Sir,
Erythromelanosis Follicularis Faciei et Colli (EFFC) and Erythroses Pigmentosa Mediofacialis (EPM) are considered to be the disorders of abnormal follicular keratinization characterized by a triad of hyperpigmentation, erythema, and keratotic follicular papules. Herein, we report a young female with a features of both in association with generalized keratosis pilaris which is a rare co-occurrence, diagnosis of which was confirmed by dermoscopy and histopathology.
A 16-year-old female reported with multiple asymptomatic elevated lesions associated with darkening of skin which appeared first over the sides of cheeks, upper part of ear and gradually extended over the neck since 4 years. Similar lesions were also seen over central part of face since 2 years. Patient denied history of topical application and photosensitivity. Her past, personal, and family history was insignificant. Cutaneous examination revealed bilaterally symmetrical follicular micropapules associated with well-demarcated erythema and hyperpigmentation over the pre-auricular region, pinnae of ear and neck [Figure 1a and b]. Forehead, perinasal, peribuccal region, and chin also showed lesions of similar morphology [Figure 2]. In addition, patient had keratotic papules over bilateral extremities, back, chest, abdomen, and thighs suggestive of generalized keratosis pilaris [Figure 3a-d]. On diascopy of facial lesion erythema disappeared but pigmentation persisted. Dermoscopy using 3 Gen Dermlite DL4 (CA, USA) 10 × polarized mode, from cheeks revealed multiple small whitish rounds with keratotic follicular plugs surrounded by gray spots in a background of brownish discoloration suggestive of EFFC [Figure 4a]. Forehead lesion on dermoscopy showed numerous dilated follicles with keratotic plugging, perifollicular erythema, and scaling suggestive of EPM [Figure 4b]. Dermoscopy of the lesion from upper arm showed coiled hair, keratotic plugs, perifollicular erythema, and scaling suggestive of keratosis pilaris [Figure 4c]. Skin biopsy (one from cheek and another from forehead) with H and E staining revealed follicular hyperkeratosis with acanthosis with increased pigmentation in the basal layer. Dermis showed superficial perivascular lymphocytic infiltrate [Figure 5a and b]. Based on clinical, dermoscopy and histopathology a final diagnosis of coexistent EFFC and EPM in a patient of generalized keratosis pilaris was made. The patient was counselled and started on topical tretinoin 0.025% cream and sunscreen for face and an emollient for the body. After 8 weeks of treatment patient showed only mild improvement and is under regular follow-up.
Figure 1.

(a and b) Bilaterally symmetrical follicular papules, erythema, and hyperpigmentation over pre-auricular region extending over pinnae and neck
Figure 2.

Erythema, hyperpigmentation, and follicular papules over forehead, perioral region and chin
Figure 3.

(a-d) Lesions of keratosis pilaris symmetrically present over arms, back, chest and abdomen, thighs, and legs, respectively
Figure 4.
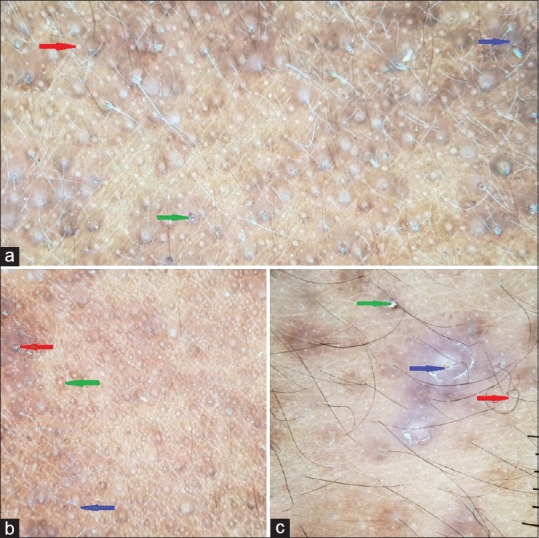
(a) Dermoscopy of EFFC revealed multiple small whitish rounds (Red arrow) with keratotic follicular plugs (Green arrow) surrounded by grey spots in a background of red-brown discolouration (Blue arrow) (b) Dermoscopy of EPM showed numerous dilated follicles (Red arrow), keratotic plugging (Green arrow) with perifollicular erythema and scaling (Blue arrow). (c) Dermoscopy of the lesion from upper arm showed coiling of hair shaft (Red arrow) with keratotic plugs (Green arrow) surrounded by perifollicular erythema and scaling (Blue arrow). (polarized; original magnification: 10X.)
