Abstract
Introduction
During the SARS-COV-2 pandemic and consequent government measures to prevent the overwhelming of public hospitals, emergency department (ED) orthopaedic turnout was significantly altered. This study compared the turnout of patients with upper extremity (UE) and hand & wrist (H&W) emergencies during the SARS-COV-2 pandemic, with the same period of 2019, in the public and private sector.
Material-Methods
Data from a two-month period [March 23, 2020 (application of severe restrictions of civilian circulation) to May 18, 2020 (two weeks after lockdown cessation)] were collected from a public-university hospital and a private hospital and were compared with data from the same “normal” period in 2019.
Results
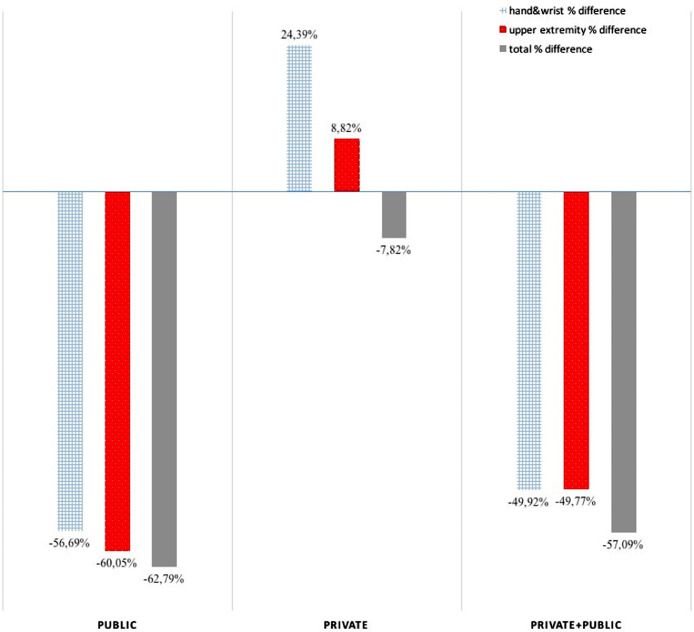
During the pandemic, the number of patients with orthopaedic, UE, and H&W problems was significantly reduced by 57.09%, 49.77%, 49.92% respectively (p<0.001) compared to 2019. However, the ratios of UE/total orthopaedic emergencies and of H&W/total orthopaedic emergencies increased significantly during the pandemic from 37.17% to 43.32% and from 25.07% to 29.15% (p=0.006 and p<0.001) respectively, compared to 2019. In the private sector, the turnout was increased for patients with UE problems (8.82%, p=0.67) and H&W problems (24.39%, p=0.3), while in the public sector the turnout was significantly decreased for UE (49.77%, p<0.001) and H&W problems (49.92%, p<0.001) in 2020 compared to 2019.
Discussion
The extent of lockdown was unprecedented in recent years. The reduction of orthopaedic, UE and H&W emergencies during lockdown can be attributed to the fear of contracting the virus in the hospitals and even more in hospitals serving as COVID-19 reference centers. Despite the decrease -in absolute numbers- of patients, the increased percentages of UE to total orthopaedic and of H&W to total orthopaedic emergencies in 2020 in both hospitals, reflect the new hobbies’ uptake and the increase of domestic accidents during the lockdown, despite overall activity decrease, and underline the necessity of presence of hand surgeons in the EDs. This is one of the very few population-based studies worldwide to show trends in incidence of different injuries of the UE at a regional level during the pandemic, and its results could affect future health care policies.
