Abstract
Introduction
Medication administration errors (MAEs) are common health problems that threaten patient safety and raise mortality rates, duration of hospital stay, and cost of services. It also influences healthcare professionals performing the procedure and healthcare organizations. Its prevalence in Ethiopia is high ranging from 51.8% to 90.8%.
Objective
This study aimed to assess the magnitude and associated factors of MAE among nurses at Northwest Amhara Region Referral Hospitals.
Methods
An institution-based cross-sectional study was conducted from February to March 2019. A simple random sampling technique was employed to select 348 nurses. Structured pretested self-administered questionnaires and an observational checklist were used to collect data. The data were entered in Epi-info version 7, analyzed using SPSS version 20 (SPSS Inc., Chicago, IL), and presented in tables and graphs. Bivariate and multivariable logistic regressions were computed to identify the factors associated with MAEs. p Values <.05 and adjusted odds ratios were used to declare the significance and strength of the association.
Results
One hundred and seventy-eight (54%) of the respondents made MAEs in the last 12 months. Only 10 (5%) of the 200 observed nurses were administered medications without any breach in any of the six rights of medication administration. Factors like poor knowledge (AOR = 5.98; 95% CI (2.39,14.94)), poor communication (AOR = 2.94; 95% CI (1.34, 6.46)), stress (AOR = 5.41; 95% CI (2.53, 11.57)), interruption during medication administration (AOR = 4.70, 95% CI (2.42, 9.10)), and night shift (AOR = 2.79, 95% CI (1.42, 5.46)) were significantly associated with MAE.
Conclusions
The magnitude of MAE was high. Poor knowledge, poor communication, stress, night shift, and interruption were significantly associated with MAEs. Strengthening institutional medication administration regulations and guidelines and minimizing interruption during medication administration would help minimize MAEs.
Keywords: Magnitude, medication administration, medication administration error, nurse; Northwest Ethiopia
Introduction
Medication administration errors (MAEs) can be defined as a deviation from the prescriber’s medication order as written on the patient’s chart, manufacturers’ administration instructions, or relevant institutional policies1. It is a medication error (ME) when one of the six rights of medication administration (time, patient, medication, dose, route, and documentation) is breached. It reaches patients and poses a threat to patient safety, increasing mortality rates, length of hospital stay, and related costs2. Medication errors most commonly occur during the administration step of the medication process3. Wrong time error, administering the drug to the wrong patient, wrong dose error, administering the wrong drug, and administering medication through the wrong route are the most prevalent administration errors4. Medication errors can occur by any member of a healthcare team, but errors committed by nurses are the most common because nurses spend most of their time administering medication in hospitals5. Medication administration errors are common in Middle Eastern countries which ranges from 9.4 to 80% of all MEs. Medication-related harm poses many disabilities to patients living in low-income countries than those living in high-income countries6.
In African hospitals, 8.4% of patients reported having experienced any suspected adverse drug event at hospital admission and 2.8% of patients admitted to hospitals due to adverse drug events. Similarly, the mortality rate attributed to adverse drug events was 0.1%7. In Egypt, 0.77% of patients were harmed by MAEs and needed either extended hospitalization or intervention8. In Ethiopia, MAE is a common health problem with a magnitude ranging from 51.8% to 90.8%9–12, and 1.5% of patients experienced actual adverse drug events associated with MEs13. Healthcare professionals are suffering from MEs, especially nurses who commit MAEs can suffer emotional distress and lack confidence, especially when the error results in significant patient harm. Health institutions also suffer from MEs through the increased cost of unplanned prolonged hospitalization and treatment of patients14,15. Failure to check the patient’s identification before administration, the storage of similar preparations in similar areas, interruptions during medication administration, characteristics of the nurse (age, sex, work experience, year in the specific unit, nurse-to-patient ratio, and educational status), route, medication administration at night shift, and inaccurate documentation and inadequate communication during changes in shifts in hospitals are the most common factors associated with MAEs16–19.
The WHO’s third global patient safety challenge program develops a strategy to reduce severe, avoidable medication harms by half by 2022, especially by addressing harm results from errors due to weakness in the health system and by making improvements in the medication administration practices6. Although MAEs are well investigated throughout much of the developed world, the issue has only rarely been researched in developing countries, including Ethiopia. Therefore, this study was intended to assess the magnitude and associated factors of MAEs among nurses working in Northwest Amhara Region Referral Hospitals, Northwest Ethiopia.
Methods and materials
Study design and period
An institutional based cross-sectional study was conducted from 19 February 2019 to 20 March 2019.
Study setting
The study was conducted in the Northwest Amhara Region Referral Hospitals. According to the 2007 Central Statistical Agency of Ethiopia, Amhara National Regional State has a total population of 17,221,976 of whom 8,641,580 are male and 8,580,396 females. Debre Markos, Felege Hiwot, and the University of Gondar are the three referral hospitals found in Northwest Amhara Region. Each referral hospital serves 3.5–5 million people. There are more than 906 (463 nurses) and 430 (222 nurses) healthcare professionals at the University of Gondar Comprehensive Specialized Referral Hospital and Debre Markos Referral Hospital, respectively, who are assigned in different units to offer health care services.