Figure 5.
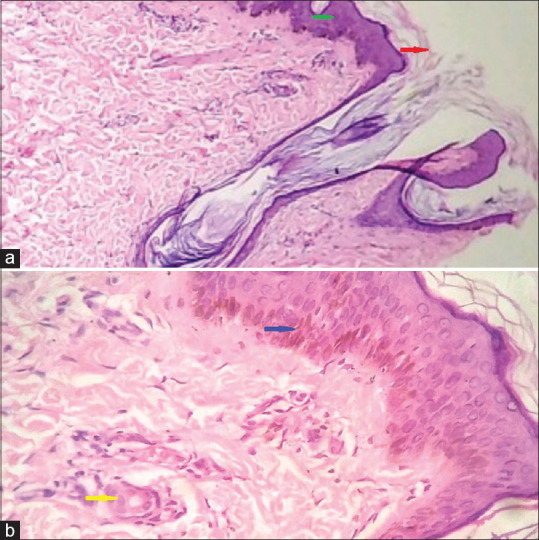
(a) Scanner view, showing follicular hyperkeratosis (Red arrow), acanthosis (Green arrow) (H and E, 10X). (b) Dermis showing increased pigmentation of basal cell layer (Blue arrow), mild perivascular lymphocytic infiltrate (yellow arrow) (H and E 40X)
EFFC is an unfamiliar syndrome described by Kitamura, in 1960, with well-demarcated erythema, telangiectasia, hyperpigmentation, and follicular papules primarily on lateral aspect of the face, with an extension on to the lateral half of the neck, thus the name et colli (in Latin”et”=”and”,”colli”=”neck”). It affects patients of all ethnic group but majorly seen in Asian or Middle Eastern men.[1] The male to female ratio is observed to be 2:1.[2] However, it is increasingly reported in female patients as noticed in our case.[3] EPM as described by Brocq, is erythematous to hyperpigmented, rough skin over midline of the face. It is synonymously called as erythrose pigmentaire faciale, dermatose pigmentée médiofaciale, erythrosis pigmentosa peribuccalis, erythrosis pigmentata faciei, erythromelanosis follicularis faciei and erythrosis pigmentosa faciei colli.[4] The etiology of EFFC is multifactorial and includes genetic (autosomal recessive) and hereditary components.[5] Previous data suggest spontaneous mutation in EFFC.[6] Tuzun and Wolf et al. postulated that EFFC to be a chromosomal instability syndrome.[7] It is hypothesized that various environmental factors such as cosmetics, ultraviolet radiation, and topical formulations can cause hyperpigmentation over the period of years. Dermoscopy of EFFC shows multiple round whitish areas with follicular plugs, some shows central hair, surrounded by blue gray spots or peppering in a reddish-brown background.[8] Dermoscopy of EPM includes follicular dilatation with yellowish keratotic plugs, perifollicular erythema, and scaling surrounded by slate-gray globules.[9] Histology of EFFC and EPM is similar and shows follicular hyperkeratosis, increased basal layer pigmentation, and incontinence of melanin pigment with dermal melanophages. Dermis shows perivascular and periadnexal lymphocytic infiltrate with vasodilatation.[8] EFFC has been found to be associated with keratosis pilaris of different body parts which postulated that EFFC is a variant of keratosis pilaris.[3,4,6,7,10,11] Juhlin et al. has reported a single case of EFFC and EPM occurring in a 34-year-old female postulating that the two conditions are same.[12] Our case is unique since she had concurrent EFFC, EPM, and generalized KP. It can be stated that both EFFC and EPM are etiologically same conditions manifesting at different sites. Dermoscopy plays an important beside tool to identify these entities. Differential diagnosis of EFFC and EPM includes ulerythema ophryogenes, atrophoderma vermiculatum, Riehl's melanosis, poikiloderma of Civatte, tricostasis spinulosa, lichen spinulosus [Table 1]. Treatment of EFFC and EPM is same but unsatisfactory. Various topical keratolytics such as tretinoin, glycolic acid, salicylic acid (20–30%), urea, ammonium lactate, vitamin C can be used assuming it to be a disorder of keratinization. Oral isotretinoin (0.1–1 mg/kg/d) can be tried for extensive involvement. Topical tacalcitol ointment was found to be a successful therapeutic option for EFFC in recent years.[13] Multiple sessions of long-pulsed dye laser for erythema and Q-switched Nd: YAG laser (1,064 nm) for hyperpigmentation are mentioned in the treatment of EFFC by Li et al.[14] EFFC and EPM are underreported disorders which can be easily diagnosed with the help of a dermoscope. Also, it is the rarity of EFFC and EPM associated with generalized KP which prompted us to report this case.