Keywords: SARS-COV-2 pandemic, Upper extremity, Hand, Wrist, Emergency department, Turnout
Introduction
On a worldwide scale, on January 30, the World Health Organization (WHO) declared COVID-19 outbreak a public health emergency of international concern [1]. In the absence of a COVID-19 vaccine, governments around the world had to take a number of public health measures to reduce the transmission of the virus and to avoid a massive influx of patients into public hospitals that could overwhelm health systems. In Greece, the first government action was on February 27th following the first three confirmed COVID-19 cases, which was to ban seasonal celebratory parades about to take place on the last weekend of February. By March 10th, there were 89 confirmed cases in the country, related mostly to travellers from the Mediterranean coastline (Italy and Israel) [2]. Strong recommendations were issued by the Ministry of Heath regarding individual sanitation measures, and prevention measures were taken in areas with increased confirmed cases. WHO reclassified the rapidly spreading coronavirus outbreak as a pandemic on March 11th [3]. From March 13th, Greek government actions escalated and on March 23rd, severe restrictions of civilian circulation were applied, not only between regions, but also inside cities, indefinitely. Only supermarkets, take away cafeterias, pharmacies, private medical facilities, car repair shops, petrol stations and heavy industry remained open. All Easter celebrations and family gatherings were prohibited. The lockdown period came to an end on May 4th 2020 and by that day, there were 2632 confirmed cases and 146 deaths of COVID-19 patients in Greece [4].
During these unprecedented circumstances and amid consequent government measures to prevent the overwhelming of public hospitals, emergency department orthopaedic turnout was significantly altered. According to various studies in Europe and the USA, under normal circumstances upper extremity injury incidence ranges from 1130 to 2491 per 100,000 persons per year of all injury patients visiting the Emergency Department (ED) [5], [6], [7]. We hypothesised that the epidemiology of patients visiting the ED during the lockdown period would be very different compared to the identical “normal” period in 2019, both qualitatively (diagnoses) and quantitatively.
The aim of this study was to report and analyze the regional epidemiologic characteristics of orthopaedic upper extremity emergency consultations and their variation during the COVID-19 pandemic, in a private and a public-university hospital of the same region, and to compare the turnout between the same periods of 2019 and 2020 and between the public and private sector. Ethical approval for this study was obtained from the Institutional Ethics/Scientific Committees of the two hospitals (Private Hospital: June 6, 2020 and Public University Hospital: June 22, 2020, ID:26045).
Materials and Methods
Data were obtained from two hand trauma centers accredited by the Hand Trauma Committee (HTC) of the Federation of European Societies for Surgery of the Hand (FESSH), one in a public university hospital and one in a private hospital. Both hospitals are located in the same regional unit, which is the 8th (out of 75) largest population-wise and the 2nd largest area-wise of the country [8]. The public university hospital was also a designated COVID-19 reference center.
Clinical notes, demographical data, outcome and radiology reports were collected for all consecutive patients with upper extremity problems (injuries or incidents like tumors, tendinopathies, arthritis flares) during the lockdown imposed in Greece from March 23rd 2020, up to May 18th 2020 (two weeks after termination of lockdown). The same data were collected from patient records for the identical period in 2019, as a control reference to compare.
Data were sorted by age, gender, diagnosis and outcome. Diagnoses were further divided into one of the following six main categories: a) soft tissue injury, b) infection, c) pain without direct injury (such as arthritis flare up, tendinopathy, painful mass or swelling), d) sprain, e) fracture and f) dislocation. Lacerations were further characterized as simple or more complex (comprising of injured tendons, nerves and amputations). Data were also sorted by specific anatomic region, which were: a) the shoulder (including clavicle and scapula), b) the humerus, c) the elbow, d) the forearm, e) the wrist and f) the hand. According to the HTC of FESSH, as it appears in its inclusion criteria for the European Emergency Hand Trauma Network, the definition of hand trauma is “any closed or open injury to the wrist and/or the hand, substantially involving skin, muscle, tendon, bone and joint, nerve and/or vessels” [9].
Descriptive statistics, Chi square and Student's t-test for paired or independent samples were appropriately used for data analyses. Statistical significance was set as p<0.05.