Study participants
Nurses working in Northwest Amhara Region Referral Hospitals during the study period who have at least a diploma qualification in nursing, a minimum of one-year work experience, and providing direct patient care were included in the study. Those nurses who were on annual leave, maternal leave, and seriously ill and attending external training courses off-site during the study period were excluded.
Sample size determination and sampling procedure
The sample size was calculated using Epi info version 7 stat cal by taking the estimated proportion of MAE among nurses: 71%, confidence level of 95%, and margin of error 5% for magnitude, while for factors associated with MAEs (assuming comparative cross-sectional; unexposed: exposed (1:1)). The final sample size was 348, after adding a 10% non-response rate. From three total referral hospitals, two hospitals were selected using the lottery method. A sampling frame was prepared for each hospital by taking lists of nurses from the hospital human resource management after the number of nurses was proportionally allocated to each hospital. Finally, each study subject was selected using a simple random sampling technique.
Data collection instruments and procedures
Data were collected using a validated structured pretested self-administered questionnaire that was adapted from previous studies. Separate tools were used to collect data regarding knowledge of nurses concerning medication and medication administration, the attitude of nurses toward medication administration, and communication of nurses with other nurses and physicians during medication administration adapted from previous studies and guidelines developed by recognized nursing associations. Stress and fatigue were also measured using separate stress and fatigue assessment scales. The Workplace Stress Scale from the American Institute of Stress which contains eight statements about how nurses usually feel was used to assess stress and participants who score 26 and above on the stress measurement scale were considered as having stress20. A validated 10-item fatigue assessment scale was used to assess fatigue and participants who score 22 and above the fatigue assessment scale were considered as having fatigue21. The scale’s psychometric properties were analyzed and internal consistency of 0.90 was obtained. The observational checklist developed by reviewing different kinds of literature was used to gather data by observing nurses while medicating patients to assess whether they followed the six rights of medication administration or not before they were asked to fill the self-administered questionnaire. The questionnaire was collected with the help of six trained BSc nurse data collectors and two MSc nurse supervisors. A written guideline was given to data collectors to assure that every nurse received the same directions and information.
Data processing and analysis
All the collected data were checked for completeness, then compiled, coded, and finally entered into EPI-INFO version 7.2.1.0. Incomplete data were considered as a non-response. The entered data were exported to SPSS version 20 (SPSS Inc., Chicago, IL) statistical software for analysis. Frequencies and percentages were used to describe the descriptive statistics of the data, and tables and graphs were used for data presentation. To assess the association between independent variables and the dependent variable, first bivariate relationships between each independent variable and outcome variable were investigated using a binary logistic regression model. Independent variables with a p value <.2 at the bivariate level were included in multivariable analysis to control for potential confounding factors. After adjusting for their effect on the outcome variable, those variables with a p value <.05 with a 95% confidence interval were regarded as factors significantly associated. The strength of association was determined using adjusted odds ratios with 95% confidence intervals. Model fitness was checked using the Hosmer and Lemeshow test, and the model was well fitted because the p value was >.05 (.83).
Data quality assurance
The data collection instruments were reviewed by four experts (two clinical nurses and two nurse academics). The tools were also tested with a pretest by taking 10% of the sample size two weeks before the actual data collection time at Debre Tabor Hospital. Amendments on the instrument, such as unclear questions and ambiguous words, were made accordingly. The resultant data were used to calculate Cronbach’s alpha, which was 0.84 for the self-administered questionnaire and 0.72 for the observational checklist. The data collected in the pretests were not included in the final results. Data collectors and supervisors were recruited based on their experience in data collection and supervision, and one-day training was given regarding the objective of the study, instrument, and data collection procedures by the principal investigator. Supervision was conducted by the principal investigator and supervisors. Data were collected in a separate and quiet room. The observees were aware of the observation but unaware of when they were being observed.
Ethical consideration
Before conducting the study, ethical clearance was obtained from the Institutional Review Board of the University of Gondar on behalf of the ethical review committee of the School of Nursing. Written permission letters were obtained from the clinical directors of the hospitals. Participants were informed about the purpose of the study and verbal informed consent was obtained from them. Confidentiality was maintained by omitting direct personal identifiers on the questionnaire, by using code numbers, by storing data locked with a password, and not misuse or wrongfully disclose their information. Participants were also informed that participation was voluntary and they could withdraw from the study participation at any stage if they were not comfortable about the investigation. The nurses did not know who the data collectors and supervisors were because they were recruited from hospitals not included in the study. The investigator prepared a one-page information sheet regarding the purpose and nature of the study.
Results
Socio-demographic and work-related characteristics of the respondents
A total of 332 nurses participated in this study, with a 95.4% response rate. More than half (56.3%) of the respondents were male and nearly half (50.6%) of them were married. The median age of the respondents was 28.5 (27, 31) inter quartile range (IQR), and more than half (58.1%) of them fell in the age range of 25–29 years. Concerning the educational level, the majority of the respondents (81.9%) had a Bachelor of Science degree in nursing. The majority (83.7%) of the study participants were Orthodox, and 254 (76.5%) of them were Amhara in ethnicity. The median monthly salary of the respondents was 5294 Ethiopian birr (4446, 6179) IQR, and nearly half (53.3%) of them earned a monthly salary of 4000–5999 Ethiopian birrs (Table 1).
