Summary
The gold standard of treatment for major burns is early burn excision and autografting. In major burns this is complicated by a lack of donor site availability. Another challenge after burn injury is achieving optimal cosmetic and functional outcomes. Dermal regeneration templates (DRT) are biomatrices that help to address these problems. Within our centre the most commonly used are two-stage Integra® and single-stage Matriderm®. We review the use and outcomes of DRT in primary burns reconstruction within our regional burns centre. All patients undergoing primary burn reconstruction using Integra® (n=59) or Matriderm® (n=35) over a 13-year period were included. Integra® was used in patients with significantly larger burns (20.4% TBSA vs 1.7% TBSA). Comparable levels of graft take were seen in both groups. Major infections were significantly higher in the Integra® group (11/35 compared to 3/59). There was no significant difference in haematoma development, hypertrophic scarring or the need for secondary reconstructive surgery. Burn contractures developed in 15 patients treated with Matriderm® and 21 with Integra®. DRT have been used safely and effectively and have played an increasingly important role in our service over the last 13 years. Integra® is used primarily in large burns with limited donor sites and Matriderm® in smaller burns in cosmetically sensitive areas.
Keywords: dermal regeneration templates, dermal substitutes, Matriderm, Integra, major burns
Abstract
Le traitement de référence des brûlures graves est l’excision précoce et la greffe autologue. Dans ces brûlures graves, ce traitement peut s’avérer difficile par le manque de disponibilité de sites donneurs. De plus, l’obtention de résultats satisfaisants tant sur le plan cosmétique que fonctionnel est un véritable challenge dans les suites de brûlures. Les matrices dermiques (DRT) sont des biomatériaux qui peuvent aider à résoudre ces problèmes. Dans notre centre, les matrices le plus souvent utilisées sont Integra® double couche et Matriderm ®. Nous avons étudié l’utilisation des matrices dermiques et leurs résultats dans la chirurgie primaire des brûlures dans notre centre de traitement des brûlures de province. Tous les patients ayant bénéficié d’une chirurgie primaire pour brûlure par Integra® (n=59) et par Matriderm® (n=35) dans les 13 dernières années ont été inclus. Integra® a été utilisé pour des patients présentant des brûlures significativement plus étendues (20,4% TBSA vs 1,7% TBSA). Le taux de prise des greffes est comparable dans les deux groupes. Les infections sévères sont plus élevées de façon significative dans le groupe traité par Integra® (11/59 contre 3/35). Il n’y a pas de différence significative en ce qui concerne les hématomes, l’évolution hypertrophique des cicatrices ou la nécessité de chirurgie secondaire. Des rétractions cicatricielles sont apparues chez 15 patients traités par Matriderm® et chez 21 patients traités par Integra®. L’utilisation des matrices dermiques nous semble sûre et utile et a été largement développée ces 13 dernières années dans notre centre. Integra® est utilisé en chirurgie primaire pour les brûlures très étendues où les sites donneurs font défaut alors que Matriderm® est utilisé pour les brûlures de petite surface à enjeu fonctionnel et cosmétique.
Introduction
In the acute period following a significant burn injury the gold standard of treatment is early burn excision and reconstruction with split thickness autograft (SSG). Burn excision with adequate early wound cover is a critical step in modulating the body’s hypermetabolic and physiological response to burn injury and reducing the risk of bacterial invasion. 1 In patients with burns affecting over 50% of their total body surface area (TBSA), there is insufficient donor skin to allow immediate autografting. 2 The development of dermal regeneration templates (DRT) offers a potential solution. These are biomatrices which provide a permanent “off the shelf” method of wound cover at the time of burn excision by replacing the lost dermal cutaneous layer and acting as a scaffold for revascularisation and collagen formation to optimise wound healing. SSG are applied either at the time of DRT application or at a later date following revascularisation.
Another important consideration, particularly in burns affecting the hands, face and joints, is patients’ long-term functional and aesthetic outcome. Up to 90% of major burns involve the hands,3 and when affected even small burns can result in significant disability. For example, full thickness burns exposing tendons are considered “ungraftable” due to poor graft take and the functional limitations caused by adhesions. DRTs provide an interface allowing grafting over tendons while also aiming to optimise wound healing1 and scar quality in aesthetically important areas, reducing the need for delayed reconstruction.