Results
Annual comparison
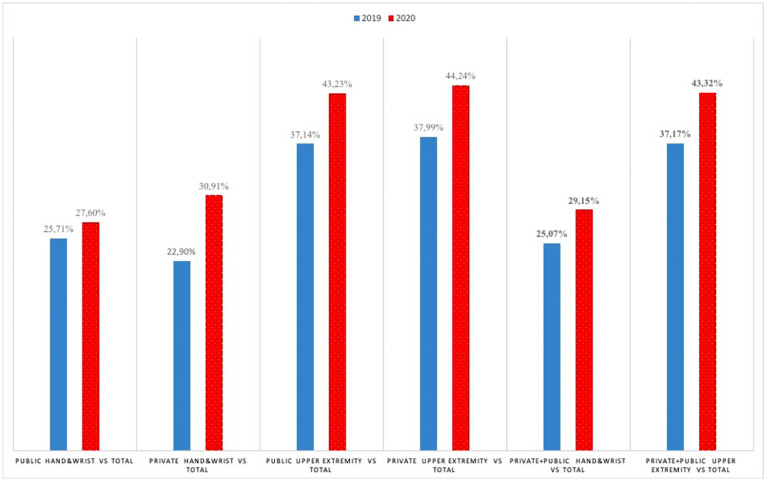
The total number of patients with orthopaedic problems in general, with upper extremity problems, and with hand & wrist problems specifically, was significantly lower in 2020, compared to 2019 (p<0.001 for orthopaedic problems, upper extremity problems and hand & wrist problems). The ratio of upper extremity to total orthopaedic emergencies increased significantly in 2020, from 37.17% to 43.32% (p=0.006). Similarly, the ratio of hand & wrist emergencies to total orthopaedic emergencies increased significantly in 2020, from 25.07% to 29.15% (p<0.001) (Fig. 1, Fig. 2, Fig. 3 ).
Fig. 1.
Differences in emergency department turnout between 2019-2020 per hospital and anatomical site.
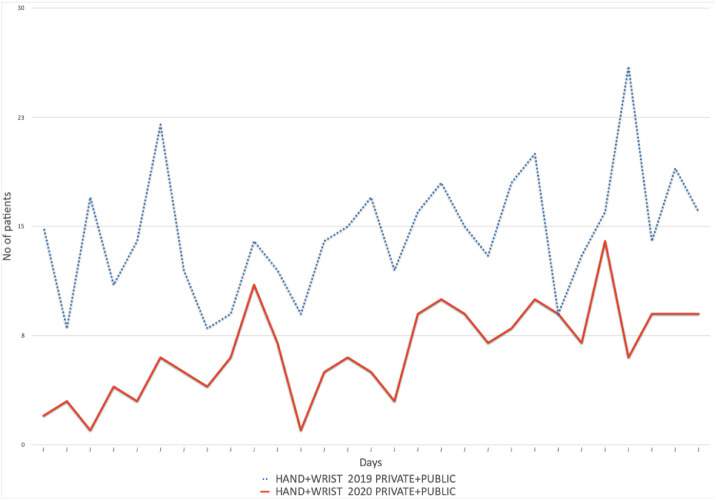
Fig. 2.
