Abstract
Background & Aims:
Patient satisfaction is an important, but largely overlooked, component of management of functional gastrointestinal disorders. We aimed to identify demographic, clinical, psychosocial, and health-care use factors associated with satisfaction of patients with irritable bowel syndrome (IBS).
Methods:
We collected data from consecutive patients at an outpatient gastroenterology clinic of a tertiary care center from 2017 through 2019; the patients completed an electronic symptom survey at their initial visit and 3–6 months later. Patients were included in the study if they met Rome IV criteria for IBS with no organic cause for their symptoms. Patient satisfaction was measured using the irritable bowel syndrome satisfaction with care scale. We collected demographic, clinical, psychosocial, and healthcare use information from survey responses and review of medical records.
Results:
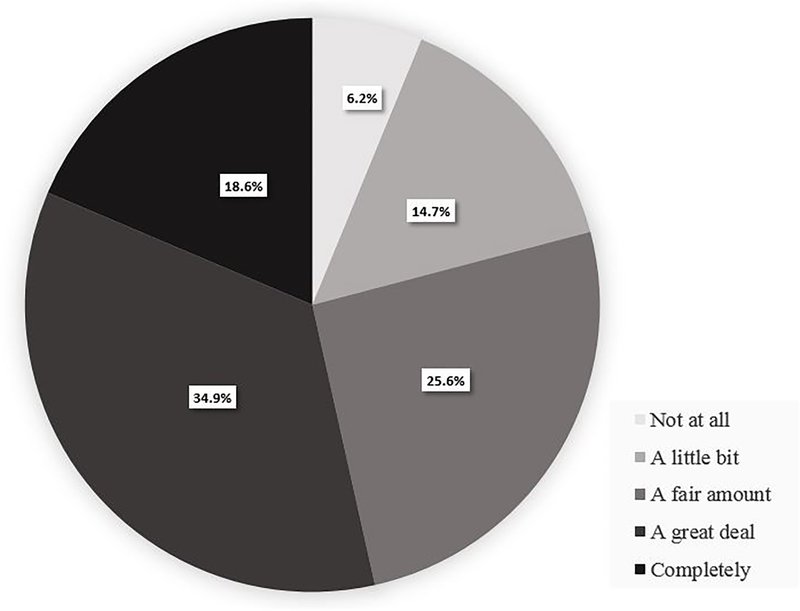
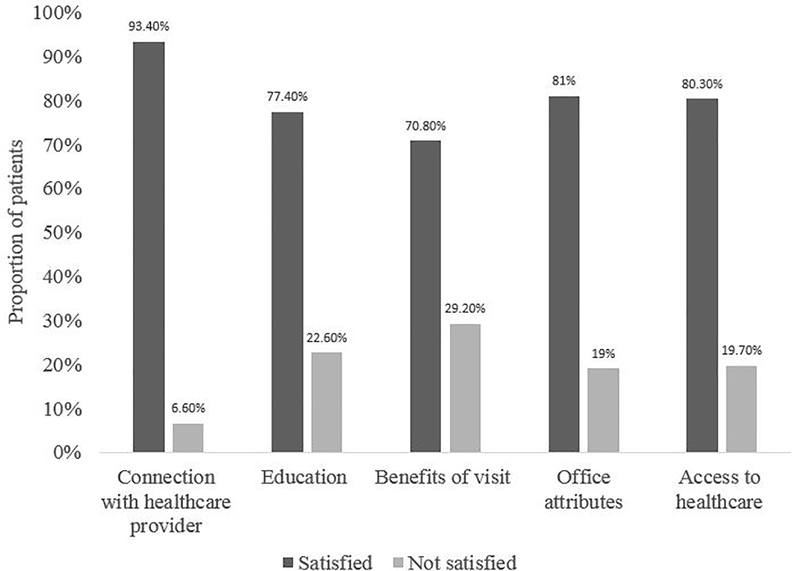
Of the 137 patients who completed the study, most were satisfied a great deal (34.9%) or completely (18.6%), whereas 6.2% were not satisfied at all and 14.7% were a little satisfied. Among the 5 satisfaction subscales, the highest proportion of patients were satisfied with connection with their provider (93.4%). The subscale benefits of the visit had the lowest satisfaction rate (70.8%). Factors associated with overall satisfaction scores in the 3–6 months after initial consultation included decreased severity of IBS, higher number of follow-up gastroenterology visits, higher number of diagnostic tests during the follow-up period, and higher number of recommendations made at initial visit. Additionally, lower depression score at initial visit associated with higher satisfaction after 3–6 months.