Integra (Integra Life Science Corporation, Plainsboro, NJ, USA), is the most widely use DRT.4 Its traditional form is as a 1.3mm thick bilaminar sheet consisting of a cross linked bovine derived collagen with shark derived chondroitin-6-sulfate glycosaminoglycan dermal matrix and a temporary silicone epidermal layer.5 Traditionally, Integra and SSG application has been a two-stage process. Following burn excision, the dermal matrix with the overlying silicone epidermal layer is applied. Over the following weeks, the collagen within the dermal layer provides a scaffold for fibroblast, lymphocyte and macrophage infiltration. This leads to the formation of a “neodermis”.5 The presence of glycosaminoglycans within the dermal matrix reduces collagen breakdown by collagenases. Following formation of the neodermis, a second stage procedure is performed in which the silicone epidermal layer is removed and a thin SSG applied,5 reducing donor site morbidity.
Matriderm (Dr. Otto Suwelack Skin & Health Care AG, Billerbeck, Germany) is a 1mm acellular DRT comprised of a Type I, III, V collagen and elastin scaffold.6 The collagen within the matrix promotes cell migration, proliferation and revascularisation while the elastin component aims to improve the elasticity of regenerated tissue by promoting early angiogenesis and elastin synthesis.6Matriderm® is a single layer product, lacking the epidermal layer seen in Integra , and therefore autografting is required at the time of application. Integra® has released a one-stage product, however it is not routinely used in our unit.
Dermal regeneration templates are playing an increasingly important role in acute burn reconstruction, however there is a lack of evidence on their long-term outcomes. We aimed to review the use, outcomes and complications of DRT within our regional burn centre.
Materials and methods
We identified patients who had undergone primary reconstruction following burn injury using a DRT between January 2003 and December 2016 using our burns database (International Burn Injury Database). Data were collected retrospectively from all available patient notes and operative records. Exclusion criteria included: absence of operative notes and DRT used only for secondary burn reconstruction.
Data collected included: patient demographics, mechanism, depth and percentage TBSA of burn, Baux score, presence of inhalational injury, need for escharotomies, surgeries performed, complications and the need for secondary reconstructive surgeries. Early complications measured were: infection, DRT and SSG loss. Late complications measured were: hypertrophic scarring, contracture and need for secondary reconstructive procedures.
General care and protocols
Patients with major burns are assessed by the MDT on arrival. Burns are cleaned, prepped twice with aqueous betadine and debrided. Escharotomies are performed if required. Typically dressings are Jelonet® (Smith & Nephew), betadine soaked gauze and absorbent dressings secured with crepe. Depending on burn severity, patients are taken to the burns ward or the burn intensive care unit. As soon as stable, patients are taken to theatre for burn excision.
Surgical technique – Integra
Integra application occurred 48 hours after primary burn excision if “second look” surgery confirmed completeness of burn excision and no further wound extension. Following anaesthesia and positioning, patients were cleaned and double prepped with aqueous betadine. Tissue was debrided to healthy bleeding tissue. Integra® was applied unmeshed and secured with staples to the periphery and quilted to the wound bed. To prevent shear, Integra was further secured with a non-shear primary dressing Telfa Clear (Convidien), overlying elasticated gauze and a nanocrystalline silver dressing. This was held in place with a bulky absorbent secondary dressing secured by crepe bandages. Postoperatively patients returned to the burns ward or burns intensive care unit depending on the extent of their burn injury.
Wounds were inspected for seroma, haematoma or infection and dressings changed every 48-72 hours following Integra® application. Once adequate vascularisation had occurred, typically after three to four weeks, the temporary silicone layer was removed and a thin split skin graft (8/1000th of an inch in thickness) was applied.