Daily turnout of patients with hand & wrist problems.
Fig. 3.
Annual ratio of upper extremity and hand & wrist emergencies to total orthopaedic emergencies.
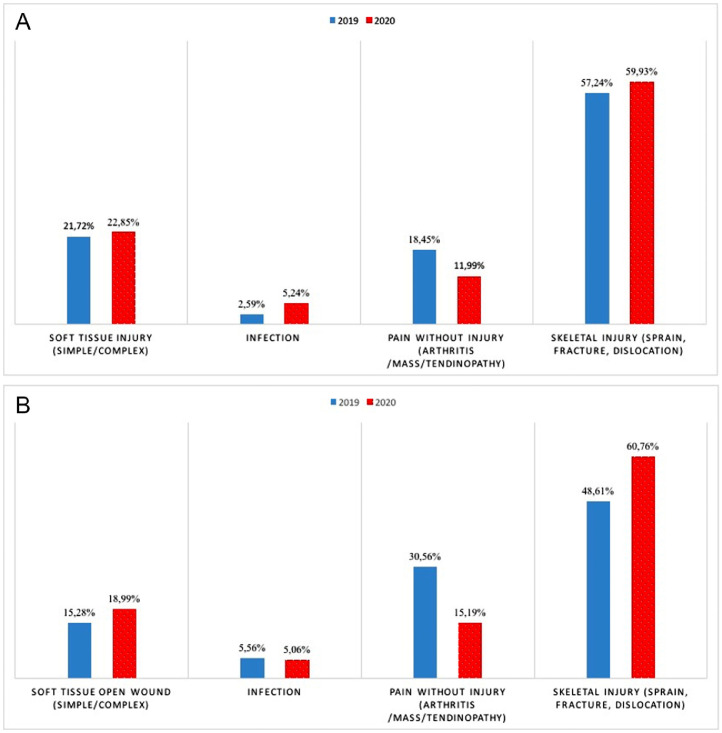
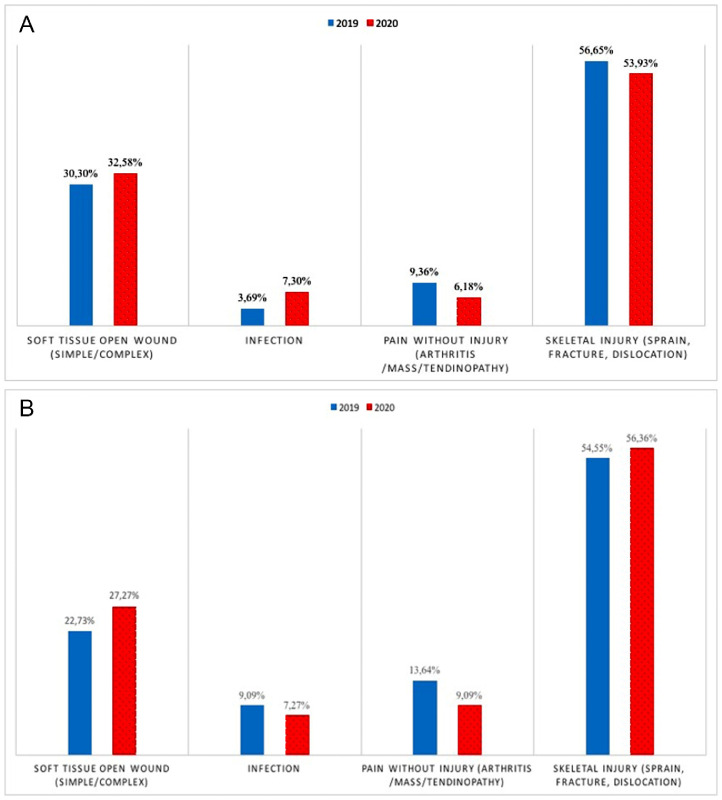
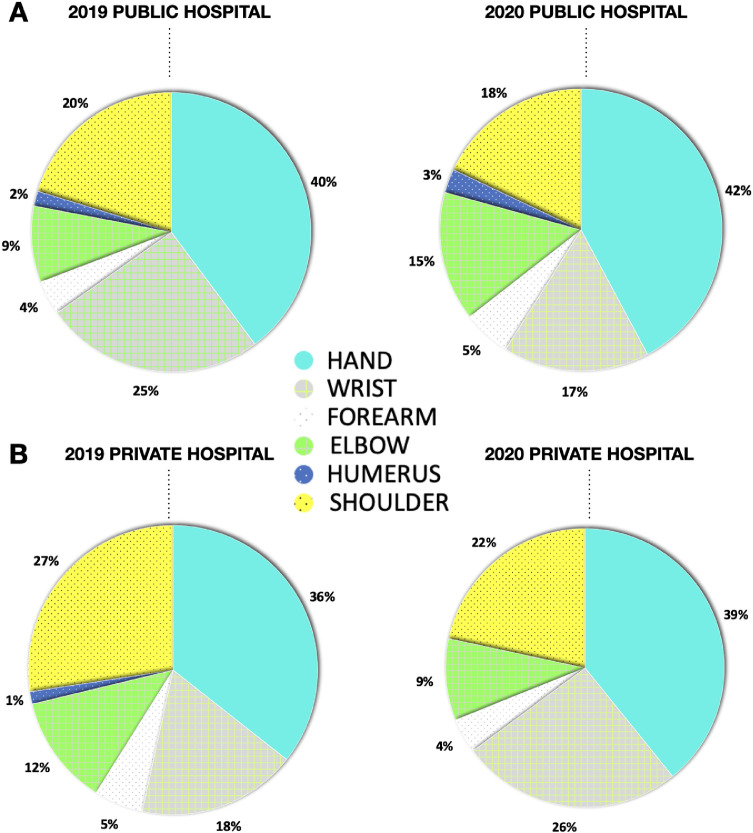
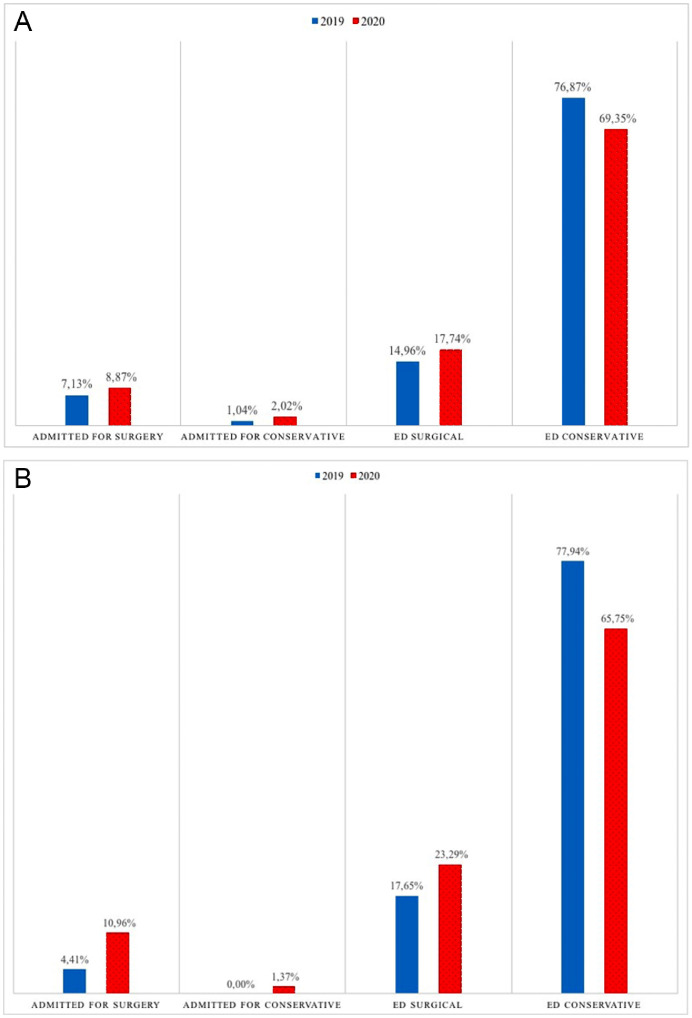
The frequencies of diagnoses per year are shown in Figs. 4 and 5 . The distribution of diagnoses per anatomical region per year are shown in Fig. 6 . Finally, the type of treatment (surgical or conservative) is presented in Fig. 7 .
Fig. 4.
Annual frequency of different upper extremity diagnoses: (A) public hospital, (B) private hospital.
Fig. 5.
Annual frequency of different hand & wrist diagnoses: (A) public hospital, (B) private hospital.
Fig. 6.
Annual distribution of diagnoses per anatomical region: (A) public hospital, (B) private hospital.
Fig. 7.
Type of treatment for upper extremity patients per year: (A) public hospital, (B) private hospital.
Comparison according to sector
Private Hospital
In 2019, patients with upper extremity problems comprised 37.99% of all orthopaedic emergencies, while patients with hand and wrist problems comprised 22.9%. In 2020, patients with upper extremity problems comprised 44.24% of all orthopaedic emergencies, while patients with hand and wrist problems comprised 30.91% (Fig. 3).
Between 2019 and 2020 the total number of patients with hand and wrist problems did not differ significantly (p=0.3), nor did the daily ratio of above elbow to below elbow patients (p=0.23) nor the daily ratio of patients with hand and wrist problems to total orthopaedic emergencies (p=0.55).