Conclusions:
Based on a survey of 137 patients with IBS, factors associated with satisfaction 3–6 months after establishing care with a gastroenterologist include reduced IBS severity, lower depression score at initial visit, higher number of recommendations, and higher number of follow-up gastroenterology visits.
Keywords: FGID, patient-reported outcomes, psychologic factors, treatment
Introduction
Patient satisfaction is an important aspect of health care that has received increasing attention as more reimbursement models move towards value-based care. In value-based models, a percentage of reimbursement is determined by the quality, rather than the quantity, of care, with “quality” measured in large part via patient satisfaction1–3. Measures of patient satisfaction have been used as a proxy for quality of care for decades, with research to suggest that higher satisfaction with medical care is associated with higher likelihood of following medical advice and of returning to the same provider for follow-up care4. In chronic illnesses, such as pain and diabetes, higher patient satisfaction has been associated with improved clinical outcomes5,6 Given its importance, there is a need to understand the factors associated with patient satisfaction, especially in chronic and difficult to treat conditions such as irritable bowel syndrome (IBS).
The literature evaluating patient satisfaction in gastroenterology has focused mainly on satisfaction after procedures7–13. Surprisingly, much less attention has been paid to patient satisfaction in chronic gastrointestinal disorders, such as IBS, for which treatment targets are based more on symptoms rather than objective outcomes. A baseline survey of participants prior to being randomized into a trial of cognitive behavioral therapy for IBS revealed that certain personality traits (i.e., low neuroticism), whether the patient had insurance coverage, and having previously consulted with a gastroenterologist were all positively associated with patient satisfaction14. However, there were several limitations to that study that decreased its generalizability to IBS patients. For example, patient satisfaction was measured using only a single-item with an unspecified recall time-frame, the population was part of a psychological research study, many (approximately 30%) had never seen a gastroenterologist, and clinical data (such as number of procedures) was not prospectively collected. In 2011, Dorn et al developed and validated an IBS-specific measure of patient satisfaction for use in clinical care15. The IBS satisfaction with care scale (IBS-SAT) evaluates domains of patient-physician relationship, health education, symptom-relief, office attributes, and access to healthcare. However, no study to date has used this validated questionnaire to explore the determinants of patient satisfaction with IBS care in a real-world setting.
The current prospective study aims to identify demographic, clinical, psychosocial and health-care utilization related predictors of patient satisfaction in a sample of IBS patients presenting to a tertiary care gastroenterology clinic using the IBS-SAT.
Materials and Methods
Patients
Consecutive new patients presenting to the outpatient Center for Functional Bowel Disorders and GI Motility at Beth Israel Deaconess Medical Center in Boston, Massachusetts between October 2017 and March 2019 completed an electronic symptom survey for clinical purposes before their initial visit and a sub-set consented to complete a follow-up research survey after 3–6 months. Data for the present study was used only from those who consented and completed the follow-up survey. Data was collected via Research Electronic Data Capture (REDCap), a HIPAA compliant, free, secure, web-based application. Ethics approval was obtained from the institutional review board.
Measures
Irritable Bowel Syndrome Severity Scoring System (IBS-SSS).
