EXECUTIVE SUMMARY
The COVID-19 pandemic, with its resultant social distancing, has disrupted the delivery of healthcare for both patients and providers. Fortunately, changes to legislation and regulation in response to the pandemic allowed Emory Healthcare to rapidly implement telehealth care. Beginning in early March 2020 and continuing through the initial 2-month implementation period (when data collection stopped), clinicians received telehealth training and certification. Standard workflows created by means of a hub-and-spoke operational model enabled rapid sharing and deployment of best practices throughout the system’s physician group practice. Lean process huddles facilitated successful implementation. In total, 2,374 healthcare professionals, including 986 attending physicians, 416 residents and fellows, and 555 advanced practice providers, were trained and certified for telehealth; 53,751 new- and established-patient audio–video telehealth visits and 10,539 established-patient telephone visits were performed in 8 weeks for a total of 64,290 virtual visits. This initiative included a new COVID-19 virtual patient clinic that saw 705 patients in a 6-week period. A total of $14,662,967 was charged during this time; collection rates were similar to in-person visits. Initial patient satisfaction scores were equivalent to in-person visits. We conclude that rapid deployment of virtual visits can be accomplished through a structured, organized approach including training, certification, and Lean principles. A hub-and-spoke model enables bidirectional feedback and timely improvements, thus facilitating swifter implementation and a quick rise in patient volume. Financial sustainability is achievable, but to sustain that, telehealth requires the support of continued deregulation by legislative and regulatory bodies.
BACKGROUND
The COVID-19 pandemic has disrupted the delivery of emergent, urgent, and elective medical care models throughout the world. Among many challenges are the extensive requirements for personal protective equipment (PPE; Ranney et al., 2020) and severe constraints on the traditional interactions among clinicians, allied health professionals, and patients. Social distancing, an effective way to limit viral spread (Wilder-Smith & Freedman, 2020), has unfortunately also resulted in the cancelation of thousands of elective visits and procedures (Kutikov et al., 2020). Therefore, patients and families may not receive the care and treatment they need if there are no alternatives to in-person care.
Telehealth has been established in acute intervention-based services such as tele-ICU (Trombley et al., 2018), telestroke (Nguyen-Huynh et al., 2018), and telepsychiatry (Reinhardt et al., 2019)—among many others. Outpatient deployments in specialties such as ophthalmology and primary care also suggest that telehealth care is at least as effective as traditional face-to-face care and is cost effective (Bashshur et al., 2016; Maa et al., 2020). The advent of multiple care models in telehealth effectively positions the deployment of these technologies to provide additional services and solve access problems caused by COVID-19 (Hollander & Carr, 2020). Organizations that have invested significantly in telehealth infrastructure and care pathways are more readily able to respond to the struggles created by the COVID-19 pandemic (Hollander & Carr, 2020); conversely, health systems with minimal to no underlying infrastructure may be at a disadvantage to implement telehealth care models amid current challenges.
Emory Healthcare (EHC) in Atlanta, Georgia, is an academic medical center with 11 hospitals and more than 250 clinical sites delivering care for more than 820,000 patients annually. Investments in telehealth prior to the COVID-19 pandemic were limited to the deployment of tele-ICU at multiple hospitals (2014), telenephrology at two regional hospitals (2017), and telepsychiatry and teleneurology at two individual hospitals (2019). A small centralized group—the EHC telehealth team—was formed in 2019 to build up telehealth in a stepwise fashion based on use-case needs, but the lack of appropriate payment models and regulatory burdens prevented wide deployment of telehealth. The advent of the COVID-19 pandemic crisis suddenly required a massive effort to expand outpatient telehealth within weeks. This article describes the model that was used to achieve rapid implementation in EHC’s physician group practice (PGP).
METHODS
Training, Certification, and Platform
In March 2020, soon after the nature of the pandemic became apparent, a systemwide telehealth policy was created to grant telehealth privileges. The policy was created by the EHC system’s chief medical officer (CMO) and associate CMO, and then enacted by the CMOs of all the hospitals and PGP. The policy allowed for a one-time training and certification program for EHC providers that allowed faculty, employed, and affiliated physicians to deploy telehealth services as part of their practice, obviating the need for renewal of telehealth privileges every 2 years. Advanced practice providers (APPs) were given access to the training program and certification as well.
