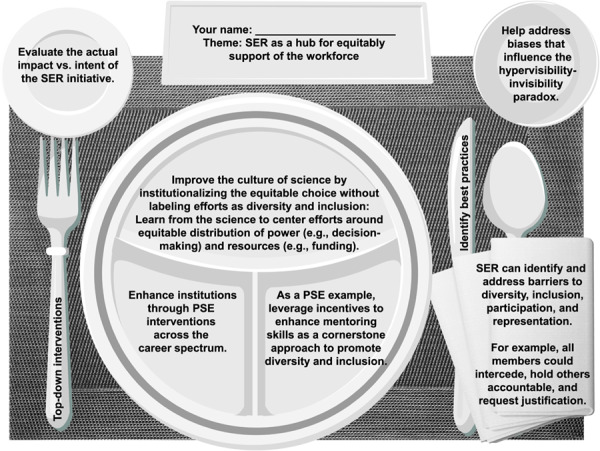
Initiative ideas to improve diversity, inclusion, representation, and participation in epidemiology. Policy, systems, and environmental (PSE) support = direct provision of (or active advocacy for) another organization or institution to provide tangible resources. SER, Society for Epidemiologic Research.
POTENTIAL OPPORTUNITIES TO IMPROVE DIVERSITY AND INCLUSION IN EPIDEMIOLOGY
SER leadership and interested members could identify potential opportunities by learning from scholars who identified, for instance, discriminatory policies and practices (e.g., segregation) as fundamental, unnatural causes of inequities, which can result in phenomena illustrated by the Gardener’s tale, marginalization, the Superwoman Schema, or John Henryism (where strain occurs when ambitions are not met with proper resources) (16–20). Researchers have also revealed that inequities can negatively affect everyone (21), and SER is no exception.
SER exists to support the workforce of epidemiologists and can enhance diversity and inclusion through efforts to improve the culture within stakeholder institutions and epidemiology in general. With the goal of becoming a model organization that could serve as a national example regarding diversity and inclusion, the committee should identify best practices to implement or advocate for (with an emphasis on top-down intervention approaches) coupled with routine process and outcome evaluations until the desirable, agreed-upon outcomes are attained. For example, NIH has recommended a systems approach to strengthening the pipeline (13). The Diversity Consortium Program has identified that “our ability to achieve lasting diversity across the career spectrum will benefit from data-driven systems approaches that link NIH’s ($250 million) investment (over 5 years) in training with measurable outcomes. A systems approach requires that we understand how outcomes at each career stage are influenced by institutional settings and interventions and by individual circumstances and decisions.” (13 p. 3, 22–37).
SER leadership and interested members can engineer equity by incorporating optimal policy, systems, and environmental interventions throughout trainees’ career trajectories without labeling approaches as diversity and inclusion efforts. Analogous to the culture of health initiatives (38), we can promote diversity and inclusion by making the equitable choice the default, easy choice through policy, systems, and environmental changes/interventions—as touted by the Centers for Disease Control and Prevention—to address structural and behavioral inequities that likely hinder diversity/inclusion (39).
SER could supplement institutional infrastructure by serving as an information and opportunity hub designed to better coordinate and streamline efforts to reduce predictable barriers across the career spectrum. SER leadership can provide concrete opportunities and connect to resources (e.g., financial), which might attract diverse trainees. For example, capacity-building (e.g., manuscript and/or grant writing; career coaching) and professional-development (e.g., mentoring, conflict resolution, negotiation) workshops (in-person or virtual) could be used to supplement underresourced or unsupportive/isolating home institutions. Also, SER leadership can recommend that R01 awardees seek to add administrative diversity supplements to their grants.