Table 1.
Differential diagnosis of erythrosis pigmentosa mediofacialis and erythromelanosis follicularis faciei et colli
| Diagnosis | Site | Clinical Features | Histopathology | Dermoscopy |
|---|---|---|---|---|
| 1) Keratosis pilaris[15] | Extensor aspect of extremity, thigh, buttock, sometimes generalised. | Multiple gray-white tiny keratotic plugs on follicular opening, antenna sign positive, hair entrapment seen. | Basket weave and lamellated orthokeratosis, follicular infundibular dilatation and plugging with focal peri-infundibular parakeratosis, perifollicular lymphocytic infiltrate | Coiled vellus hairs sometimes semi-circular, or looped, peri-follicular erythema and peri-pilar casts. Hairs emerging in groups of 2 or 3. Vascular ectasias |
| 2) Keratosis pilaris atrophicans faciei (ulerythema ophrayogens)[16] | Face especially eyebrows, cheeks | Same as KP but associated with prominent atrophy and alopecia. Eyebrows involvement known as ulerythema ophryogenes, lesion starts in the lateral part of eyebrows progresses medially to involve rest of eyebrow and cheeks | Follicular atrophy with perifollicular fibrosis, hyperkeratotic plugging of follicular openings and mild perivascular and perifollicular lymphocytic infiltrate | Background erythema with some scattered fine linear vessels and yellow-white dots in the follicular openings, surrounded by brown circles of perifollicular hyperpigmentation |
| 3) Keratosis rubra pilaris[17] | Cheeks, eyebrows | Similar findings of KP with marked erythema | Similar findings of KP with more dilated capillaries | Irregularly coiled vellus hairs embedded into the horny layer with perifollicular erythema and underlying vascular ectasia |
| 4) Atrophoderma vermiculatum[17] | Cheeks | Bilaterally symmetrical erythematous follicular papules on cheeks in child, resulting in honeycomb atrophy | Epidermal atrophy, mild perifollicular inflammation, decrease number of follicles which are widely dilated either empty or contained keratinous materials. Dermal atrophy with disappearance of elastic fibers. | Reticulated depressions with narrow ridges of normal appearing skin giving worm-eaten appearance |
| 5) Poikiloderma of Civate[18,19] | Lateral aspect neck | Triad of reticulate hyper-pigmentation, atrophy, and telangiectasia. Telangiectasias are interfollicular with sparing of thin rim of skin around each hair follicle | Epidermal, papillary dermal atrophy with loss of papillae, hyaline masses at the dermoepidermal junction and disappearance of the elastic network in the upper dermis. In fully developed lesions cavities in the connective tissue filled with epidermal cells, pigment and lymphocytes may be seen. | Dotted/globular vessels and linear irregular vessels, giving rise to a “spaghetti and meatballs” appearance along with perifollicular whitish areas. Additional findings include follicular keratotic plugs and delicate reticular or structureless brownish areas. |
| 6) Lichen spinulosus[17] | Extensor aspects of extremities, neck, abdomen, thigh, buttocks, popliteal fossa | Multiple grouped follicular papules with projecting keratin spine without erythema | Follicular hyperkeratosis and keratotic plugging of infundibulum with perifollicular and perivascular mononuclear infiltrate | Follicular papules with translucent spines |