Table 1.
Socio-demographic characteristics of nurses working in Northwest Amhara Region Referral Hospitals, Northwest Ethiopia, 2019 based on the questionnaire (n = 332 nurses).
| Variables | Category | Frequency (n = 332) | Percentage (100%) |
|---|---|---|---|
| Age | 20–24 years | 11 | 3.3 |
| 25–29 years | 193 | 58.1 | |
| 30–34 years | 99 | 29.8 | |
| ≥35 years | 29 | 8.8 | |
| Sex | Female | 145 | 43.7 |
| Male | 187 | 56.3 | |
| Marital status | Single | 147 | 44.3 |
| Married | 168 | 50.6 | |
| Othersa | 17 | 5.1 | |
| Educational status | Diploma | 42 | 12.7 |
| BSc nurse | 272 | 81.9 | |
| MSc nurse | 18 | 5.4 | |
| Religion | Orthodox | 278 | 83.7 |
| Muslim | 35 | 10.6 | |
| Protestant | 19 | 5.7 | |
| Ethnicity | Amhara | 254 | 76.5 |
| Oromo | 42 | 12.7 | |
| Tigere | 13 | 3.9 | |
| Othersb | 23 | 6.9 | |
| Monthly salary (ETB) | 2000 − 3999 | 49 | 14.8 |
| 4000 − 5999 | 177 | 53.3 | |
| 6000 − 7999 | 96 | 28.9 | |
| 8000 − 9999 | 10 | 3.0 |
Abbreviation. ETB, Ethiopian Birr.
Separated, divorced.
Kimanit, SNNP, and Guragie.
The median work experience of respondents was 4 (3, 6) IQR years, and most of them (91.3%) were working in the inpatient department. Concerning the duty shift, more than half (59.0%) of the respondents were working in the day shift. Nearly, two-thirds (65.0%) of nurses had worked for more than five months in their unit. More than three-fourths (77.7%) nurses worked in rotation. The majority (88.3%) of the participants were forced to work more than expected to do at a specified time and nearly half (50.3%) of nurses faced interruption during medication administration (Table 2).
Table 2.
Work-related characteristics of nurses working based in Northwest Amhara Region Referral Hospitals, Northwest Ethiopia, 2019 on the questionnaire (n = 332 nurses).
| Variables | Category | Frequency (n = 332) | Percentage (100%) |
|---|---|---|---|
| Work experience | ≤5 years | 226 | 68.1 |
| 6–10 years | 90 | 27.1 | |
| 11–15 years | 12 | 3.6 | |
| >15 years | 4 | 1.2 | |
| Working unit | Medical ward | 58 | 17.5 |
| Surgical ward | 77 | 23.2 | |
| Pediatrics ward | 67 | 20.2 | |
| Emergency | 74 | 22.3 | |
| ICU | 26 | 7.8 | |
| OPD | 29 | 8.7 | |
| Duty shift | Day shift | 196 | 59.0 |
| Night shift | 136 | 41.0 | |
| Type of shift work | Rotating | 258 | 77.7 |
| Fixed | 74 | 22.3 | |
| Faced interruption | Yes | 167 | 50.3 |
| No | 165 | 49.7 | |
| Faced workload | Yes | 293 | 88.3 |
| No | 39 | 11.7 | |
| Duration in the present working unit | ≤3 months | 45 | 13.6 |
| 4–5 months | 71 | 21.4 | |
| ≥6 months | 216 | 65.0 |
Magnitude and types of medication administration errors
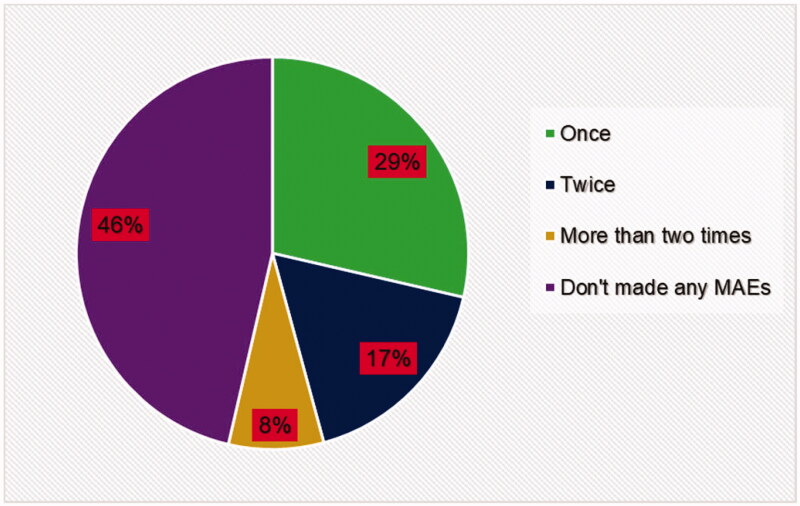
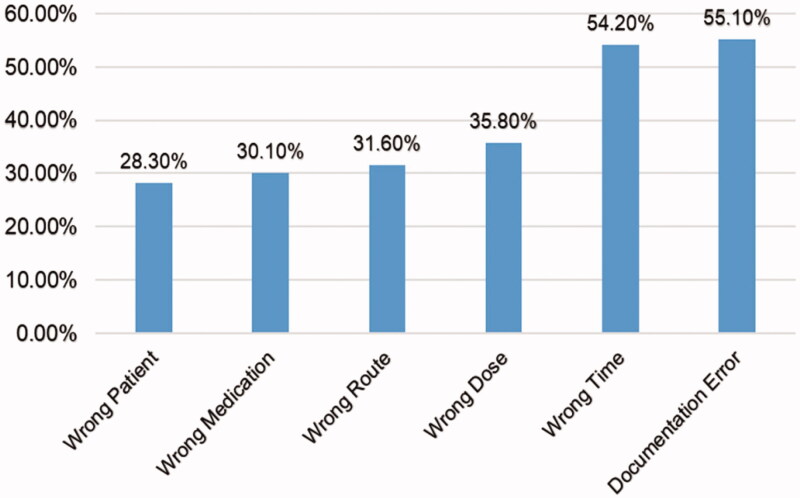
From a total of 332 study participants, 54% of nurses made MAE in the last 12 months with 95% CI (47.9, 59.3) based on the questionnaire. Among these, 29% of the participants made MAE only once during the specified period, while 17% and 8% of them made MAE two times and more than two times, respectively (Figure 1). Regarding the types of MAEs, documentation error was the most frequent one (55.1%), followed by the wrong time (54.2%), wrong dose (35.8%), wrong route (31.6%), wrong medication (30.1%), and wrong patient (28.3%) (Figure 2). From the total dosage errors, overdose accounted for 42.9%. Regarding the routes of medication administration, errors were most frequently committed by nurses when they administered medication through parenteral route 70.5% (Table 3).
Figure 1.
Frequency of medication administration errors in Northwest Amhara Region Referral Hospitals, Northwest Ethiopia, 2019 based on the questionnaire (n = 332 nurses).
Figure 2.
Types of medication administration errors in Northwest Amhara Region Referral Hospitals, Northwest Ethiopia, 2019 based on the questionnaire (n = 332 nurses).