The IBS-SSS is a validated scale for assessing overall IBS symptom severity.16 It includes 5 questions of equal weight concerning symptoms over the past 10 days: average severity of abdominal pain, number of days with abdominal pain, average severity of abdominal distension or bloating, satisfaction with bowel habits, and the overall interference in their quality of life from these symptoms. All questions are scored on a 0–100 scale. The scores for all five questions are summed to a total IBS-SSS score between 0–500. Lower scores indicate lower symptom severity. A reduction in IBS-SSS score of ≥ 50 points is considered a clinically meaningful change.
Patient Reported Outcomes Measurement Information System (PROMIS) scales.
PROMIS is a National Institutes of Health (NIH) set of tools used to provide information on patient outcomes in a variety of fields. Patients completed the PROMIS Anxiety 7a, Depression 8a, and Sleep Disturbance 6a questionnaires before their initial visit and at 3–6 months17. The PROMIS Anxiety Scale 7a short form and PROMIS Depression Scale 8a short form consist of seven and eight questions, respectively, and each question has a 5-point Likert scale. The PROMIS Sleep Disturbance questionnaire consists of six questions with similar response options. For each PROMIS questionnaire, the total raw score was calculated by summing the response values to each question, which was then transformed to a standardized T-score distribution. This distribution has been established such that the mean value for the healthy US population is 50 and the standard deviation (SD) represents variation of 1018 Anxiety, depression and sleep disturbance were defined as a T-score ≥60.
Patient Satisfaction.
Patient satisfaction was assessed 3–6 months after the initial consultation using the irritable bowel syndrome satisfaction with care scale (IBS-SAT)15. IBS-SAT is a disease-specific, validated measure of patients’ satisfaction with IBS care. It comprises of 38 items assessing patient satisfaction with the following five subscales: connection with healthcare provider, education, benefits of visit, office attributes, and access to healthcare. The first item is a measure of overall satisfaction, asking “Overall, how satisfied are you with the care you most recently received for your IBS?” This was scored as 1=not at all, 2=a little bit, 3=a fair amount, 4=a great deal, and 5=completely. For the remaining 37 items, patient answered how strongly they agree or disagree with each item on a five point Likert scale: 1=strongly disagree, 2= disagree, 3=neither agree nor disagree, 4=agree or 5=strongly agree. The overall IBS-SAT score was calculated by calculating the mean score of the 37 individual items. Mean scores for each subscale were also calculated and ranged from 0–5 with higher scores suggesting higher satisfaction. Patients were considered satisfied for a subscale if the mean score for that subscale was greater than 3. If the mean score for subscale was ≤ 3, patient was considered not satisfied for that subscale.
Healthcare utilization and medical record review.
Patients were asked before their initial GI consultation at the BIDMC if they had previously seen a gastroenterologist for their symptoms. Online medical records were reviewed to extract the number of laboratory tests and diagnostic procedures (i.e., endoscopies, radiological investigations, breath tests, manometries) performed between the time of initial consultation and completion of follow-up survey (3–6 months). Medical records were also reviewed to collect the following data for each patient: total number of recommendations at initial visit (which included pharmacological and non-pharmacological therapies prescribed, referrals and lifestyle changes), number of over the counter and prescription medications tried during the follow-up period, number of phone calls to gastroenterologist, number of gastroenterology follow-up visits, number of referrals (physical therapy, nutrition, acupuncture etc.), gender of physician, and whether a gastroenterology fellow was involved in the initial consultation.
Statistical Analysis
Statistical analysis was performed used Stata 13.0 (StataCorp, College Station, USA). Mean and median were reported with standard deviation (SD) and range respectively.
To explore the predictors of patient satisfaction, a two-step linear regression process described below was used. The dependent variable was patient satisfaction, which was measured using the mean IBS-SAT score. Independent variables are listed in Table 2. Based on the results of unadjusted or univariable linear regression models (which studies the linear relationship between the dependent variable and single independent variable without adjusting for other variables), all variables with p<0.1 on unadjusted analyses were included in a multivariable linear regression model (which assessed the linear relationship between the dependent variable and multiple independent variables while adjusting for potential confounders) and retained in the model if still significant at this level. Those with P-value ≥ 0.1 in the unadjusted analyses were added back to the multivariable model one at a time. In the final model, we only retained variables that were significantly (p<0.05) associated with our outcome. The strength of relationship between dependent and independent variables is being reported using standardized beta coefficient (β) and p-value.