| 7) Riehl’s melanosis[20] | Cheeks, temporal area, forehead | Patches of hyperpigmentation over these areas, sometimes associated with pruritus, prolong use of cosmeceuticals can be elicited | Dilated infundibulum with inflammatory cell infiltrate, liquefaction of basal cells, pigment incontinence, dilated vessels with perivascular inflammatory infiltration. | Sparse scaling, pseudonetwork, grey dots/granules, follicular keratotic plugs, perifollicular whitish halo, telangiectatic vessels |
| 8) Trichostasis spinulosa[17] | Nose, abdomen, back, rarely diffuse | Multiple tiny black dots on face especially over tips of nose, black dots represent vellus hair, without erythema | Follicular hyperkeratosis, Dilated infundibulum with numerous pigmented vellus hairs and keratin material | Tuft of short vellus hairs emerging from the same follicular opening. Keratotic plugs within dilated follicle |
| 9) Comedonal acne[21] | Cheeks, forehead, neck, chest, back | Tiny papules sometimes black (open comedons) containing cellular debris and sometimes white (closed comedons) with intact overlying epithelium | Epidermis shows follicular dilatation with keratinous material, mild perivascular lymphocytic infiltrate in dermis | Numerous homogenous areas, light & dark-brown sometimes black in color depending on the type of acne open or closed comedones, predominantly circular and situated superficially. |
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Judge MR, McLean WH, Munro CS. Disorders of keratinization. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8th ed. Vol. 1. UK: Wiley-Blackwell; 2010. pp. 1972–3. [Google Scholar]
- 2.Al Hawsawi K, Aljuhani O, Niaz G, Fallatah H, Alhawsawi A. Erythromelanosis follicularis faciei: A case report and review of the literature. Case Rep Dermatol. 2015;7:335–9. doi: 10.1159/000442343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Augustine M, Jayaseelan E. Erythromelanosis follicularis faciei et colli: Relationship with keratosis pilaris. Indian J Dermatol Venereol Leprol. 2008;74:47–9. doi: 10.4103/0378-6323.38409. [DOI] [PubMed] [Google Scholar]
- 4.Kalwaniya S, Morgaonkar M, Gupta S, Jain SK. Co-occurrence of erythrosis pigmentosa mediofacialis and erythromelanosis follicularis faciei et colli associated with keratosis pilaris in an adolescent female. Indian J Dermatol. 2016;61:467. doi: 10.4103/0019-5154.185747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yanez S, Velasco JA, Gonzalez MP. Familial erythromelanosis follicularis faciei et colli-an autosomal recessive mode of inheritance. Clin Exp Dermatol. 1993;18:283–5. doi: 10.1111/j.1365-2230.1993.tb02190.x. [DOI] [PubMed] [Google Scholar]
- 6.Arif T. Generalized keratosis pilaris associated with erythromelanosis follicularis faciei et colli: A rare coexistence. Indian J Paediatr Dermatol. 2015;16:149–51. [Google Scholar]
- 7.Tüzün Y, Wolf R, Tüzün B, Ozdemir M, Demirkesen C, Deviren A, et al. Familial erythromelanosis follicularis and chromosomal instability. J Eur Acad Dermatol Venereol. 2001;15:150–2. doi: 10.1046/j.1468-3083.2001.00148.x. [DOI] [PubMed] [Google Scholar]