Table 3.
Distribution of dosage and route errors in Northwest Amhara Region Referral Hospitals, Northwest Ethiopia, 2019 on the questionnaire (n = 332 nurses).
| Types of errors | Categories | Frequency | Percentage (100%) |
|---|---|---|---|
| Wrong dose (n = 119) | Over dose | 51 | 42.9 |
| Under dose | 49 | 41.1 | |
| Both | 19 | 16.0 | |
| Wrong route (n = 105) | Parenteral route | 74 | 70.5 |
| Enteral route | 19 | 18.1 | |
| Topical route | 12 | 11.4 |
Observational checklist results
To triangulate the results of self-administered questionnaires, observational data were collected by observing nurses during medication administration. Totally, 200 nurses were observed when they were administered medications. The results showed that only 10 (5%) of the 200 directly observed nurses administered medications without any breach in any of the six rights of medication administration. More than half (53%) of the observed nurses did not document administered medications and the patient’s condition on the patient chart and failed to administer the right dose of medication. One hundred and three (51.5%) of them failed to administer the right medication at the right time. Ninety-two (46.0%) and 48.5% of the observed nurses did not give medication to the right patient and administer medication through the right route, respectively (Table 4).
Table 4.
The level of adherence to the six rights of medication administration in Northwest Amhara Region Referral Hospitals, Northwest Ethiopia, 2019 based on the observation (n = 200 nurses).
| Variables | Response | Frequency (n = 200) | Percentage (100%) |
|---|---|---|---|
| Give medication to the right patient | Yes | 108 | 54.0 |
| No | 92 | 46.0 | |
| Administer the right medication | Yes | 97 | 48.5 |
| No | 103 | 51.5 | |
| Administer the right dose | Yes | 94 | 47 |
| No | 106 | 53 | |
| Administer through the right route | Yes | 103 | 51.5 |
| No | 97 | 48.5 | |
| Administer medication at the right time | Yes | 97 | 48.5 |
| No | 103 | 51.5 | |
| Document necessary information | Yes | 94 | 47 |
| No | 106 | 53 |
Factors associated with medication administration errors
Using bivariate logistic regression analysis, 10 variables were found to be significantly associated with MAEs based on the questionnaire. Stress, fatigue, nurse’s knowledge, and attitude, communication with other nurses and physicians, follow guidelines, place where nurses earn an educational qualification, interruption during medication administration, duty shift, and availability of guidelines for medication administration. In multivariable logistic regression analysis, factors significantly associated with MAEs were nurse’s knowledge, stress, communication with other nurses and physicians, interruption during medication administration, and duty shift. The odds of MAEs were nearly six times higher among nurses who had poor knowledge compared to those who had good knowledge (AOR = 5.98; 95% CI (2.39,14.94)). Similarly, the odds of MAEs were nearly three times higher among nurses who had poor communication as compared to nurses who had good communication with other nurses and physicians (AOR = 2.94; 95% CI (1.34, 6.46)). Nurses who were stressed were 5.4 times more likely to commit MAEs than those who were not stressed (AOR = 5.41; 95% CI (2.53, 11.57)). Nurses who were interrupted during medication administration were 4.7 times more likely to commit MAEs than nurses who were not interrupted (AOR = 4.70; 95% CI (2.42, 9.10)). Finally, the odds of MAEs were 2.8 times higher among nurses administering medication during the night time than those administering medication during the daytime (AOR = 2.79; 95% CI (1.42, 5.46)) (Table 5).