Surgical technique – Matriderm
Matriderm® application occurred at the time of primary burn excision. Following anaesthesia and positioning, patients were cleaned and prepped twice with aqueous betadine. Burns were excised down to healthy bleeding viable tissue. Matriderm was applied unmeshed and a thin split skin graft (8/1000th of an inch in thickness) secured overlying it with staples or dissolvable sutures to the periphery and for quilting. Then non-adherent, shear-reducing dressings were applied as for Integra®. Post-operatively, patients returned to the burns ward or burns intensive care unit depending on the extent of their burn injury. Initial graft check typically occurred after 48 hours with donor site wound review at 14 days.
Definitions
The number of surgeries relates to the number of surgeries a patient has at the site of DRT use. Dressing changes were not included even if these occurred in theatre, unless further burn debridement, excision or grafting occurred.
Time to 1st stage Integra or Matriderm application was measured from the time of initial burn injury. Length of stay was from patient admission to first discharge. Patients with small burns may not be admitted until the date of their surgery, while those with larger burns are admitted at the time of initial burn assessment.
Percentage take of Integra was calculated from patients’ intra-operative records. DRT was considered to have “taken” if it was fully adherent to the underlying tissues and therefore vascularisation had occurred. In patients treated with Matriderm®, percentage graft take and Matriderm take were considered equal and recorded from post-operative inpatient or outpatient notes.
Patients who developed an infection within the DRT were identified from patient notes, intra-operative findings recorded on operation notes and microbiology results. Major infection was defined as one leading to greater than ten percent loss of DRT and minor infection as one leading to less than this. Complications in terms of haematoma, infection, contracture and hypertrophic scarring were recorded only if they occurred at the site of DRT use.
Outcomes
Outcomes assessed were graft take, time to healing of DRT treated area and presence of complications. Healing time was taken as the date that healing was recorded in a patient’s wound care notes.
Statistics
Significance was calculated using the student’s ttest for continuous data and chi-squared test for binary data.
Results
Demographics
The DRTs used for primary burn reconstruction were Integra® and Matriderm. In a 13-year period, between January 2003 and December 2016, DRTs were used in primary burn reconstruction in acute care for 94 patients (59 Matriderm, 35 Integra). Indications for the use of DRT were: high percentage TBSA burns with limited donor sites, full thickness burns exposing vital structures or burns over aesthetically or functionally important areas.
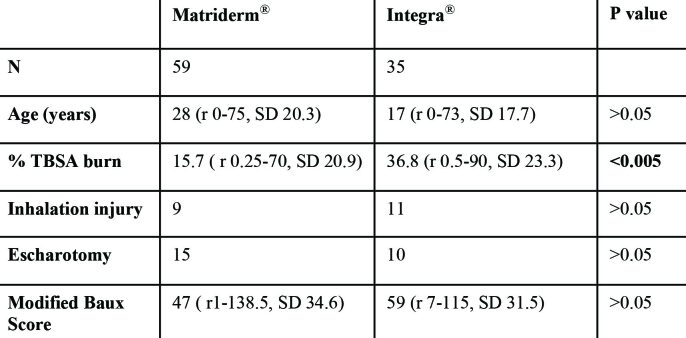
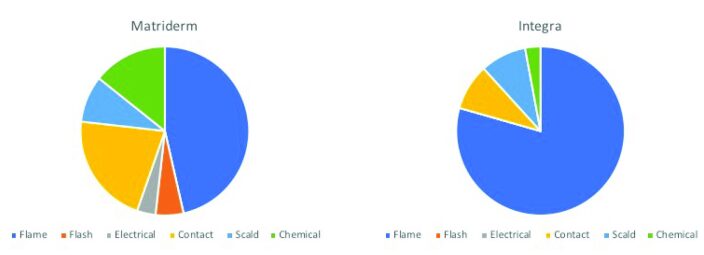
The mean age of patients was 17 +/- 17.7 (Integra ) and 28 +/- 20.3 (Matriderm). There was a significant difference in the presence of inhalational injury (12/35 Integra, 9/59 Matriderm, p=0.02) between the groups but not in modified Baux Score or the need for escharotomy (Table I). Three patients died in the Matriderm group and one in the Integra group, all from sepsis. Flame burns were the most common burns in both groups: 77% (27/35) Integra and 46% Matriderm (26/59) (Fig. 1).