The program was delivered in three modules that already had been in preparation but were rapidly finalized when the pandemic started. Module 1 promoted a basic understanding of telehealth based on the state of Georgia’s definition, the benefits of telehealth, basic applications, definitions, types of telehealth, licensing requirements, and EHC standards for handling personal health information. Module 2 defined state and federal legislation and regulations regarding licensure, billing, coding, and allowable practice. Module 3 provided basics about the pre-, intra-, and post-telehealth visit processes. Providers typically completed each module in approximately 1 hour. The modules were designed to ensure that practitioners could safely apply telehealth in the right-use cases, complying with laws and understanding the elements of telehealth visits from start to finish.
Upon completion of all modules, providers were required to pass a 10-question assessment and attest that they would obtain in-person training. Zoom (Zoom Video Communication Inc.) was the platform for conducting telehealth visits, as EHC already had a HIPAA-compliant, enterprise license agreement with Zoom. To maintain social distance from one another, physicians, APPs, and facilitators were taught virtually how to use Zoom. These first learners were selected based on interest, technological skills, and ability to train others. They completed their initial training within 10 days of system telehealth go-live. The urgency to deploy superseded testing of these learners who went on to train others, although their knowledge and skills were later refined by the EHC telehealth team through virtual nightly meetings during the next few weeks.
Adopting Hub-and-Spoke Deployment
We adopted a hub-and-spoke model to scale the effectiveness of the EHC telehealth team (Figure 1). The small team was the hub; each section, division, or practice was a spoke. Chairpersons and service line chiefs were highly supportive and engaged. Each spoke included a dyad of at least one administrative facilitator and one physician or APP champion; larger groups had multiple dyads.
FIGURE 1.
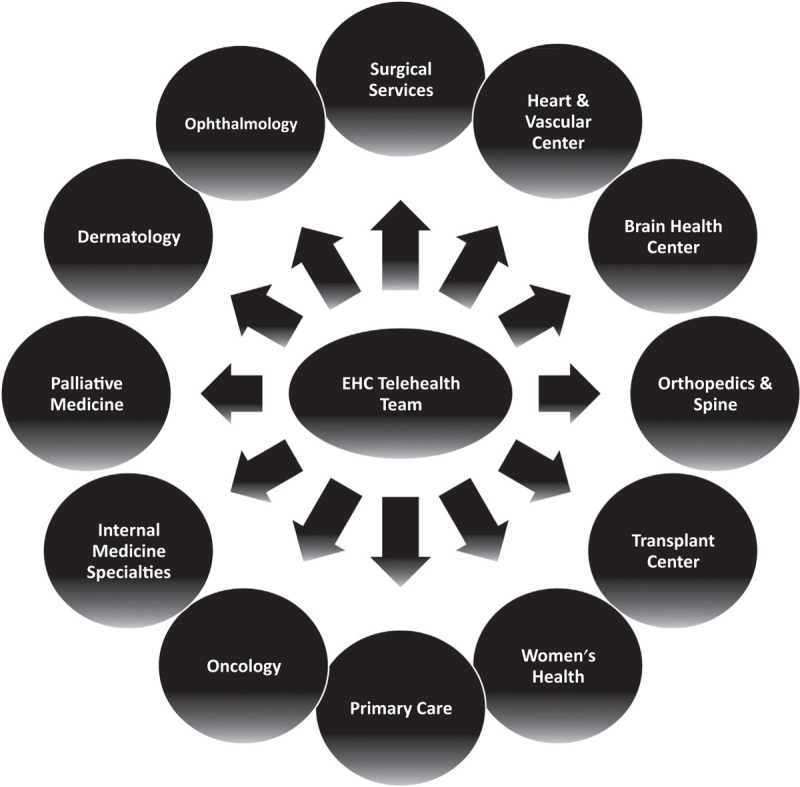
The Hub-and-Spoke Model of the EHC Telehealth Team and Participants
Delivering Outpatient Telehealth
As community spread of COVID-19 unfolded in early March, elective visits were canceled or suspended to protect patients and conserve PPE. Each EHC group developed a plan, with guidance from the EHC telehealth team, to increase outpatient telehealth visits to maintain continuity of care with existing patients and provide access for new patients. Workflows were developed based on the EHC scheduling system (Cerner, GE Centricity Business) that allowed new and established video visits as well as telephone visits. Providers reviewed existing schedules and determined whether patients should be seen in person or switched to audio–video or phone visits. Administrative staff contacted patients for scheduling, assessed and confirmed willingness to engage in a telehealth visit, and told patients how to download and log into the Zoom application. Clinical staff assisted physicians in the rooming process via Zoom or phone by obtaining patient-reported vital signs (e.g., blood pressure using a home sphygmomanometer), medical history, allergies, current medications, social history, and a review of systems.