As a form of active engagement and consensus-building, given that all members need to feel included (not excluded), valued, and respected, focus groups or interviews of members can be conducted to identify barriers to participation and representation along with potential levers of change. Unmet needs could be identified to align the goals of SER with diverse members. After all, the most affected communities can best identify the solutions, which is not to imply that these populations are responsible for addressing historical issues. SER leaders and interested members can cultivate a culture where allies feel comfortable interceding (“who is not being represented at this table?”), calling out biases, challenging assumptions, and requesting justification for decisions, which have been shown to lead to better decisions (40). Focus groups (or even social media) could also be used to reengage non-SER members and better understand their lack of participation while anticipating reasons related to, for example, having no or insufficient funds to cover membership fees or dues and conference travel or untimely reimbursement of fees, time constraints, fear of exclusion or diminishing returns, and a lack of mentorship to tout its importance.
While everyone has implicit/unconscious biases, SER leaders and interested members can proactively address them (and their resulting consequential macro- or microaggressions) by implementing and advocating for the widespread implementation of tactics outlined at, for instance, https://biasinterrupters.org/. These tools can change behavior (e.g., more women and underrepresented groups hired) (41). The influence of biases when making key decisions could be minimized by using an algorithm for decisions or selection rather than human judgment. Explicit and implicit biases make negatives hypervisible or recognized in a manner that leads to shame or blame, exacerbated imposter syndrome, or stereotype threat, while positive attributes or contributions are rendered virtually invisible or underrecognized (42). This hypervisibility-invisibility paradox (and other abuses of power) among disadvantaged populations could contribute to phenomena known as “death by a thousand cuts” and “Black tax” (43).
An overreliance on “dinner table” conversations with insufficient representation of disadvantaged groups could be minimized by institutions creating and consistently implementing decision-making criteria and explicit written documents and policies needed for career advancement (e.g., lab expectations, symposia proposals, hiring and promotion procedures and policies) at all stages along the career pipeline (44). In fact, all SER policies could be evaluated for their impact on equity while anticipating unintended consequences.
SER leadership can enhance mentoring/sponsorship as a cornerstone approach to promote diversity/inclusion. Mentorship and especially sponsorship are paramount for supporting even the most talented individual’s career trajectory and ultimate success to enhance diversity and inclusion (45–48). SER leaders and interested members should advocate for and utilize diversity-focused, culturally sensitive mentorship training (such as the National Research Mentoring Network—a part of the Diversity Program Consortium), understanding that a good scientist does not automatically equate to a good mentor (49). Furthermore, it is likely that underrepresented groups experience unique stressors (e.g., discrimination), and effective mentors should not invalidate concerns. Also, well-intentioned accommodating (and ultimately sabotaging) of mentees for whom mentors have lower expectations should be countered with constructive, skill-building, and emotionally supportive critiques or suggestions for improvement. It could be useful to develop an incentivized cross-institution mentor-mentee matching program with established investigators in well-resourced institutions matched to mentees from disadvantaged groups identified through a directory (e.g., membership list) with social identity information.
Mentoring or sponsorship relationships often develop from academic networks that expand through organizations like SER. Therefore, effective networking at SER meetings and beyond can help “level the playing field.” SER and the field of epidemiology should seek to incentivize mentee diversity (e.g., inclusion in hiring, tenure, and leadership criteria; retention monitoring; offering monetary diversity awards; incorporation into strategic plans). SER leaders and interested members could tout (as a model) diversity success stories (e.g., partnerships between large universities and historically Black colleges and universities) that can be replicated elsewhere (50).
Furthermore, race-matched mentoring could provide an understanding of and protection from pervasive organizational and interpersonal biases, but mentoring solely based on subject-matter expertise does not require race matching. To help address time constraints that disproportionately affect racial/ethnic minorities (51), SER leadership could provide help with or advocacy for avoiding “invisible service” and buying time through, for instance, grant-writing assistance, employing cost-saving flexible schedules, and improving matters related to career balancing (52, 53). In what I deem the “good fit problem,” mentors/sponsors are more likely to prefer mentees like themselves, which disadvantages underrepresented racial/ethnic minorities. This could be mitigated with unconscious-bias and empathy training (“How would I feel in this situation?”). Also, SER members could advocate for trainees to establish a mentorship team consisting of multiple mentors whose areas of expertise do not greatly overlap but which cover domains considered important for success (54–58).