Table 5.
Bivariate and multivariable logistic regression analyses of factors associated with MAEs among nurses working in Northwest Amhara Region Referral Hospitals, Northwest Ethiopia, 2019 (n = 332 nurses).
| Variables | MAEs |
OR with 95% CI |
p value for AOR | ||
|---|---|---|---|---|---|
| Yes | No | Crude | Adjusted | ||
| Knowledge | |||||
| Poor | 80 | 13 | 8.85 (4.67, 16.80) | 5.98 (2.39, 14.94)a | <.001 |
| Good | 98 | 141 | 1 | 1 | |
| Attitude | |||||
| Poor | 92 | 44 | 2.67 (1.69, 4.22) | 0.63 (0.29, 1.36) | .238 |
| Good | 86 | 110 | 1 | 1 | |
| Communication | |||||
| Poor | 110 | 28 | 7.28 (4.38, 12.11) | 2.94 (1.34, 6.46)a | .007 |
| Good | 68 | 126 | 1 | 1 | |
| Stress | |||||
| Yes | 99 | 18 | 9.47 (5.34, 16.80) | 5.41 (2.53, 11.57)a | <.001 |
| No | 79 | 136 | 1 | 1 | |
| Fatigue | |||||
| Yes | 93 | 59 | 1.76 (1.14, 2.73) | 0.63 (0.31, 1.26) | .188 |
| No | 85 | 95 | 1 | 1 | |
| Educational qualification | |||||
| From private institutions | 38 | 10 | 3.91 (1.88, 8.15) | 2.35 (0.71, 7.83) | .163 |
| From gov't institutions | 140 | 144 | 1 | 1 | |
| Follow guidelines | |||||
| No | 75 | 35 | 2.48 (1.53, 4.00) | 1.02 (0.48, 2.17) | .956 |
| Yes | 103 | 119 | 1 | 1 | |
| Interruption | |||||
| Yes | 126 | 41 | 6.68 (4.13, 10.81) | 4.70 (2.42, 9.10)a | <.001 |
| No | 52 | 113 | 1 | 1 | |
| Availability of guidelines | |||||
| No | 101 | 58 | 2.17 (1.40, 3.37) | 1.58 (0.80, 3.10) | .186 |
| Yes | 77 | 96 | 1 | 1 | |
| Duty shift | |||||
| Night | 98 | 38 | 3.74 (2.34, 5.99) | 2.79 (1.42, 5.46)a | .003 |
| Day | 80 | 116 | 1 | 1 | |
Statistically significant at p value <.05.
Discussion
This study aimed to assess the magnitude of MAEs and its associated factors among nurses working in Northwest Amhara Region Referral Hospitals. The findings of this study showed that the magnitude of MAEs was 54% based on the questionnaires. This means that the magnitude of MAEs in the study area was high because errors should not be committed at the time of medication administration. This finding was relatively consistent with studies conducted in Felege Hiwot Referral Hospital (56.4%), in the intensive-care unit of Jimma University Specialized Hospital (51.8%), and South Africa (51%)9,11,22. On the other hand, it was lower than studies conducted in two public hospitals in Southern Ethiopia (71%) and in Tigray, Northern Ethiopia (62.7%)10,23. The possible explanation for this difference might be due to variations in the type of hospitals and researched clinical units. Previous studies were conducted in general hospitals and a single unit. But the current study was conducted in referral hospitals and incorporated all working units in the hospital. This might be because of the difference in educational level, experience level, and training of health professionals and the more developed and equipped facilities and guidelines in referral hospitals than in general hospitals.
The finding of this study was also lower than a study conducted in Nigeria (64%)24. This might be due to differences in sample size and study participants. The previous study was conducted among 75 pediatrics nurses, and the high magnitude of MAEs might be because medication dosing in pediatric patients considers body weight, which needs dosage calculation and hence can result in miscalculation. Similarly, the findings of this study were lower than studies conducted in Tehran (64.5%) and South Korea (69.6%)25,26. The possible justification for the difference might be the difference in sample size and type of hospitals where the study was conducted. The findings of this study were higher than studies conducted in Egypt (25%), Ghana (27.2%), and Southern Iran (37.6%)27–29. This discrepancy might be due to differences in clinical units included in the study, constituents of MAEs, and mechanisms put in place to minimize the occurrence of MAEs. Previous studies were conducted in a single unit. This might also be a consequence of the gap in the quality of health care.