Table I. Patient demographics.
Fig. 1. Mechanism of burn injury for patients treated with Matriderm (left) and Integra (right).
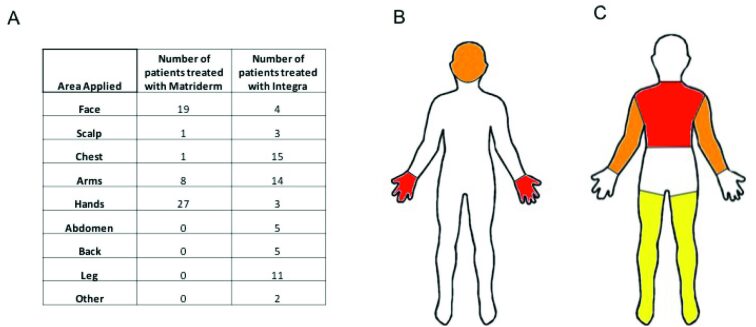
Use of dermal substitutes Patients treated with Integra had significantly larger percentage TBSA burn (36.8% +/- 23.3 (with mean 33% TBSA +/- 23 deep dermal or full thickness) compared to 15.7% +/- 20.9 (with 13% +/- 19 deep dermal or full thickness), p < 0.005. Matriderm® was used primarily to resurface the hands and face. In contrast, Integra was used mainly on the limbs and back (Fig. 2).
Fig. 2. A) Actual number of patients treated with each DRT at each body area. B) Diagrammatic representation of areas Matriderm most commonly applied to. C) Diagrammatic representation of areas Integra most commonly applied to.
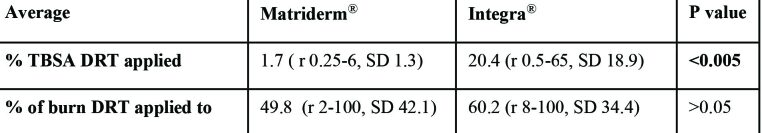
Integra was used to cover a significantly larger percentage TBSA: average 20.4% +/- 18.9 (minimum 0.5, maximum 65) compared to 1.7% +/- 1.3 (minimum 0.25, maximum 6) (Table II). There was no significant difference in the percentage of a patient’s total burn that each dermal substitute was applied to: 60.2% +/- 34.4 Integra, 49.8% +/- 42.1 Matriderm® (Table II).
Table II. Use of Matriderm and Integra based on percentage TBSA.
Time frame
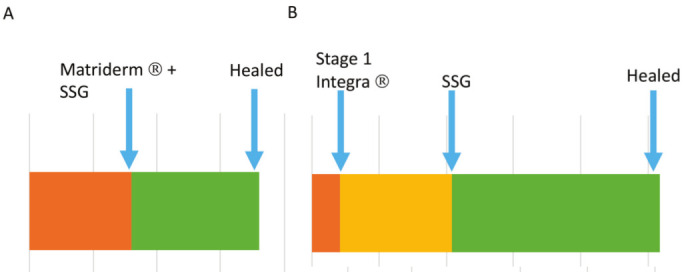
Integra was applied 4.1 +/- 6.8 days post-burn and SSG applied 20.9 +/- 5.1 days later. Matriderm was typically applied at day 16.0 +/- 20.0 post burn (Fig. 3), with SSG applied at the time of Matriderm application.
Fig. 3. Timeline of Matriderm A: and Integra B: use from time of injury to healing.
Outcomes
Graft take. There was no difference in percentage take of DRT (Matriderm 84% +/- 33.3, Integra 2.9% +/- 39.1, p 0.2). Average graft loss in the Integra group was 14.6% +/- 30.0. Complete loss of autograft occurred in six patients managed with Integra and two with Matriderm. This was statistically significant (Chi-squared test, p 0.01). Further grafting was required to DRT-treated areas in eight Matriderm and 11 Integra cases. Allograft was used as a temporising measure on exposed areas following Integra debridement due to infection in 13 patients.