SER can leverage leadership to employ top-down interventions. As illustrative examples, NIH hired a Chief Officer for Scientific Workforce Diversity, prioritized recruitment of diverse investigators, requires diversity statements from investigator applications, requires implicit-bias training, incorporates an evaluation of diverse trainees into tenure criteria, and has helped turn “how diversity improves science” into a rigorous scientific area. As an example of representation, the NIH Director announced that he would no longer serve on panels without representation from women and other disadvantaged groups (59), and the leadership at SER could follow suit with an intersectionality lens. As one example of how SER could take on a stronger national advocacy role, SER leadership and committee members could influence or inform the Association of Schools and Programs of Public Health’s stance on diversity and inclusion principles and tactics through, for instance, formal statements, which can be used to more efficiently disseminate information across schools of public health, where many epidemiology programs are located. Regarding participation, SER meeting organizers should consider the broad attractiveness or feasibility of supported social activities (e.g., karaoke) and meeting locations that are sensitive to diverse members’ sociocultural identities given that spaces can be differentially experienced. For example, I once participated in a training held at what was obviously a former plantation. Regarding representation, mere academic understanding is not an effective replacement of lived experiences. Much like community stakeholders/partners serving as coauthors on publications (60), SER leaders and interested members could advocate for journals such as the American Journal of Epidemiology to require representation from the social identity group being studied on manuscripts in a “nothing about us without us” approach (61), which would structurally increase opportunities for disadvantaged groups and lead to more comprehensive citing of the literature (62). New standards for researchers, journals, and reviewers regarding publishing epidemiologic research on racial health disparities should also be employed (63). Furthermore, the SER selection committee could actively “make space” by requiring a certain percentage of the accepted symposia to include diverse speakers. SER leadership could have the initiative evaluated by discussing tracking, monitoring, and reporting of membership statistics (especially among leadership) at business meetings or plenary sessions during annual meetings as standard practice.
In conclusion, as demonstrated by the coronavirus disease 2019 (COVID-19) pandemic, everyone is interconnected and, therefore, negatively affected by a lack of diversity. We all have a role to play in increasing diversity to improve our science. To maximize our potential, we must ensure that everyone can acquire the nourishment they need to optimally participate in and contribute to the health and well-being of SER as an organization and the epidemiology field. Despite already full plates, we need to ensure that we have the buffet of options that meet all needs. This commentary serves as food for thought.
ACKNOWLEDGMENTS
Author affiliations: Epidemiology Branch, National Institute of Environmental Health Sciences, National Institutes of Health, Department of Health and Human Services, Research Triangle Park, North Carolina (Chandra L. Jackson); and Intramural Program, National Institute on Minority Health and Health Disparities, National Institutes of Health, Department of Health and Human Services, Bethesda, Maryland (Chandra L. Jackson).
This work was funded by the Intramural Program at the National Institute of Environmental Health Sciences (grant Z1AES103325-01).
I thank Erin Knight, Nyree Riley, and Dr. Symielle Gaston for their technical assistance.
Conflict of interest: none declared.