Although total orthopaedic turnout in the ED decreased by 7.82% between 2019 and 2020 (p=0.45), patients with upper extremity problems in total and with hand & wrist problems specifically, increased by 8.82% (p=0.67) and 24.39% (p=0.3), respectively (Fig. 1).
The mean age of patients with upper extremity problems was 43.16 years in 2019, and 47.16 in 2020 (p=0.36). A prevalence of female patients was noted although the male/female ratio did not differ between the 2 periods (p=0.81 for 2019 and p=0.48 for 2020) (Table 1 ).
Table 1.
Sample Demographics.
| Year | 2019 |
2020 |
||||
|---|---|---|---|---|---|---|
| Hospital | Public | Private | Public & Private | Public | Private | Public & Private |
| Mean age | 39.96 | 43.16 | 40.3 | 40.8 | 47.16 | 42.1 |
| (range) | (2-89) | (3-87) | (2-89) | (1.5-92) | (2-97) | (1.5-97) |
| [St. deviation] | [22.96] | [24.26] | [23.14] | [23.21] | [26.28] | [24.13] |
| 95% Conf. interval | 1.88 | 5.96 | 1.79 | 2.93 | 6.17 | 2.67 |
| Male/female (%) | 62.6/37.4 | 48.5/51.5 | 61.1/38.9 | 61.4/38.6 | 46.6/53.4 | 58.1/41.9 |
Public University Hospital
In 2019, patients with upper extremity problems comprised 37.14% of all orthopaedic emergencies, while patients with hand and wrist problems comprised 25.71%. In 2020, patients with upper extremity problems comprised 43.23% of all orthopaedic emergencies, while patients with hand and wrist problems comprised 27.6% (Fig. 3).
The daily ratio of patients with above elbow to below elbow problems also did not differ significantly between 2019 and 2020 (p=0.4), nor did the daily ratio of patients with hand and wrist problems to total orthopaedic emergencies (p=0.28).
Total orthopaedic attendance in the emergency department decreased by 62.79% between 2019 and 2020 (p<0.001). Patients visiting the ED for hand and wrist problems were decreased by 49.92% (p<0.001) and patients visiting for upper extremity problems were decreased by 49.77% (p<0.001) (Fig. 1).
Mean age of patients with upper extremity problems was 39.96 years in 2019, and 40.58 in 2020 (p=0.72), while more male patients visited the ED for upper extremity problems both in 2019 (p<0.001) and 2020 (p<0.001) (Table 1).
Private versus Public University Hospital
The daily ratio of patients with hand and wrist problems to total orthopaedic emergencies did not differ significantly between the two hospitals for both years (p=0.63 for 2019 and p=0.1 for 2020) nor did the ratio of patients with upper extremity to total orthopaedic emergencies differ for any of the years (p=0.62 for 2019 and p=0.31 for 2020).
The daily ratio of patients with above elbow to below elbow problems was statistically higher in the public hospital for both years (p<0.005).
There was a trend for older patients visiting the private hospital compared to the public hospital, although it did not reach statistical significance for both years (p=0.31 and p=0.06) (Table 1).
More male patients with upper extremity problems visited the ED in 2019 and 2020 (p<0.001 and p=0.003, respectively).
Discussion
The extent of lockdown was unprecedented in recent years, and no previous epidemiological data concerning trauma consultations to ED are available. Even in the most recent SARS outbreak in Asia, health policy actions were different. SARS outbreak was contained by means of syndromic surveillance, prompt isolation of patients, strict enforcement of quarantine of all contacts, and only in a few areas was community-level quarantine forced [10]. One would expect to observe major differences in ED visits, firstly due to decreased traffic and leisure activities, secondly due to fear of contacting or transmitting the virus and finally due to change in ED organisation during the pandemic. In a recent research on stroke admissions and referrals, there was an initial significant decrease in strokes (by 20%) mainly driven by patient-related factors, such as fear of exposure to the SARS-CoV-2, while the reduction of stroke referrals after the termination of lockdown was largely explained by hospital policies [11]. In Italy, a significant reduction in all admissions due to severe emergent cardiovascular diseases was observed, and the authors hypothesised that a significant decrease in the incidence of cardiac diseases seemed unlikely, and that several factors related to misinformation (widespread appearance of COVID-19 news on mass media, spread of fake news on social media, and lack of verified information on precautions limiting in-hospital spread of the disease) have contributed to the public perception of hospitals as unsafe environments [12].