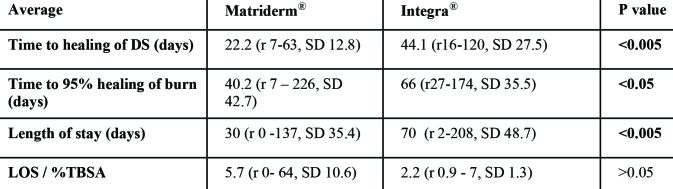
Time to healing. Time to 95% healing of burn was measured from date of burn. Patients treated with Integra® had significantly longer time to healing of the DRT treated area (mean 44.1 days c.f. 20.1) and 95% healing of all burnt area (66 days c.f. 40.2 days), as well as significantly longer length of stay (Table III). However, when length of stay is adjusted for percent TBSA there is no significant difference (Table III).
Table III. Table demonstrating healing times and length of stay for patients treated with Matriderm® and Integra.
Time from burn to healing of DRT site was 56.1 days for Integra and 36 days for Matriderm. This was 20.0 days post SSG for Matriderm and 31 days for Integra.
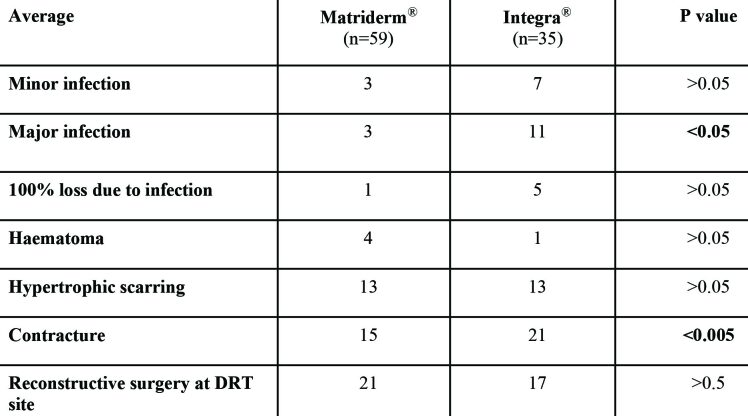
Early complications. Infection of the DRT site was reported in 18 patients treated with Integra and six managed with Matriderm. There was no significant difference in the number of minor infections in each group, however there were significantly more major infections at the site of DRT use in those managed with Integra (11/35) compared to Matriderm (3/59) (Table IV). The most common organisms causing infection in the Matriderm group were Staphylococcus spp (including coagulase-negative staphylocci and Staphylococcus aureus) and Group A Streptococcus. In the Integra group the most common infective organisms were Staphylococcus spp and Pseudomonas aeruginosa. Allograft was used at sites initially treated with Integra following infection in 13 cases.
Complete loss of DRT due to infection was significantly higher in the Integra group (5/35 c.f. 1/59). One patient in both groups had 100% DRT loss without any evidence of infection. There was no difference in haematoma development between the two groups: (1/35) Integra, (4/59) Matriderm (p=0.2).
Late complications. Hypertrophic scarring affected 13 Matriderm treated patients and 13 Integra patients. This difference was not significant (p=0.06). Significantly fewer patients developed burn contractures at the site of DRT use in the Matriderm cohort (15 c.f. 21). However, there was no difference in the need for secondary reconstructive surgery at the site of DRT use between the two groups (48.6% Integra, 35.5% Matriderm).
Table IV. Comparison of complications for patients treated with Matriderm® and Integra.
Discussion
The DRTs Integra and Matriderm have played an increasingly important role in primary burns reconstruction within our service over the last 13 years. The differing roles we use Integra and Matriderm for are demonstrated by the average percentage TBSA of burn we use each of them on and the differing body areas they are most commonly used to cover.