- 8.Maouni S, El Anzi O, Sqalli A, Znati K, Meziane M, Hassam B. Erythromelanosis follicularis faciei et colli: Dermoscopy and dermatopathology correlates. JAAD Case Rep. 2019;5:535–6. doi: 10.1016/j.jdcr.2019.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luna PC, Abad ME, González VM, Vigovich F, Casas JG, Larralde M, et al. Erythrosis pigmentosa peribuccalis in an adolescent: Dermoscopic description and management. Pediatr Dermatol. 2016;33:e65–8. doi: 10.1111/pde.12756. [DOI] [PubMed] [Google Scholar]
- 10.Ermertcan AT, Oztürkcan S, Sahin MT, Türkdogan P, Saçar T. Erythromelanosis follicularis faciei et colli associated with keratosis pilaris in two brothers. Pediatr Dermatol. 2006;23:31–4. doi: 10.1111/j.1525-1470.2006.00166.x. [DOI] [PubMed] [Google Scholar]
- 11.Elghblawi E. Erythromelanosis follicularis faciei et colli: A first female case report from the outskirts of Libya and literature review. Indian J Paediatr Dermatol. 2017;18:53–9. [Google Scholar]
- 12.Juhlin L, Alkemade H. Erythrosis pigmentosa mediofacialis (Brocq) and erythromelanosis follicularis faciei et colli in the same patient. Acta Derm Venereol. 1999;79:65–6. doi: 10.1080/000155599750011741. [DOI] [PubMed] [Google Scholar]
- 13.Kim WJ, Song M, Ko HC, Kim BS, Kim MB. Topical tacalcitol ointment can be a good therapeutic choice in erythromelanosis follicularis faciei et colli. J Am Acad Dermatol. 2012;67:320–1. doi: 10.1016/j.jaad.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 14.Li YH, Zhu X, Chen JZ, Wu Y, Wei HC, Gao XH, et al. Treatment of erythromelanosis follicularis faciei et colli using a dualwavelength laser system: A splitface treatment. Dermatol Surg. 2010;36:1344–7. doi: 10.1111/j.1524-4725.2010.01637.x. [DOI] [PubMed] [Google Scholar]
- 15.Sonthalia S, Bhatia J, Thomas M. Dermoscopy of keratosis pilaris. Indian Dermatol Online J. 2019;10:613–4. doi: 10.4103/idoj.IDOJ_279_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Coelho De Sousa V, Pinheiro R, Cunha N, Lencastre A, Cabete J. And next…Adnexa: Ulerythema ophryogenes and keratosis pilaris. Eur J Dermatol. 2018 Aug 1;28(4):566–7. doi: 10.1684/ejd.2018.3385. [DOI] [PubMed] [Google Scholar]
- 17.Panchaprateep R, Tanus A, Tosti A. Clinical, dermoscopic, and histopathologic features of body hair disorders. J Am Acad Dermatol. 2015 May;72(5):890–900. doi: 10.1016/j.jaad.2015.01.024. [DOI] [PubMed] [Google Scholar]
- 18.Katoulis AC, Stavrianeas NG, Panayiotides JG, Bozi E, Vamvasakis E, Kalogeromitros D, Georgala S. Poikiloderma of Civatte: a histopathological and ultrastructural study. Dermatology. 2007;214(2):177–82. doi: 10.1159/000098580. [DOI] [PubMed] [Google Scholar]
- 19.Errichetti E, Stinco G. Dermoscopy in Facilitating the Recognition of Poikiloderma of Civatte. Dermatol Surg. 2018 Mar;44(3):446–7. doi: 10.1097/DSS.0000000000001222. [DOI] [PubMed] [Google Scholar]
- 20.Wang L, Xu AE. Four views of Riehl's melanosis: clinical appearance, dermoscopy, confocal microscopy and histopathology. J Eur Acad Dermatol Venereol. 2014 Sep;28(9):1199–206. doi: 10.1111/jdv.12264. [DOI] [PubMed] [Google Scholar]
- 21.Vora RV, Kota RS, Sheth NK. Dermoscopy of nevus comedonicus. Indian Dermatol Online J. 2017;8:388–9. doi: 10.4103/idoj.IDOJ_430_16. [DOI] [PMC free article] [PubMed] [Google Scholar]