This research showed that during the initial lockdown of the pandemic there was a vast reduction of orthopaedic patients in the public hospital , and a minor reduction in the private hospital. The best explanation for this paradox could be that patients tried to avoid visiting hospitals for fear of contracting the virus and even more the public hospital that was a COVID-19 reference center.
In our study, a significant decrease in absolute numbers of upper extremity patients was noted in 2020 in the public sector but not in the private, while the percentage of upper extremity to orthopaedic emergencies increased significantly in both hospitals. Finally, the percentage of admissions for upper extremity surgery to all orthopaedic emergencies increased slightly in the public sector and significantly in the private. In a study that took place during the pandemic, a significant reduction of 32% in absolute numbers of all extremity injury-related admissions was also recorded, while the ratio of admissions of patients with upper extremity fractures to all orthopaedic admissions remained constant between 2018 and 2020 [13]. In another study on upper extremity patients’ turnout during the pandemic, despite a 65% decrease in rate of emergencies, patients were treated surgically more often in 2020 compared to the previous year [14].
Although in absolute numbers there was a decrease of orthopaedic, upper extremity and hand & wrist emergencies, the percentage of hand & wrist patients to total orthopaedic patients increased significantly from 2019 to 2020, in both hospitals, comprising approximately 30% of orthopaedic patients for 2020. This is probably due to the new hobbies’ uptake and thus, increase of domestic accidents during the lockdown, despite overall activity and MVAs decrease. The percentage of patients with hand & wrist emergencies should raise concern in the orthopaedic community about the competence of ED physicians (general practitioners, general surgeons, young orthopedic residents) on diagnosing and treating such patients. Also, in a study from Netherlands published in 2013, Polinder et al found over a 22-year period that upper extremity injury comprised 42% of the total injury-related ED visits [7]. Thus, an experienced hand surgeon in any trauma center should become a necessity rather than a luxury.
Hand and wrist problems were more common compared to above elbow problems in the present study for both 2019 and 2020, with skeletal injuries also prevailing in both years. Pichard et al report that the proximal or distal location of upper extremity problem did not differ between 2019 and 2020 [14]. Similar trends for the type of hand and wrist injuries have been demonstrated in several studies [6,7,15,16], with the exception of a study focusing on the effect of the recent pandemic on hand and wrist injuries, with skeletal injuries being the second reason for ED visits, following lacerations [14]. Due to surgical treatment and prolonged rehabilitation, over 75% of health care costs are attributed to fractures [7]. Infection rates remained low and very similar between 2019 and 2020 in our study, although they have been reported to be as high as 17% [16].
In general, upper extremity problems appear to be age-related [7] and gender-related with male patients being slightly more prone to upper extremity injuries [5]. In the present study a male predominance was observed but the age-related trend was not depicted. Concerning the increase of the age of patients that was noted previously during lockdown between 2019 and 2020 [14], in the present study the age of patients did not differ significantly between the 2 years.
This study is not without limitations. It was decided not to include data concerning mechanism of injury (such as fall, home or workplace accidents, motor vehicle accidents), since data were not available for all patients. Data from other public or private health care facilities or primary care centers in the region were also not available for inclusion in the study. In addition, the fact that one of two hospitals was a COVID-19 reference center might create bias, as patients would avoid even more to visit the ED of a COVID-19 reference hospital. Finally, the lack of a national health registry makes it impossible to obtain national data for epidemiological purposes in our country.
Conclusions
To the best of our knowledge, this is one of the very few population-based studies worldwide to show trends in incidence of different injuries of the upper extremity at a regional level during the SARS-COV-2 virus pandemic. The results presented in this study are epidemiologically extremely valuable, they raise concern about the role of the hand surgeon in the emergency department and should affect future health care policy.
Declaration of Competing Interest
None.