Physicians performed examinations via Zoom, drawing as needed from guidance developed and made available by other EHC physicians who were more familiar with telehealth. Facilitators and physician champions performed rapid tests of change with continuous quality improvement methodology to achieve best outcomes. One instance of this led to establishing a central group of technical staff on the EHC PGP access team, who would assist patients requiring more help with technology when administrative staff were unsuccessful. Other examples included additions to the standard templates in the electronic health record (EHR) system: the words “patient-reported” added to documentation of vital signs and verification of patient location in Georgia to facilitate compliance with state licensure. To address the safety problem of patients driving during their telehealth visits, administrative staff also inserted specific, standard language into scripts to prohibit driving during audio–video interaction, and all providers were instructed to promptly end a visit when patients were driving.
Best-Practice Sharing
The EHC telehealth team conducted nightly office hours during the first weeks of deployment to demonstrate workflows and answer questions. The bidirectional communication between hub and spokes aided the understanding of local problems and facilitated problem-solving by the hub or other spoke sites that had earlier identified and resolved similar problems.
Screen sharing was extremely important for these meetings, which included Zoom functionality demonstrations and presentations of refined standard work documents. Each meeting was recorded for later distribution. The meetings also included situational awareness report-outs that followed EHC’s systemwide Lean huddle process. These report-outs covered updated training numbers; outpatient practice status; and defects in safety, methods, equipment, staffing, or supply concerns for each spoke (See Figure S1, published online as Supplemental Digital Content at). All materials were shared on the organization’s intranet. This knowledge sharing optimized workflows and helped new users quickly operationalize telehealth. In May, the nightly meetings shifted to a weekly schedule.
Analyzing the Data
Telemedicine visits were labeled in scheduling software as “new video visit,” “new prolonged video visit,” “new extended video visit,” “established video visit,” “established extended video visit,” “established prolonged video visit,” “established telephone visit,” “annual wellness video visit,” “consult video visit,” and “second surgical opinion video visit” to provide clarity to providers and support data tracking. MicroStrategy business analytics software (MicroStrategy Inc.) was used to access data in the EHC clinical data warehouse and EPSi financial system (Allscripts Healthcare). Microsoft Excel (Microsoft Corp.) was used to tabulate and graph data.
RESULTS
Between March 10 and May 6, 2,374 individuals completed training and certification (Table 1). Most trainees were attending physicians (42%), followed by APPs (23%). In response to the trainees’ interest, a graduate medical education policy was later developed that allowed deployment of telehealth under guidance of program directors and staffing attendings; fellows and residents were 18% of those trained. Nurses, medical assistants, athletic trainers, and other healthcare professionals (e.g., administrators, coordinators) were not required to be trained because they were not responsible for clinical decision making or compliance with telehealth visits; these groups made up 18% of those trained. The vast majority of physicians and APPs for whom outpatient practice was necessary completed the training. Barriers to training included preference to continue seeing patients in person upon reopening of services and difficulty accessing the training modules.
Table 1.