Table 2:
Factors associated with patient satisfaction on univariable analysis
| Standardized Beta coefficient | P-value | |
|---|---|---|
| Demographic characteristics | ||
| Mean age (SD) | −0.05 | 0.57 |
| Female gender | 0.04 | 0.64 |
| Clinical characteristics | ||
| IBS subtype | 0.03 | 0.73 |
| Mean IBS symptom severity | −0.13 | 0.13 |
| Change in IBS severity over 3 months | −0.29 | 0.001* |
| Baseline psycho-somatic characteristics | ||
| Baseline anxiety score | −0.16 | 0.07* |
| Baseline depression score | −0.24 | 0.005* |
| Baseline sleep disturbance score | −0.06 | 0.49 |
| Change in anxiety score | −0.12 | 0.18 |
| Change in depression score | −0.11 | 0.23 |
| Change in sleep score | −0.004 | 0.96 |
| Baseline Healthcare utilization | ||
| Prior gastroenterology consultation | −0.12 | 0.18 |
| Duration of symptoms | 0.10 | 0.26 |
| Healthcare utilization in three months | ||
| Serological or stool investigations performed | 0.10 | 0.24 |
| Number of diagnostic tests performed** | 0.28 | 0.001* |
| Number of medications tried for GI symptoms*** | 0.05 | 0.60 |
| Number of recommendations at initial visit**** | 0.19 | 0.03* |
| Number of phone calls | −0.11 | 0.20 |
| Number of gastroenterology follow-up visits | 0.20 | 0.02* |
| Number of services referred to by gastroenterologist | 0.11 | 0.19 |
| Physician characteristics | ||
| Patients evaluated by female physician | −0.05 | 0.59 |
| Patients evaluated by Fellows at first visit | −0.13 | 0.13 |
Factors with P-value less than 0.1 which were include in multivariable regression
Includes endoscopies, manometries, breath tests, and radiologic investigations
Includes over the counter as well as prescription
Includes pharmacological and non-pharmacological therapies, referrals, lifestyle changes
Results
A total of 395 patients (208 with Rome IV IBS) consented to complete the followup surveys and 228 (140 with IBS, 67% IBS response rate) returned the followup survey (58% overall response rate). IBS was diagnosed using Rome IV criteria by 8 gastroenterologists with expertise in managing functional gastrointestinal disorders. Online review of medical records (performed by PS) confirmed that respondents with IBS diagnoses were not found to have any organic cause for their symptoms during the follow-up period. Three IBS respondents did not complete the IBS-SAT. Therefore, 137 IBS patients were included in the current study.
Of the 137 IBS patients included, the mean age was 44.1 (± 17.1) years and the majority (78.1%) were women. More than one-third of patients had anxiety at baseline, one quarter had sleep disturbance, and one tenth had depression. More than three-fourths had previously seen a gastroenterologist for their symptoms. The majority (56%) reported having IBS symptoms for 10 years or longer. Other baseline clinical and psychosocial characteristics along with their health care utilization pattern are described in Table 1. During the duration of follow-up, the mean change in IBS severity score was −65.1 (± 108.6).