In our experience, two-stage Integra provides a valuable treatment option in patients with extensive burns where there is inadequate donor skin available for immediate autografting by allowing early burn excision and early definitive wound cover, but delays the need for autografting for around three weeks, allowing time for donor site healing. This is particularly valuable in patients with burns over 50% TBSA. Our use of Integra in this way is evident as the average percentage TBSA burn of a patient treated with Integra is 37% (minimum 0.5% TBSA, maximum 90%). Integra is typically used to cover on average 60% of the total burn a patient has sustained. Following complete excision of burns, we typically apply Integra on day four post burn. The dermal matrix layer supports the formation of a “neodermis” aiding revascularisation and collagen deposition, which over time develops into reticular and papillary dermis.7 An advantage of this is improved vascularisation in poor recipient sites, increasing the likelihood of graft take and allowing the use of thinner autografts.8 Around 21 days later the silicone epidermal layer is discarded and SSG is applied. During this 21-day period wound checks and dressing changes are performed every 48 hours.
Our unit favours Matriderm for patients with small burns in areas of functional or cosmetic importance. The use of a dermal matrix in these areas allows deep burns, even those exposing structures such as tendons, to be grafted. Improved cosmesis is achieved with the use of sheet rather than meshed graft.9 The one-stage nature of Matriderm® reduces the need for further procedures and prolonged inpatient stay. Although Integra have now released a single stage product, we do not currently have experience of using this in a large cohort of patients. Despite the differing indications for the use of both DRT and the significant difference in burn severity between the groups, graft take was comparable (Integra 85% +/- 30.0 and Matriderm 84.0% +/- 33.3) and in line with other centres.1 The lack of significant difference in graft take is interesting also given the differing extent of graft application and the timing (immediate versus delayed). However, significantly more patients treated with Integra had complete loss of autograft than with Matriderm (6/35 c.f. 2/59) and required further re-grafting to DRT treated sites. This may be representative of the patients within the Integra group, who had significantly larger burns and therefore are typically more unwell.
Time to healing after DRT use is comparable to the use of SSG alone10 and in our series faster healing was seen in DRT-treated areas. The use of VAC dressings can improve both DRT and autograft take and are used in patients undergoing secondary burns reconstruction. However we do not routinely use VAC dressings when using DRT in patients undergoing primary burn reconstruction due to the quality of surrounding skin.
Our experience is that patients treated with Matriderm have significantly shorter length of stay LOS) than those treated with Integra (average 30 days +/- 35.4 c.f. 70 days +/- 48.7), however they also had significantly smaller percentage TBSA burns (average %TBSA burn 15.7 +/- 20.5 c.f. 36.8 +/- 23.3). When length of stay is adjusted for percentage TBSA of burn there is no significant difference between the two groups, despite Integra being a two-stage process. In fact, this delayed need for autografting can be advantageous in these patients’ management, ensuring patients have adequate donor site availability for grafting.
In our 13-year experience we have found DRTs to be safe and effective in the treatment of acute burns. Infection is the most commonly reported complication of DRT use1 and was the most frequently occurring complication in our population. Due to the physiological effects of burns, patients affected are already at high risk of developing infection. We saw significantly more major infections in the Integra group compared to Matriderm (11/35 c.f. 3/59). There are several possible explanations for this. Firstly, these patients have more extensive burns than those we treat with Matriderm and therefore have a greater predisposition to infection. Secondly, the presence of the silicone epidermal layer provides a surface under which seromas can develop and become infected.8 We frequently use allograft in areas where Integra has become infected, either directly on to areas where Integra has been removed or to cover the dermal layer following removal of the silicone covering. Following this we have a high success rate with autografting. Recognising the high risk of infection in patients treated with DRTs, many centres including our own give prophylactic post-operative antibiotics.1 Our standard regime is five days of Benzylpenicillin and Gentamicin. Resultantly, our infection rates are in line with those reported elsewhere for DRT use1 and the most common causative organisms are Staphylococcus spp and Psuedomonas spp.