Numbers of Emory Healthcare Physicians and Staff Trained March 10–May 6, 2020, Through Healthstream Learning Center Modules
| Physician | APP | Nurse | MA&AT | Trainees | Other | Total | |
|---|---|---|---|---|---|---|---|
| The Emory Clinic Faculty Practice | 858 | 469 | 36 | 22 | – | 236 | 1,621 |
| Emory Specialty Associates | 128 | 72 | 93 | 9 | – | 9 | 311 |
| Graduate Medical Education | – | – | – | – | 416 | – | 416 |
| Emory Hospitals | – | 14 | 4 | 5 | – | 3 | 26 |
| Total number | 986 | 555 | 133 | 36 | 416 | 248 | 2,374 |
| Total percentage | 42% | 23% | 6% | 2% | 18% | 10% | 100% |
Note. APP = advanced practice provider; MA = medical assistant; AT = athletic trainer.
An exponential increase of outpatient appointments was seen in the first weeks after training deployment. Between March 16 and May 6, 64,290 telehealth visits took place—53,751 (84%) were audio–video visits (Figure 2) and 10,539 (16%) were telephonic. The top five performance groups included primary care (34%), orthopedics and spine (11%), neurology (7%), psychiatry (4%), and endocrinology (3%). Primary care also developed a telehealth clinic for outpatient COVID-positive healthcare workers and patients who were referred by the outpatient nasal-swab diagnostic clinic or discharged from the emergency department (ED). This clinic completed 705 audio–video and telephone visits in its first 8 weeks.
FIGURE 2.
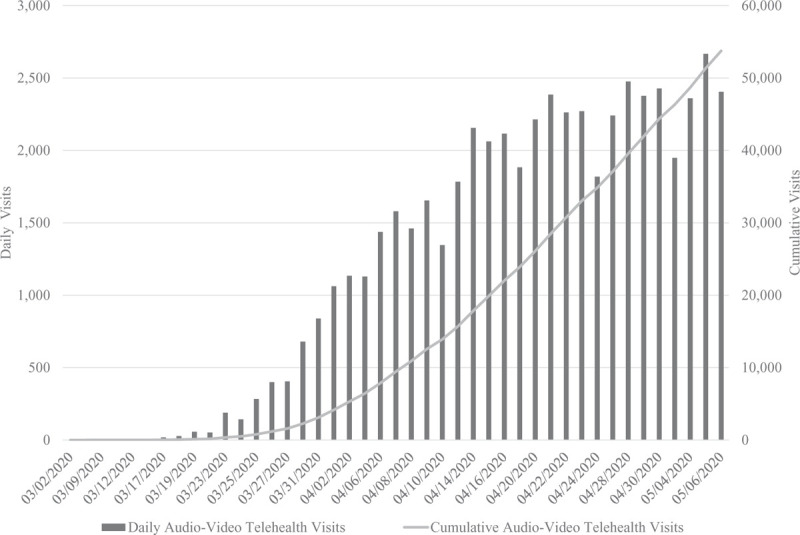
Emory Healthcare Physician Group Practice Outpatient Telehealth Encounters, March 2, 2020–May 6, 2020
Patient barriers to audio–video visits included patient preference, lack of access to technology, and limited internet access in certain rural areas. Practice barriers included the need to redo providers’ scheduling templates to maximize utilization of patient slots. Operational challenges included
the inability of patients to connect to the audio–video visit, primarily because of user errors, which prompted a telephone visit;
the delivery of a physical prescription to certain patients (accomplished by means of fax or the EHR system’s patient portal); and
the completion of consent forms, which required signatures from the patient and provider (routed through fax or the EHR system’s patient portal and delivered back to the practice).
The financial impact of telehealth also was tracked March 16 to May 6. During that period, a total of $14,662,967 was charged. Approximately 73% of charges were billed; the others were held for one or more of three reasons: (1) review by patient financial services, (2) missing charges, and (3) holds on telephone billing because some payers requested that telephone visits be billed as evaluation and management codes, necessitating manual review of each claim. Of the billed claims, HMO/PPO/other commercial plans represented 57%, Medicare 35%, Medicaid 4%, and self-pay 4%. The collection yield rate of the submitted charges was 95%—approximately 3% higher than in-person visits, likely because payers waived patient payments related to these visits. Most denials by payers cited a lack of information needed for adjudication of claim and missing charges.