Table 1:
Baseline characteristics and healthcare utilization by patients with IBS
| Demographic characteristics | |
| Mean age (SD) | 44.1 (17.0) |
| Female gender | 107 (78.1%) |
| Clinical characteristics | N (%) |
| IBS subtype | |
| IBS-D | 38 (27.7) |
| IBS-C | 69 (50.4) |
| IBS-M | 30 (21.9) |
| Mean IBS symptom severity* | 266.1 (100.9) |
| Baseline characteristics** | N (%) |
| Anxiety | 48 (35) |
| Depression | 23 (16.8) |
| Sleep disturbance | 35 (25.6) |
| Prior gastroenterology consultation | 107 (78.1) |
| Duration of symptoms | |
| < 1 year | 16 (11.7) |
| 1–5 years | 27 (19.7) |
| 5–10 years | 17 (12.4) |
| >10 years | 77 (56.2) |
| Healthcare utilization in three months after initial consultation | |
| Serological or stool investigations performed | 76 (55.5) |
| Median number of diagnostic tests performed*** | 1 (0–4) |
| Median number of medications taking for their GI symptoms**** | 2 (0–10) |
| Median number of recommendations at initial visit***** | 4 (1–10) |
| Median number of phone calls | 0 (0–9) |
| Median number of follow-up visits | 1 (0–4) |
| Median number of services referred to | 0 (0–2) |
| Physician characteristics | |
| Patients evaluated by female physician | 101(73.7) |
| Patients evaluated by Fellows at first visit | 51 (37.2) |
Mean values are expressed with standard deviation (SD) and median values with range.
Measured using IBS-SSS
Defined by PROMIS T-score ≥60
Includes endoscopies, manometries, breath tests, and radiologic investigations
Includes over the counter as well as prescription
Includes pharmacological and non-pharmacological therapies, referrals, lifestyle changes
Patient Satisfaction
When asked about overall satisfaction with current IBS care, the majority of patients were either a great deal (34.9%) or completely satisfied (18.6%). Only 6.2% were not satisfied at all and 14.7% were a little bit satisfied (Figure 1). The mean overall IBS-SAT score was 3.8 ± 0.6. Among the five subscales of patient satisfaction, the highest proportion were satisfied with connection with the provider subscale (93.4%). The subscale of ‘benefits of the visit’ had the lowest satisfaction rate (70.8%) (Figure 2). The mean scores (SD) for five subscales were: connection with the provider (4.2 ± 0.7), education (3.7 ± 0.8), benefits of visit (3.6 ± 0.8), office attributes (3.6 ± 0.7), and access to healthcare (3.8 ± 0.7).
Figure 1:
Percentage of patients with varying degrees of overall patient satisfaction with the current IBS care
Figure 2.
Percentage of patients reporting satisfaction (and dissatisfaction) with various subdomains of IBS satisfaction with care scale (IBS-SAT)
Predictors of patient satisfaction.
Of the variables listed in Table 2, those with P value <0.1 on unadjusted analyses were included in the multivariable analysis. The factors which were positively associated with patient satisfaction on unadjusted analyses at the level of P<0.1 were-decrease in IBS severity from baseline, lower baseline depression severity, lower baseline anxiety severity, higher number of recommendations at initial gastroenterology visit, higher number of diagnostic procedures during the follow-up period and higher number of follow-up gastroenterology visits (Table 2).
In the final multivariable model (table 3), higher number of recommendations at initial visit (β=0.25, P=0.002), higher number of follow-up gastroenterology visits (β=0.15, P=0.04), and higher number of diagnostic tests during the follow-up period (β=0.28, P<0.001) were positively associated with higher patient satisfaction with IBS care. Higher baseline depression score (β= −0.25, P=0.001) and increase in IBS severity score from baseline (β= −0.26, P=0.001) were negatively associated with patient satisfaction at follow-up. The overall model predicted 30% of the variance in patient satisfaction (R-square= 0.299, p<0.001). For a multiple regression model with five independent variables (predictors), at a probability level of 0.05, a sample size of 137 had 94% power to detect a medium effect size (f2 =0.15).
Table 3:
Predictors of patient satisfaction on multivariable analysis
| Standardized Beta coefficient | P-value | |
|---|---|---|
| Change in IBS severity score from baseline | −0.26 | 0.001 |
| Baseline depression score | −0.25 | 0.001 |
| Total number of diagnostic tests during the follow-up period* | 0.28 | <0.001 |
| Total number of recommendations at initial gastroenterology visit** | 0.25 | 0.002 |
| Total number of gastroenterology follow-up visits | 0.15 | 0.04 |
Includes endoscopies, manometries, breath tests, and radiologic investigations
Includes pharmacological and non-pharmacological therapies, referrals, lifestyle changes
Discussion
We identified several salient predictors of satisfaction in patients with IBS 3–6 months after establishing medical care with a gastroenterologist. Decrease in IBS severity, higher number of diagnostic testing during the follow-up period, higher number of recommendations at the initial visit, higher number of follow-up visits, and lower depression score at initial visit were predictive of greater patient satisfaction at follow-up.