REFERENCES
- 1. DeVilbiss EA, Weuve J, Fink DS, et al. Assessing representation and perceived inclusion among members of the Society for Epidemiologic Research. Am J Epidemiol. 2020;189(10):998–1010. [DOI] [PubMed] [Google Scholar]
- 2. Valantine HA, Beckerle MC, Reed KL, et al. Teaching corporate in college. Sci Transl Med. 2014;6(251):251fs33. [DOI] [PubMed] [Google Scholar]
- 3. Hong L, Page SE. Groups of diverse problem solvers can outperform groups of high-ability problem solvers. Proc Natl Acad Sci U S A. 2004;101(46):16385–16389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Valantine HA, Collins FS. National Institutes of Health addresses the science of diversity. Proc Natl Acad Sci U S A. 2015;112(40):12240–12242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Valantine H. NIH's essential 21st-century research challenge: enhancing scientific workforce diversity. J Invest Dermatol. 2016;136(12):2327–2329. [DOI] [PubMed] [Google Scholar]
- 6. Albert MA. #Me_Who anatomy of scholastic, leadership, and social isolation of underrepresented minority women in academic medicine. Circulation. 2018;138(5):451–454. [DOI] [PubMed] [Google Scholar]
- 7. National Academy of Sciences Expanding Underrepresented Minority Participation. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 8. National Research Council (US) Committee to Study the National Needs for Biomedical, Behavioral, and Clinical Research Personnel Research Training in the Biomedical, Behavioral, and Clinical Research Sciences. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 9. Sauermann H, Roach M. Science PhD career preferences: levels, changes, and advisor encouragement. PLoS One. 2012;7(5):e36307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gibbs KD Jr, McGready J, Bennett JC, et al. Biomedical science Ph.D. career interest patterns by race/ethnicity and gender. PLoS One. 2014;9(12):e114736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gibbs KD Jr, McGready J, Griffin K. Career development among American biomedical postdocs. CBE Life Sci Educ. 2015;14(4):ar44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Working Group on Diversity in the Biomedical Research Workforce Draft report of the advisory committee to the director working group on diversity in the biomedical research workforce. Bethesda, MD; National Institutes of Health; 2012;184. [Google Scholar]
- 13. Valantine HA, Lund PK, Gammie AE. From the NIH: a systems approach to increasing the diversity of the biomedical research workforce. CBE Life Sci Educ. 2016;15(3):fe4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ginther DK, Schaffer WT, Schnell J, et al. Race, ethnicity, and NIH research awards. Science. 2011;333(6045):1015–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hoppe TA, Litovitz A, Willis KA, et al. Topic choice contributes to the lower rate of NIH awards to African-American/Black scientists. Sci Adv. 2019;5(10):eaaw7238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jones CP. Levels of racism: a theoretic framework and a gardener's tale. Am J Public Health. 2000;90(8):1212–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Williams DR, Cooper LA. Reducing racial inequities in health: using what we already know to take action. Int J Environ Res Public Health. 2019;16(4):606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. James SA. John Henryism and the health of African-Americans. Cult Med Psychiatry. 1994;18(2):163–182. [DOI] [PubMed] [Google Scholar]
- 19. Woods-Giscombé CL. Superwoman schema: African American women's views on stress, strength, and health. Qual Health Res. 2010;20(5):668–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Krieger N. Discrimination and health inequities In: Berkman LF, Kawachi I, Maria Glymour M, eds. Social Epidemiology. New York, NY: Oxford University Press; 2014:96. [Google Scholar]
- 21. Marmot M. Closing the health gap. Scand J Public Health. 2017;45(7):723–731. [DOI] [PubMed] [Google Scholar]