The long-term outcome we were interested in assessing was the rate of hypertrophic scarring and contractures. Heimback et al. reported that 57% of burnt patients treated with SSG alone developed hypertrophic scarring.8 In this cohort fewer patients developed hypertrophic scarring (13/59 Matriderm, 13/35 Integra). This rate is also lower than that reported in the early use of dermal substitutes.8 Contracture development is common following burn injury, affecting up to 54% of patients.11 Contractures result in poor cosmesis and functional limitation,12 and as a result they are frequently an indication for further surgery. Our study and others13,14 report reduced levels of wound contracture in patients treated using DRTs (21/35 Integra and 15/59 Matriderm). This is in keeping with research demonstrating that DRT use improves skin elasticity subjectively compared to the use of SSG alone4 and results in improved cosmetic outcome.15 Interestingly, in our patient cohort there was a significant difference in contracture rates between patients managed with Matriderm and Integra (Chi squared test p < 0.005). This may be due to the presence of elastin within Matriderm’s matrix which interrupts myofibroblast differentiation and therefore subsequent collagen contraction,16 thereby potentially improving the elasticity of regenerated skin. The reduced rates of scar contracture reported in our cohort justify our choice of using Matriderm in addition to SSG in areas of functional and aesthetic importance. No studies have objectively demonstrated improved elasticity in wounds treated with Matriderm. Interestingly, despite the reduced contracture and hypertrophic scarring rates seen in the Matriderm treated group, there was no significant difference in the need for secondary reconstructive surgery dependent on DRT used (21/59 Matriderm, 17/35 Integra ). This is likely due to the functional and aesthetic importance of the areas we typically treat with the Matriderm and so the greater impact of contractures and hypertrophic scarring in these areas if they do occur.
Despite the increasing use of DRT, few studies compare long-term outcomes. In particular, further research is needed to directly compare the functional and aesthetic outcomes of patients whose primary burn reconstruction involves the use of DRTs and also the impact that DRT use has on patients’ physiological response to burn injury and the number of procedures they require when used in the management of major burns. The main limitation of this study was its retrospective nature and therefore the reliance on information recorded within patients’ notes. Further prospective multi-centre studies are needed to evaluate functional and aesthetic outcomes after DRT and compare these to patients who have been managed with SSG alone.
Conclusion
Early tangential excision and wound closure with SSG or skin substitutes remains the gold standard treatment for deep dermal or full thickness burns. In our experience, dermal regeneration templates can be safely and effectively used to address some of the limitations of SSG, by addressing problems with donor site availability and morbidity as well as reducing the risk of secondary contraction and hypertrophic scarring which result from destruction of the dermis.
References
- 1.Lohana P, Hassan P, Watson SB. Integra in burns reconstruction: our experience and report of an unusual immunological reaction. Ann Burns Fire Disasters . 2014;27(1):17–21. Available from:http://www.ncbi.nlm.nih.gov/pubmed/25249843 . [PMC free article] [PubMed] [Google Scholar]
- 2.Shakespeare P. Burn wound healing and skin substitutes. Burns . 2001;27(5):517–522. Available from:http://www.ncbi.nlm.nih.gov/pubmed/11451610 . [PubMed] [Google Scholar]
- 3.Ryssel H, Germann G, Kloeters O, Gazyakan E, Radu CA. Dermal substitution with Matriderm in burns on the dorsum of the hand. Burns . 2010;36(8)X:1248–1253. doi: 10.1016/j.burns.2010.05.003. Available from:http://linkinghub.elsevier.com/retrieve/pii/S0305417910001178 . [DOI] [PubMed] [Google Scholar]