Symptom improvement is the primary goal of most consultations for IBS and, therefore, it is not surprising that a decrease in IBS severity 3–6 months after the initial consultation predicted higher patient satisfaction with medical care. It is interesting to note, however, that the severity of IBS symptoms at the initial consultation did not predict treatment satisfaction. Clinically, this suggests that patients with severe IBS symptoms were as likely to be satisfied with their care as those with mild or moderate symptoms, particularly if they had improvement in their symptoms. This is consistent with previous research indicating that symptom severity is not significantly associated with patient satisfaction in IBS14 or celiac disease19. To our knowledge, this is the first time that change in IBS symptom severity has been associated with higher patient satisfaction scores.
Unfortunately, complete symptom relief is difficult to achieve in patients with IBS, particularly those in a tertiary care center, the majority of whom had seen a gastroenterologist previously and had symptoms for over 10 years. Thus, it is not surprising that among the various domains included in the IBS-SAT, the subdomain of ‘benefits of visit’ had the lowest satisfaction rate (70.8%). This domain includes assessment of symptom relief, better sense of control over symptoms, expectations of care and treatment by trial and error. Lower satisfaction in this domain could be due to several modifiable or non-modifiable factors such as lack of symptomatic improvement with pharmacological or non-pharmacological therapy tried, high expectation in this patient population visiting a tertiary referral center, or lack of individualized approach in IBS where therapeutic options are often not targeted towards underlying pathophysiology. This also highlights the need for personalized, safe and effective pharmacological options to manage IBS related symptoms.
Higher depression scores at initial consultation was associated with lower satisfaction at follow-up. Depression has also been identified as a predictor of poorer patient satisfaction in primary care20 and chronic pain21,22. Given the high comorbidity of both depression and anxiety in IBS23,24, this finding highlights the importance of screening IBS patients for low mood and anxiety and for physicians to be prepared to discuss these issues with their patients. To this end, it is ideal to have referral resources for both general mental health (to treat anxiety and depression) as well as for health psychology (for the treatment of illness-specific issues).
We also found that the number of recommendations at initial visit was associated with higher patient satisfaction 3–6 months after initial consultation. The number of recommendations included pharmacological and non-pharmacological therapies prescribed, referrals, and lifestyle changes. Therefore, a multipronged approach in managing IBS symptoms might provide patients with a hope for improvement and better sense of control over their symptoms which in turn may be associated with higher patient satisfaction.
Finally, the number follow up visits and diagnostic tests were both associated with higher patient satisfaction at follow-up. These findings are consistent with previous studies suggesting that patient satisfaction in IBS and other chronic gastrointestinal diseases may be associated with access to diagnostic tests 14,15. However, these findings must be interpreted with caution for several reasons. First, statistical significance was achieved based on a small number of tests ordered at the initial visit, and it is not yet clear whether this bears clinical significance in terms of long-term patient satisfaction. Secondly, this finding raises important ethical concerns about measuring quality of care based on patient preferences, as such a model might incentivize physicians to move away from evidence-based care (e.g. using symptom-based diagnostic criteria for IBS) in order to improve patient satisfaction25. With this in mind, future quantitative or qualitative research studies might focus on elucidating what patients with chronic and/or functional diagnoses may be seeking from medical consultation, such as reassurance to ease health anxieties, in addition to relief from symptoms. Indeed, reassurance (provided by frequent visits and/or a strong patient-provider relationship) may be an important underlying factor determining the patient satisfaction.