DISCUSSION
The COVID-19 crisis has forced rapid adoption of telehealth among healthcare providers. Reasons to adopt telehealth include social distancing protocols that isolate patients and families from their physicians and PPE conservation. EHC leadership has recognized the opportunity telehealth can provide and facilitated major operational changes to support successful adoption. These changes include policy development and enactment; standardized training, assessment, and certification; leadership’s expectation of providers to shift from in-person care to telehealth; and the provision of resources necessary to accomplish these changes. Employment of a hub-and-spoke operational model has been a key to the success of the launch of telehealth within a 2-month time frame. However, variations in adoption and performance have occurred. EHC sections able to rapidly revise their scheduling templates have achieved early success. Sections that require in-person examinations for certain visits (e.g., ophthalmology, oral maxillofacial surgery, gynecology) have been slower to implement, as have sections whose providers routinely perform procedures with visits (e.g. otolaryngologists who visualize nasal passages using endoscopy).
As a Lean organization, EHC allows the people closest to the work to make changes that facilitate the best possible outcomes for its patients and its people (Aij et al., 2015). The EHC telehealth team uses documented Lean methodology in healthcare to implement this mindset (Albanese et al., 2014). As such, sections of EHC have developed resources and practices that can be shared through EHC’s intranet and weekly report-outs. Best practices are disseminated through the facilitator–physician/APP dyad to other sections for implementation. Lines of communication remain open, with questions handled by appropriate personnel. “Go and see” sharing among sections is accomplished through Zoom; principal elements of Lean, including visual controls, standard work documents, situational awareness, and leadership discipline, allow the continued rapid growth of telehealth at EHC.
External factors facilitating the uptake include the sweeping regulatory and legislative changes instituted by the Centers for Medicare & Medicaid Services and Congress. These include payment at parity for almost all patient care services that formerly required in-person visit, along with adoption of similar guidance by other commercial payers. Also, electronic visits through a patient portal are payable by Centers for Medicare & Medicaid Services (a regulatory change made at the beginning of 2020, before the COVID-19 pandemic). In addition, physicians and APPs can now prescribe schedule II to V medications in states that allow this practice. National regulation of medicine is not uniform, with some states requiring providers to obtain full state licenses to practice. Therefore, usage of telehealth has not yet reached its widest potential.
Concerns remain regarding the future of telehealth in the United States. Although the federal government has been swift to enact change in response to the pandemic, it is possible past regulations that discouraged telehealth will be reenacted. Healthcare providers may again have to deal with the inability to see patients at home rather than a clinic when they start a visit, a lack of payments for telephone visits when audio–video visits are not possible with certain patients, and restrictions on prescriptions for scheduled substances. While the relaxation of regulations around these three barriers and success in retrieving early payments by insurers have driven telehealth at EHC during the pandemic, the tremendous effort and resources required to maintain patient access through telehealth will be undone if these barriers return—in addition to the loss of patient goodwill achieved with the convenience of telehealth. These negative outcomes also threaten newly established follow-up mechanisms for the chronically ill who have difficulty attending in-person appointments and others who lack transportation.
The next step for EHC will be to add acute care telehealth and maximize patient access to all venues. This will include establishing remote monitoring protocols for high-risk patients and those with chronic conditions, image capturing and forwarding methodologies for dermatology and other sections, and mobile health. Ultimately, the immediate telehealth wins of PPE conservation and minimized spread of infection are setting the foundation for the future of better access to care.
There are potential limitations to our telehealth model. Success is definite but early; results are expected to be maintained but require disciplined follow-through. The additions of acute care telehealth in the ED and specialty consultation on the inpatient floors are expanding the bandwidth required of the EHC telehealth team; therefore, ensuring that the integrity of the hub-and-spoke model holds up to ensure high degrees of quality and safety is critical. Also, initial enthusiasm is high as clinicians realize the importance of telehealth in their practice. As this enthusiasm wanes, appropriate attention to performance practice evaluation will be vital. Moreover, new trainees require the hardwiring of telehealth protocols, with continued vigilant oversight by program directors.