References
- 1.WHO Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) – 30 January 2020. https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- 2.Greek Ministry of Health. https://www.moh.gov.gr/articles/ministry/grafeio-typoy/press-releases/6809-anakoinwsh-5-newn-kroysmatwn-sars-cov-2
- 3.WHO Director-General's opening remarks at the media briefing on COVID-19 – 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19%2D%2D-11-march-2020
- 4.Greek Ministry of Health. https://www.moh.gov.gr/articles/ministry/grafeio-typoy/press-releases/7141-enhmerwsh-diapisteymenwn-syntaktwn-ygeias-apo-ton-yfypoyrgo-politikhs-prostasias-kai-diaxeirishs-krisewn-niko-xardalia-ton-ekproswpo-toy-ypoyrgeioy-ygeias-gia-to-neo-koronoio-kathhghth-swthrh-tsiodra-kai-ton-ypoyrgo-dikaiosynhs-kwsta-tsiara-4-5
- 5.Giustini M, de Leo A, Leti Acciaro A, Pajardi G, Mamo C, Voller F, et al. Incidence estimates of hand and upper extremity injuries in Italy. Ann Ist Super Sanita. 2015;51(4):305–312. doi: 10.4415/ANN_15_04_10. [DOI] [PubMed] [Google Scholar]
- 6.Ootes D, Lambers KT, Ring DC. The epidemiology of upper extremity injuries presenting to the emergency department in the United States. Hand (N Y) 2012;7(1):18–22. doi: 10.1007/s11552-011-9383-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Polinder S, Iordens GI, Panneman MJ, Eygendaal D, Patka P, Den Hartog D, et al. Trends in incidence and costs of injuries to the shoulder, arm and wrist in The Netherlands between 1986 and 2008. BMC Public Health. 2013;13:531. doi: 10.1186/1471-2458-13-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hellenic Statistical authority. https://www.statistics.gr/en/statistics/pop
- 9.Federation of European Societies for Surgery of the Hand. http://fessh.com/hand-trauma-committee/
- 10.Wilder-Smith A, Chiew CJ, Lee VJ. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect Dis. 2020;20(5):e102–e107. doi: 10.1016/S1473-3099(20)30129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bres Bullrich M, Fridman S, Mandzia JL, Mai LM, Khaw A, Vargas Gonzalez JC, et al. COVID-19: Stroke Admissions, Emergency Department Visits, and Prevention Clinic Referrals [published online ahead of print, 2020 May 26]. Can J Neurol Sci 2020:1-4. doi:10.1017/cjn.2020.101. [DOI] [PMC free article] [PubMed]
- 12.Toniolo M, Negri F, Antonutti M, Masè M, Facchin D. Unpredictable Fall of Severe Emergent Cardiovascular Diseases Hospital Admissions During the COVID-19 Pandemic: Experience of a Single Large Center in Northern Italy [published online ahead of print, 2020 May 22]. J Am Heart Assoc 2020:e017122. doi:10.1161/JAHA.120.017122 [DOI] [PMC free article] [PubMed]
- 13.Hernigou J, Morel X, Callewier A, Bath O, Hernigou P. Staying home during "COVID-19" decreased fractures, but trauma did not quarantine in one hundred and twelve adults and twenty eight children and the "tsunami of recommendations" could not lockdown twelve elective operations [published online ahead of print, 2020 May 25] Int Orthop. 2020:1–8. doi: 10.1007/s00264-020-04619-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pichard R, Kopel L, Lejeune Q, Masmoudi R, Masmejean EH. Impact of the COronaVIrus Disease 2019 lockdown on hand and upper limb emergencies: experience of a referred university trauma hand centre in Paris, France [published online ahead of print, 2020 Jun 2] Int Orthop. 2020:1–5. doi: 10.1007/s00264-020-04654-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, 3rd Cornwell EE. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143(10):945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 16.Wenzinger E, Rivera-Barrios A, Gonzalez G, Herrera F. Trends in Upper Extremity Injuries Presenting to US Emergency Departments. Hand (N Y) 2019;14(3):408‐12. doi: 10.1177/1558944717735943. [DOI] [PMC free article] [PubMed] [Google Scholar]