In this study, a total of 200 nurses were observed. Of these, only 5% of the administered medications were administered without a breach of the six rights of medication. Similar findings were reported from studies conducted in the Felege Hiwot referral hospital (98.1%) and two public hospitals in southern Ethiopia (99.7%)10,11. The finding of this study was higher than studies conducted in the pediatric ward of Jimma University Specialized Hospital (89.9%) and two medical units of a tertiary teaching hospital in Madrid, Spain (86.6%)12,30. The difference might be due to variation in the study settings, in which the above studies were conducted in a single hospital and department. However, this study was conducted in two hospitals of entire wards that nurses are working. As the findings from both self-report (54%) and observation (95%) highlighted that the magnitude of MAE was high in the hospitals incorporated in the study. This might be because most of the participants made MAE but they do not report the errors they made.
Poor knowledge, poor communication with other nurses and physicians, interruption during medication administration, stress, and night shift were significantly associated with MAEs.
The odds of MAE were nearly six times higher among nurses who had poor knowledge compared to those who had good knowledge. This finding was supported by systematic reviews conducted in Australia and African hospitals as well as studies conducted in London and Tehran7,17,18,31. This might be because knowledge provides a base on which decisions are made and implemented, lack of which results in poor decision making and poor performance. Lack of familiarity with drugs’ generic and brand names, doses, and pharmacological properties of drugs can create confusion32. Medication administration is a complex procedure requiring significant intellectual activity and critical thinking, which involves a range of interrelated considerations, like correct dosage regime, side effects, and service user’s health presentation. Inadequate pharmacological knowledge, and inability to transfer that knowledge into clinical practice results in an error during medication administration33. To maintain medication administration safety, make good clinical decisions, and perform a professional role in managing drug therapy and reducing adverse effects and common drug errors, nurses need to have good pharmacological knowledge34. Poor communication with other nurses and physicians was also significantly associated with MAEs. The odds of MAE were nearly three times higher among nurses who had poor communication as compared to nurses who had good communication. This finding was supported by systematic reviews conducted in the United Kingdom and Australia as well as studies conducted in Tehran, London, Saudi Arabia, and Rwanda1,17–19,31,35. This might be due to incomplete exchange of information between team members and physicians regarding medications to be administered leads to incorrect treatment procedures, treatment delays, and delivery of incorrect medication to the patient. Miscommunication happens during the change of shifts when one caregiver transfers partial patient-related information36. Lack of patient and drug information and miscommunication of drug orders are dimensions of poor communication, which leads to MAEs37. The instances of poor communication may be reduced by increasing the transparency during information sharing between team members and physicians, setting predetermined roles for each department, and ensuring clear channels of communication between them36. Similarly, nurses who were interrupted during medication administration were 4.7 times more likely to commit MAEs than nurses who were not interrupted. This finding was supported by systematic reviews conducted in the United Kingdom, Australia, and African hospitals as well as studies conducted in Felege Hiwot referral hospital, Southern Ethiopia, Rwanda, Nigeria, and London1,7,10,11,17–19,24. This might be due to the medication administration process is serious and needs a nurse’s full attention. When nurses are interrupted while administering medication, they become distracted, their attention is diverted, and they lose their concentration which creates the risk of committing an error38. Interruptions involve anything that disturbs an individual from the current task by averting one's attention. Noise (alarms, ringing phones, and other clinicians) and other people, or electronic devices (text messages, e-mails, or other communication technologies) are considered sources of interruptions39. Interruptions are part of every nurse’s daily routine. However, it is better if nurses have professional attentiveness during the medication administration process to ensure patient safety. When due attentiveness is missing, errors happen40. Additionally, nurses who were stressed were 5.4 times more likely to commit MAEs than those who were not stressed. This finding was supported by a systematic review conducted in the United Kingdom and a study conducted in Saudi Arabia1,35. This might be because stress can have a significant impact on individual nurses and their ability to accomplish tasks specifically, poor decision making and lack of concentration which impair job performance and increase the chance of committing an error41. When nurses are suffering from stress, they can easily make mistakes in their judgment, decisions, and behavior, and result in errors. Stress can also result in suboptimal care, increased rates of safety breaches, and higher frequency of errors in everyday clinical practice42. In professional nursing, stress may result from work overload, shortage of staff, conflicts with physicians or coworkers, pressure from family members, life and death situations, and prolonged duty hours43. There are some simple common methods used by nurses to reduce and manage stress like relaxation, exercise, altering the situation, expressing feelings instead of bottling them up, and better time management44. This study also showed that the time of medication administration was significantly associated with MAEs. Nurses who administered medication at night time were 2.8 times more likely to commit MAEs than nurses administering medication during the day time. This finding was supported by studies conducted in the Felege Hiwot referral hospital of Ethiopia and London11,18. This might be due to sleep deprivation, loss of concentration, and exhaustion experienced by nurses during the night time. Night-shift nurses who work during night time are at greatest risk of sleep deprivation as they have the challenge of their work schedules going against their body’s natural circadian rhythm45. This can result in MAEs due to impaired mathematical skills as a result of mental fatigue or decreased observational skills due to fatigue46.
This study has some limitations. The study was based on self-reported information and observation that may be prone to reporting bias because of the respondent’s interpretation of the questionnaire or desire to report their feelings and observer bias. There might also recall bias because a 12-month recall for the questionnaires is a long period.
Strength of study: The response rate was high.