CONCLUSION
The rapid systemwide deployment of outpatient telehealth at EHC has succeeded with a standardized approach using a hub-and-spoke model supported by leadership. Elements of the Lean operating system, including huddles and standardized work, have been critical. However, the regulatory and legislative changes in reimbursement that have facilitated the adoption of telemedicine must continue to support patient access through telemedicine care beyond the COVID-19 public health emergency.
Supplementary Material
Footnotes
Dr. Esper has received remuneration for medicolegal consulting.
The authors declare no conflicts of interest.
Contributor Information
Gregory J. Esper, Emory Healthcare (EHC) Office of Quality and Risk, EHC Telehealth Team, and Emory University School of Medicine Department of Neurology, Atlanta, Georgia.
Robert L. Sweeney, EHC Telehealth Team
Emmeline Winchell, EHC Telehealth Team.
J. Michael Duffell, EHC Telehealth Team.
Sarah C. Kier, EHC Telehealth Team and Physician Group Practice, Atlanta, Georgia
Hallie W. Lukens, EHC Physician Group Practice
Elizabeth A. Krupinski, EHC Telehealth Team and Emory University School of Medicine Department of Radiology and Imaging Sciences.
REFERENCES
- Aij K. H., Visse M., Widdershoven G. A. (2015). Lean leadership: An ethnographic study. Leadership in Health Services (Bradford, England), 28(2), 119–134. 10.1108/LHS-03-2014-0015 [DOI] [PubMed] [Google Scholar]
- Albanese C. T., Aaby D. R., Platchek T. S. (2014). Advanced Lean in healthcare. CreateSpace Independent Publishing Platform. [Google Scholar]
- Bashshur R. L., Howell J. D., Krupinski E. A., Harms K. M., Bashshur N., Doarn C. R. (2016). The empirical foundations of telemedicine interventions in primary care. Telemedicine Journal and e-Health, 22(5), 342–375. 10.1089/tmj.2016.0045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander J. E., Carr B. G. (2020). Virtually perfect? Telemedicine for COVID-19. New England Journal of Medicine, 382(18), 1679–1681. 10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- Kutikov A., Weinberg D. S., Edelman M. J., Horwitz E. M., Uzzo R. G., Fisher R. I. (2020). A war on two fronts: Cancer care in the time of COVID-19. Annals of Internal Medicine, 172(11), 756–758. 10.7326/M20-1133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maa A. Y., Medert C. M., Lu X., Janjua R., Howell A. V., Hunt K. J., McCord S., Giangiacomo A., Lynch M. G. (2020). Diagnostic accuracy of technology-based eye care services: The technology-based eye care services compare trial, Part I. Ophthalmology, 127(1), 38–44. 10.1016/j.ophtha.2019.07.026 [DOI] [PubMed] [Google Scholar]
- Nguyen-Huynh M. N., Klingman J. G., Avins A. L., Rao V. A., Eaton A., Bhopale S., Kim A. C., Morehouse J. W., Flint A. C. (2018). KPNC Stroke Force Team. Novel telestroke program improves thrombolysis for acute stroke across 21 hospitals of an integrated healthcare system. Stroke, 49(1), 133–139. 10.1161/STROKEAHA.117.018413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranney M. L., Griffeth V., Jha A. K. (2020). Critical supply shortages: The need for ventilators and personal protective equipment during the COVID-19 pandemic. New England Journal of Medicine, 382(18), e41. 10.1056/NEJMp2006141 [DOI] [PubMed] [Google Scholar]
- Reinhardt I., Gouzoulis-Mayfrank E., Zielasek J. (2019). Use of telepsychiatry in emergency and crisis intervention: Current evidence. Current Psychiatry Reports, 21(8), 63 10.1007/s11920-019-1054-8 [DOI] [PubMed] [Google Scholar]
- Trombley M. J., Hassol A., Lloyd J. T., Buchman T. G., Marier A. F., White A., Colligan E. (2018). The impact of enhanced critical care training and 24/7 (tele-ICU) support on Medicare spending and postdischarge utilization patterns. Health Services Research, 53(4), 2099–2117. 10.1111/1475-6773.12821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilder-Smith A., Freedman D. O. (2020). Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. Journal of Travel Medicine, 27(2) 10.1093/jtm/taaa020 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