This study has several strengths including its prospective design, use of a validated and multi-dimensional measure of patient satisfaction, and inclusion of patients in a real-world clinical setting. Despite these strengths, however, there are several limitations to consider. First, our patients were completing a measure of patient satisfaction 3–6 months after their initial visit with the gastroenterologist. Although they were informed that their individual responses would not be shared with their treatment team, their responses may have been inflated. Second, our treatment team is comprised of gastroenterologists who specialize in the treatment of functional gastrointestinal disorders and, therefore, may not be representative of the majority of physicians treating IBS in the community. Third, this study was not powered to adjust for provider differences. Fourth, there may have been differences between the 68 patients who did not complete the followup survey and the 140 who did complete the followup. Unfortunately, our database did not include information from the 68 who did not return completed followup surveys. Fifth, the validation study for the IBS-SAT did not include test-retest reliability. As a result, it may not be valid to evaluate IBS-SAT several months after a clinic visit. Finally, some of the variables in this analyses were based on chart review, which can potentially introduce error in data collection (e.g. missed information if certain variables were not included in the medical chart or were overlooked due to human error).
In conclusion, patient satisfaction is an important, but largely overlooked, component of the treatment and management of chronic, functional gastrointestinal disorders. This paper highlights data from a prospective study evaluating predictors of patient satisfaction in a tertiary care clinic. The main predictors of patient satisfaction 3–6 months after establishing care with a gastroenterologist include improvement in symptom severity, lower depression score at initial visit, higher number of recommendations at initial visit, and higher number of follow-up visits.
Background:
Patient satisfaction is an important but overlooked component of management of irritable bowel syndrome (IBS). It is not clear what factors are associated with patient satisfaction with their care.
Findings:
In a survey of 137 patients with IBS, factors associated with satisfaction 3–6 months after establishing care with a gastroenterologist include reduced severity of IBS, lower depression score at initial visit, and more gastroenterologist recommendations and follow-up visits.
Implications for patient care:
These factors can be used to improve management of patients with IBS.
Acknowledgments
Grant support: This project was funded in part by RO1 AT008573-03 (AL) and T32DK007760 (PS, SB)
Footnotes
Conflicts of interests: None
Disclosures: AL worked as consultant for Salix, Takeda, Ironwood, and Allergen.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Boyer L, Francois P, Doutre E, et al. Perception and use of the results of patient satisfaction surveys by care providers in a French teaching hospital. Int J Qual Health Care 2006;18:359–364. [DOI] [PubMed] [Google Scholar]
- 2.Schoenfelder T, Klewer J, Kugler J. Determinants of patient satisfaction: a study among 39 hospitals in an in-patient setting in Germany. Int J Qual Health Care 2011;23:503–509. [DOI] [PubMed] [Google Scholar]
- 3.Jenkinson C, Coulter A, Bruster S. The Picker Patient Experience Questionnaire: development and validation using data from in-patient surveys in five countries. Int J Qual Health Care 2002;14:353–358. [DOI] [PubMed] [Google Scholar]
- 4.Larsson G, Wilde-Larsson B. Quality of care and patient satisfaction: a new theoretical and methodological approach. Int J Health Care Qual Assur 2010;23:228–247. [DOI] [PubMed] [Google Scholar]
- 5.Alazri MH, Neal RD. The association between satisfaction with services provided in primary care and outcomes in Type 2 diabetes mellitus. Diabet Med 2003;20:486–490. [DOI] [PubMed] [Google Scholar]