Conclusions
The magnitude of MAE was high in the Northwest Amhara Region Referral Hospitals. Poor knowledge, poor communication with other nurses and physicians, interruption during medication administration, stress, and night shift were significantly associated with MAEs. Strengthening institutional medication administration regulations and guidelines and minimizing interruption during medication administration would help minimize MAEs. This finding is an essential first step toward the safe and appropriate administration of medication which in turn improves patient safety. The finding will also provide necessary information for health policy-makers to design and implement effective interventions to reduce the negative impact of MAEs on patients and the healthcare system.
Acknowledgements
The authors are grateful to the University of Gondar, Debre Markos, and the University of Gondar hospital clinical directors and nursing coordinators, data collectors, and study participants.
Transparency
Declaration of funding
No funding has been received for the conduct of this study and/or preparation of this manuscript.
Declaration of financial/other relationships
The contents of the paper and the opinions expressed within are those of the authors, and the authors decided to submit the manuscript for publication.
References
- 1.Keers RN, Williams SD, Cooke J, et al. . Causes of medication administration errors in hospitals: a systematic review of quantitative and qualitative evidence. Drug Saf. 2013;36(11):1045–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keers RN, Williams SD, Cooke J, et al. . Prevalence and nature of medication administration errors in health care settings: a systematic review of direct observational evidence. Ann Pharmacother. 2013;47(2):237–256. [DOI] [PubMed] [Google Scholar]
- 3.Dabaghzadeh F, Rashidian A, Torkamandi H, et al. . Medication errors in an emergency department in a large teaching hospital in Tehran. Iran J Pharm Res. 2013;12(4):937. [PMC free article] [PubMed] [Google Scholar]
- 4.Yousefi M, Abed Saeedi Z, Maleki M, et al. . Frequency and causes of medication errors of nurses in different shift work in educational hospitals affiliated to Shahid Beheshti University of Medical Sciences. J Shahid Beheshti School Nurs Midwifery. 2014;24(86):27–34. [Google Scholar]
- 5.Zaree TY, Nazari J, Jafarabadi MA, et al. . Impact of psychosocial factors on the occurrence of medication errors among Tehran Public Hospitals Nurses by evaluating the balance between effort and reward. Saf Health Work. 2018;9(4):447–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO . Patient safety: making health care safer; 2017. [Google Scholar]
- 7.Mekonnen AB, Alhawassi TM, McLachlan AJ, et al. . Adverse drug events and medication errors in African hospitals: a systematic review. Drugs Real World Outcomes. 2018;5(1):1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al Tehewy M, Fahim H, Gad NI, et al. . Medication administration errors in a university hospital. J Patient Saf. 2016;12(1):34–39. [DOI] [PubMed] [Google Scholar]
- 9.Agalu A, Ayele Y, Bedada W, et al. . Medication administration errors in an intensive care unit in Ethiopia. Int Arch Med. 2012;5(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alemu W, Belachew T, Yimam I.. Medication administration errors and contributing factors: a cross-sectional study in two public hospitals in Southern Ethiopia. Int J Afr Nurs Sci. 2017;7(1):68–74. [Google Scholar]
- 11.Feleke SA, Mulatu MA, Yesmaw YS.. Medication administration error: magnitude and associated factors among nurses in Ethiopia. BMC Nurs. 2015;14(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feleke Y, Girma B.. Medication administration errors involving pediatric in-patients in a hospital in Ethiopia. Trop J Pharm Res. 2010;9(4):401–407. [Google Scholar]
- 13.Dedefo MG, Mitike AH, Angamo MT.. Incidence and determinants of medication errors and adverse drug events among hospitalized children in West Ethiopia. BMC Pediatr. 2016;16(1):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ayuk Agbor G. A literature review of medication errors in the United States of America; 2016. [Google Scholar]
- 15.Mahajan R. Medication errors: can we prevent them? Oxford University Press; 2011. [Google Scholar]
- 16.Karavasiliadou S, Athanasakis E.. An inside look into the factors contributing to medication errors in the clinical nursing practice. Health Sci J. 2014;8(1):32–44. [Google Scholar]
- 17.Alomari A, Wilson VJ, Davidson PM, et al. . Families, nurses and organizations contributing factors to medication administration error in pediatrics: a literature review. iPDc. 2015;5(1):1–14. [Google Scholar]
- 18.Alqasoumi A. Evaluation of types & causes of dose administration errors. London: King's College London; 2016. [Google Scholar]
- 19.Nkurunziza A, Chironda G, Mukeshimana M.. Perceived contributory factors to medication administration errors (MAEs) and barriers to self-reporting among nurses working in pediatric units of selected referral hospitals in Rwanda. Int J Res Med Sci. 2018;6(2):401–407. [Google Scholar]