- 22. Hurtado S, White-Lewis D, Norris K. Advancing inclusive science and systemic change: the convergence of national aims and institutional goals in implementing and assessing biomedical science training. BMC Proc. 2017;11(suppl 12):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McCreath HE, Norris KC, Calderόn NE, et al. Evaluating efforts to diversify the biomedical workforce: the role and function of the Coordination and Evaluation Center of the Diversity Program Consortium. BMC Proc. 2017;11(suppl 12):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Urizar GG, Henriques L, Chun C-A, et al. Advancing research opportunities and promoting pathways in graduate education: a systemic approach to BUILD training at California State University, Long Beach (CSULB). BMC Proc. 2017;11(suppl 12):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Saetermoe CL, Chavira G, Khachikian CS, et al. Critical race theory as a bridge in science training: the California State University, Northridge BUILD PODER program. BMC Proc. 2017;11(suppl 12):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Estrada M, Eroy-Reveles A, Ben-Zeev A, et al. Enabling full representation in science: the San Francisco BUILD project’s agents of change affirm science skills, belonging and community. BMC Proc. 2017;11(suppl 12):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kamangar F, Silver G, Hohmann C, et al. An entrepreneurial training model to enhance undergraduate training in biomedical research. BMC Proc. 2017;11(suppl 12):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Taylor BE, Reynolds AJ, Etz KE, et al. BUILDing BLaST: promoting rural students’ biomedical research careers using a culturally responsive, One Health approach. BMC Proc. 2017;11(suppl 12):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Andreoli JM, Feig A, Chang S, et al. A research-based inter-institutional collaboration to diversify the biomedical workforce: ReBUILDetroit. BMC Proc. 2017;11(suppl 12):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. LaCourse WR, Sutphin KL, Ott LE, et al. Think 500, not 50! A scalable approach to student success in STEM. BMC Proc. 2017;11(suppl 12):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Collins TW, Aley SB, Boland T, et al. BUILDing SCHOLARS: enhancing diversity among U.S. biomedical researchers in the Southwest. BMC Proc. 2017;11(suppl 12):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Richardson DM, Keller TE, Wolf DSS, et al. BUILD EXITO: a multi-level intervention to support diversity in health-focused research. BMC Proc. 2017;11(suppl 12):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Foroozesh M, Giguette M, Morgan K, et al. Building integrated pathways to independence for diverse biomedical researchers: project pathways, the BUILD program at Xavier University of Louisiana. BMC Proc. 2017;11(suppl 12):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Davidson PL, Maccalla NMG, Afifi AA, et al. A participatory approach to evaluating a national training and institutional change initiative: the BUILD longitudinal evaluation. BMC Proc. 2017;11(suppl 12):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sorkness CA, Pfund C, Ofili EO, et al. A new approach to mentoring for research careers: the national research mentoring network. BMC Proc. 2017;11(suppl 12):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jones HP, McGee R, Weber-Main AM, et al. Enhancing research careers: an example of a US national diversity-focused, grant-writing training and coaching experiment. BMC Proc. 2017;11(suppl 12):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Guerrero LR, Ho J, Christie C, et al. Using collaborative approaches with a multi-method, multi-site, multi-target intervention: evaluating the National Research Mentoring Network. BMC Proc. 2017;11(suppl 12):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Robert Wood Johnson Foundation Building a culture of health. https://www.rwjf.org/en/how-we-work/building-a-culture-of-health.html. Accessed March 11, 2020.
- 39. Honeycutt S, Leeman J, McCarthy WJ, et al. Evaluating policy, systems, and environmental change interventions: lessons learned from CDC's prevention research centers. Prev Chronic Dis. 2015;12:E174-E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Girod S, Fassiotto M, Grewal D, et al. Reducing implicit gender leadership bias in academic medicine with an educational intervention. Acad Med. 2016;91(8):1143–1150. [DOI] [PubMed] [Google Scholar]
- 41. Devine PG, Forscher PS, Cox WTL, et al. A gender bias habit-breaking intervention led to increased hiring of female faculty in STEMM departments. J Exp Soc Psychol. 2017;73:211–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mowatt R, French B, Malebranche D. Black/female/body hypervisibility and invisibility a Black feminist augmentation of feminist leisure research. J Lei Res. 2013;45:644–660. [Google Scholar]
- 43. Lee H, Hicken MT. Death by a thousand cuts: the health implications of Black respectability politics. Souls. 2016;18(2–4):421–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Rieke MBaA Help wanted: an examination of hiring algorithms, equity, and bias. https://www.upturn.org/reports/2018/hiring-algorithms/. Accessed July 7, 2020.