- 6.Hirsh AT, Atchison JW, Berger JJ, et al. Patient satisfaction with treatment for chronic pain: predictors and relationship to compliance. Clin J Pain 2005;21:302–310. [DOI] [PubMed] [Google Scholar]
- 7.Woodham BL, Meng R, Roberts RH. A Novel, Dynamic Statistical Model for Predicting Patient Satisfaction with Fundoplication Based on Pre-Operative Symptom Patterns. World J Surg 2017;41:2778–2787. [DOI] [PubMed] [Google Scholar]
- 8.Courtney MJ, Rao M, Teasdale R, et al. Would you have laparoscopic Nissen fundoplication again? A patient satisfaction survey in a UK population. Frontline Gastroenterol 2014;5:272–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qureshi MO, Shafqat F, Ahmed S, et al. Factors affecting patient satisfaction during endoscopic procedures. J Coll Physicians Surg Pak 2013;23:775–779. [PubMed] [Google Scholar]
- 10.van Putten PG, Ter Borg F, Adang RPR, et al. Nurse endoscopists perform colonoscopies according to the international standard and with high patient satisfaction. Endoscopy 2012;44:1127–1132. [DOI] [PubMed] [Google Scholar]
- 11.Iravani S, Frootan M, Zojaji H, et al. Effect of general anesthesia during GI endoscopic procedures on patient satisfaction. Gastroenterol Hepatol Bed Bench 2012;5:S20–25. [PMC free article] [PubMed] [Google Scholar]
- 12.Lin OS, Kozarek RA, Arai A, et al. The effect of periodic monitoring and feedback on screening colonoscopy withdrawal times, polyp detection rates, and patient satisfaction scores. Gastrointest Endosc 2010;71:1253–1259. [DOI] [PubMed] [Google Scholar]
- 13.Yanai H, Schushan-Eisen I, Neuman S, et al. Patient satisfaction with endoscopy measurement and assessment. Dig Dis 2008;26:75–79. [DOI] [PubMed] [Google Scholar]
- 14.Quigley BM, Sova CC, Brenner DM, et al. (Can’t Get No) Patient Satisfaction: The Predictive Power of Demographic, GI, and Psychological Factors in IBS Patients. J Clin Gastroenterol 2018;52:614–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dorn SD, Morris CB, Schneck SE, et al. Development and validation of the irritable bowel syndrome satisfaction with care scale. Clin Gastroenterol Hepatol 2011;9:1065–1071.e1–2. [DOI] [PubMed] [Google Scholar]
- 16.Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther 1997;11:395–402. [DOI] [PubMed] [Google Scholar]
- 17.List of Adult Measures. http://www.healthmeasures.net/explore-measurement-systems/promis/intro-to-promis/list-of-adult-measures Accessed August 20, 2018.
- 18.PROMIS. http://www.healthmeasures.net/score-and-interpret/interpret-scores/promis Accessed August 20, 2018.
- 19.Faye AS, Mahadev S, Lebwohl B, et al. Determinants of Patient Satisfaction in Celiac Disease Care. J Clin Gastroenterol 2018;52:30–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kavalnienė R, Deksnyte A, Kasiulevičius V, et al. Patient satisfaction with primary healthcare services: are there any links with patients’ symptoms of anxiety and depression? BMC Fam Pract 2018;19:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Riley JL, Myers CD, Robinson ME, et al. Factors predicting orofacial pain patient satisfaction with improvement. J Orofac Pain 2001;15:29–35. [PubMed] [Google Scholar]
- 22.Henschke N, Wouda L, Maher CG, et al. Determinants of patient satisfaction 1 year after presenting to primary care with acute low back pain. Clin J Pain 2013;29:512–517. [DOI] [PubMed] [Google Scholar]
- 23.Vandvik PO, Wilhelmsen I, Ihlebaek C, et al. Comorbidity of irritable bowel syndrome in general practice: a striking feature with clinical implications. Aliment Pharmacol Ther 2004;20:1195–1203. [DOI] [PubMed] [Google Scholar]
- 24.Mikocka-Walus A, Turnbull D, Moulding N, et al. Psychological comorbidity and complexity of gastrointestinal symptoms in clinically diagnosed irritable bowel syndrome patients. J Gastroenterol Hepatol 2008;23:1137–1143. [DOI] [PubMed] [Google Scholar]
- 25.Fenton JJ, Jerant AF, Bertakis KD, et al. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med 2012;172:405–411. [DOI] [PubMed] [Google Scholar]