- 20.The Marlin Company NH, CT, and the American Institute of Stress Y, NY. The Workplace Stress Scale ; 2001. [Google Scholar]
- 21.Drent M, Lower EE, De Vries J.. Sarcoidosis-associated fatigue. Eur Respir Soc. 2012;40:255–263. [DOI] [PubMed] [Google Scholar]
- 22.Elliott R, Camacho E, Campbell F, et al. Prevalence and economic burden of medication errors in the NHS in England. Rapid evidence synthesis and economic analysis of the prevalence and burden of medication error in the UK; 2018. [Google Scholar]
- 23.Baraki Z, Abay M, Tsegay L, et al. . Medication administration error and contributing factors among pediatric inpatient in public hospitals of Tigray, northern Ethiopia. BMC Pediatr. 2018;18(1):321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oshikoya KA, Oreagba IA, Ogunleye OO, et al. . Medication administration errors among paediatric nurses in Lagos public hospitals: an opinion survey. Int J Risk Saf Med. 2013;25(2):67–78. [DOI] [PubMed] [Google Scholar]
- 25.You M-a, Choe M-H, Park G-O, et al. . Perceptions regarding medication administration errors among hospital staff nurses of South Korea. Int J Qual Health Care. 2015;27(4):276–283. [DOI] [PubMed] [Google Scholar]
- 26.Cheragi MA, Manoocheri H, Mohammadnejad E, et al. . Types and causes of medication errors from the nurse's viewpoint. Iran J Nurs Midwif Res. 2013;18(3):228. [PMC free article] [PubMed] [Google Scholar]
- 27.Vazin A, Zamani Z, Hatam N.. Frequency of medication errors in an emergency department of a large teaching hospital in southern Iran. Drugs Healthc Patient Saf. 2014;6:179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Acheampong F, Tetteh AR, Anto BP.. Medication administration errors in an adult emergency department of a tertiary health care facility in Ghana. J Patient Saf. 2016;12(4):223–228. [DOI] [PubMed] [Google Scholar]
- 29.Abusaad EFES, Etawy EA.. Medication administration errors at Children’s University hospitals: nurse's point of view. J Nurs Health Sci. 2015;4(1):51–60. [Google Scholar]
- 30.Rodriguez-Gonzalez CG, Herranz-Alonso A, Martin-Barbero ML, et al. . Prevalence of medication administration errors in two medical units with automated prescription and dispensing. J Am Med Inform Assoc. 2012;19(1):72–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ehsani SR, Cheraghi MA, Nejati A, et al. . Medication errors of nurses in the emergency department. J Med Ethics Hist Med. 2013;6:11. [PMC free article] [PubMed] [Google Scholar]
- 32.Kosari S. Medication errors in nursing homes: the role of pharmacological knowledge. Crit Care Nurs. 2018;1(1):9–10. [Google Scholar]
- 33.Hemingway S, Baxter H, Smith G, et al. . Collaboratively planning for medicines administration competency: a survey evaluation. J Nurs Manag. 2011;19(3):366–376. [DOI] [PubMed] [Google Scholar]
- 34.Wright K. The role of nurses in medicine administration errors. Nurs Stand. 2013;27(44):35–40. [DOI] [PubMed] [Google Scholar]
- 35.Qrishah A, Hassan M. The factors associated with the occurrence of medication errors in the Ministry of Health Hospitals in Saudi Arabia: a cross-sectional study of nurses; 2017. [Google Scholar]
- 36.Kain Z. Effects of poor communication in hospitals; 2017. [Google Scholar]
- 37.Minimizing medication errors : communication about drug orders American Academy of Ophthalmology; 2015. [Google Scholar]
- 38.Wines DR. Interruptions and distractions of nurses during medication administration on a medical-surgical unit; 2013. [Google Scholar]
- 39.Magrabi F, Li S, Dunn A, et al. . Challenges in measuring the impact of interruption on patient safety and workflow outcomes. Methods Inf Med. 2011;50(5):447–453. [DOI] [PubMed] [Google Scholar]
- 40.Buchini S, Quattrin R.. Avoidable interruptions during drug administration in an intensive rehabilitation ward: improvement project. J Nurs Manag. 2012;20(3):326–334. [DOI] [PubMed] [Google Scholar]
- 41.Akweenda FM, Cassim N, Karodia AM.. Investigating work-related stress and its impact on the performances of registered nurses employed at Katutura State Hospital in Windhoek, Namibia. Kuwait Chapt Arab J Business Manage Rev. 2016;33(3421):1–29. [Google Scholar]
- 42.Adib-Hajbaghery M, Khamechian M, Alavi NM.. Nurses’ perception of occupational stress and its influencing factors: a qualitative study. Iran J Nurs Midwifery Res. 2012;17(5):352–359. [PMC free article] [PubMed] [Google Scholar]
- 43.Khan N, Anwar H, Sayed M.. Prevalence of stress factors in nurses in Leady Reading Hospital (LRH), Khyber Teaching Hospital (KTH), and Hayatabad Medical Complex (HMC) Hospitals, Peshawar, KPK. Int J Innov Res Dev. 2015;4(4). [Google Scholar]
- 44.Onasoga Olayinka A, Osamudiamen OS, Ojo A.. Occupational stress management among nurses in a selected hospital in Benin city, Edo State, Nigeria. Eur J Exp Biol. 2013;3(1):473–481. [Google Scholar]
- 45.Johnson AL, Brown K, Weaver MT.. Sleep deprivation and psychomotor performance among night-shift nurses. AAOHN J. 2010;58(4):147–156. [DOI] [PubMed] [Google Scholar]
- 46.Bae S-H. Presence of nurse mandatory overtime regulations and nurse and patient outcomes. Nurs Econ. 2013;31(2):59–68. [PubMed] [Google Scholar]