- 45. Pfund C, Byars-Winston A, Branchaw J, et al. Defining attributes and metrics of effective research mentoring relationships. AIDS Behav. 2016;20(suppl 2):238–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Beech BM, Calles-Escandon J, Hairston KG, et al. Mentoring programs for underrepresented minority faculty in academic medical centers: a systematic review of the literature. Acad Med. 2013;88(4):541–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Flores G, Mendoza FS, DeBaun MR, et al. Keys to academic success for under-represented minority young investigators: recommendations from the research in academic pediatrics initiative on diversity (RAPID) National Advisory Committee. Int J Equity Health. 2019;18(1):93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Stolzenberg EB, Eagan K, Zimmerman HB, et al. Undergraduate Teaching Faculty: The HERI Faculty Survey 2016–2017. Los Angeles, CA: Higher Education Research Institute; 2019. [Google Scholar]
- 49. National Institutes of Health National Research Mentoring Network. https://nrmnet.net/. Accessed March 11, 2020.
- 50. Pelletier SG. Best practices: five decades on, Brown-Tougaloo partnership still thrives. https://www.nafsa.org/ie-magazine/2017/7/1/best-practices-five-decades-brown-tougaloo-partnership-still-thrives. Accessed July 17, 2020.
- 51. Gee GC, Hing A, Mohammed S, et al. Racism and the life course: taking time seriously. Am J Public Health. 2019;109(S1):S43–S47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Fassiotto M, Simard C, Sandborg C, et al. An integrated career coaching and time-banking system promoting flexibility, wellness, and success: a pilot program at Stanford University School of Medicine. Acad Med. 2018;93(6):881–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lerchenmueller MJ, Sorenson O, Jena AB. Gender differences in how scientists present the importance of their research: observational study. BMJ. 2019;367:l6573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Tsen LC, Borus JF, Nadelson CC, et al. The development, implementation, and assessment of an innovative faculty mentoring leadership program. Acad Med. 2012;87(12):1757–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Speck RM, Ward DS, Fleisher LA. Academic anesthesiology career development: a mixed-methods evaluation of the role of Foundation for Anesthesiology Education and Research Funding. Anesth Analg. 2018;126(6):2116–2122. [DOI] [PubMed] [Google Scholar]
- 56. Crews DC, Wilson KL, Sohn J, et al. Helping scholars overcome socioeconomic barriers to medical and biomedical careers: creating a pipeline initiative. Teach Learn Med. 2020. doi: 10.1080/10401334.2020.1729161 Accessed July 7, 2020. [DOI] [PubMed] [Google Scholar]
- 57. Stenken JA, Zajicek AM. The importance of asking, mentoring and building networks for academic career success—a personal and social science perspective. Anal Bioanal Chem. 2010;396(2):541–546. [DOI] [PubMed] [Google Scholar]
- 58. Cross R, Thomas R. A smarter way to network. Harv Bus Rev. 2011;89(7–8):149–167. [PubMed] [Google Scholar]
- 59. Collins FS. Time to end the manel tradition. https://www.nih.gov/about-nih/who-we-are/nih-director/statements/time-end-manel-tradition. Accessed July 7, 2020.
- 60. Eder MM, Holzer J, Calhoun K, et al. A retrospective on the vision for progress in community health partnerships: research, education, and action. Prog Community Health Partnersh. 2017;11(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Stewart M. Nothing about us without us, or the dangers of a closed-society research paradigm. Romani Studies. 2017;27(2):125–146. [Google Scholar]
- 62. Inge S. "Cite Black Women" campaign gains momentum. https://www.timeshighereducation.com/news/cite-black-women-campaign-gains-momentum. Accessed July 7, 2020.
- 63. Boyd RW, Lindo EG, Weeks LD, et al. On racism: a new standard for publishing on racial health inequities. https://www.healthaffairs.org/do/10.1377/hblog20200630.939347/full/. Accessed July 31, 2020. [Google Scholar]