- 4.Nguyen DQA, Potokar TS, Price P, Dai QA. An objective long-term evaluation of Integra (a dermal skin substitute) and split thickness skin grafts, in acute burns and reconstructive surgery. [cited 2017 Sep 24];Burns. doi: 10.1016/j.burns.2009.07.011. Available from:https://ac.elscdn.com/S0305417909004586/1-s2.0-S0305417909004586-main.pdf?_tid=c1e98cb2-a135-11e7-ad2c-00000aab0f6cacdnat=1506263972_e02a4df64de570d35b7177706d5e133f . [DOI] [PubMed] [Google Scholar]
- 5.Integra Life Sciences Corporation. [cited 2017 Sep 26];Integra’s Physician Training Site . Available from:http://www.ilstraining.com/default.html . [Google Scholar]
- 6.MatriDerm - MedSkin Solutions Dr. Suwelack AG. [cited 2018 Feb 2]; Available from:http://www.medskinsuwelack.com/en/matriderm.html . [Google Scholar]
- 7.Stern R, McPherson M, Longaker MT. Histologic study of artificial skin used in the treatment of full-thickness thermal injury . J Burn Care Rehabil . doi: 10.1097/00004630-199001000-00003. Available from:http://www.ncbi.nlm.nih.gov/pubmed/2179224 . [DOI] [PubMed] [Google Scholar]
- 8.Heimbach D, Luterman A, Burke J, Cram A. Artificial dermis for major burns. A multi-center randomized clinical trial. Ann Surg . 1988;208(3):313–320. doi: 10.1097/00000658-198809000-00008. Available from:http://www.ncbi.nlm.nih.gov/pubmed/3048216 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ryssel H, Gazyakan E, Germann G, Ohlbauer H. The use of MatriDerm in early excision and simultaneous autologous skin grafting in burns—a pilot study. Burns. 2008;34(1):93–97. doi: 10.1016/j.burns.2007.01.018. Available from:http://linkinghub.elsevier.com/retrieve/pii/S0305417907000332 . [DOI] [PubMed] [Google Scholar]
- 10.Haslik W, Kamolz L-P, Nathschläger G, Andel H. First experiences with the collagen-elastin matrix Matriderm as a dermal substitute in severe burn injuries of the hand. Burns . 2007;33(3):364–368. doi: 10.1016/j.burns.2006.07.021. Available from:http://linkinghub.elsevier.com/retrieve/pii/S0305417906002282 . [DOI] [PubMed] [Google Scholar]
- 11.Oosterwijk OM, Mouton LJ, Schouten H, Disseldorp LM. Prevalence of scar contractures after burn: a systematic review. Burns . 2017;43(1):41–49. doi: 10.1016/j.burns.2016.08.002. Available from:http://www.ncbi.nlm.nih.gov/pubmed/27639820 . [DOI] [PubMed] [Google Scholar]
- 12.Harrison CA, MacNeil S. The mechanism of skin graft contraction: an update on current research and potential future therapies. Burns . 2008;34(2):153–163. doi: 10.1016/j.burns.2007.08.011. Available from:http://www.ncbi.nlm.nih.gov/pubmed/18226455 . [DOI] [PubMed] [Google Scholar]
- 13.Haslik W, Kamolz L-P, Manna F, Hladik M. Management of full-thickness skin defects in the hand and wrist region: first long-term experiences with the dermal matrix Matriderm. J Plast Reconstr Aesthetic Surg , 2010;63(2):360–364. doi: 10.1016/j.bjps.2008.09.026. Available from:http://www.ncbi.nlm.nih.gov/pubmed/19042169 . [DOI] [PubMed] [Google Scholar]
- 14.Hur G-Y, Seo D-K, Lee J-W. Contracture of skin graft in human burns: effect of artificial dermis. Burns . 2014;40:1497–1503. doi: 10.1016/j.burns.2014.08.007. Available from:https://ac.els-cdn.com/S0305417914002769/1-s2.0-S0305417914002769-main.pdf?_tid=c5dbeabc-a302-11e7-a55b-00000aacb360acdnat=1506461976_6225750334077391aa308418bafba7dd . [DOI] [PubMed] [Google Scholar]
- 15.Dantzer E, Queruel P, Salinier L, Palmier B, Quinot JF. Dermal regeneration template for deep hand burns: clinical utility for both early grafting and reconstructive surgery. [cited 2017 Sep 26];Br J Plast Surg. doi: 10.1016/s0007-1226(03)00366-7. Available from:https://ac.els-cdn.com/ S0007122603003667/1-s2.0-S0007122603003667-main.pdf?_tid=e0993002-a2fe-11e7-a30a-00000aacb362acdnat=1506460303_ec4fdbd0de73d0786b4636fb1971fb54 . [DOI] [PubMed] [Google Scholar]
- 16.Lamme EN, de Vries HJ, van Veen H. Extracellular matrix characterization during healing of full-thickness wounds treated with a collagen/elastin dermal substitute shows improved skin regeneration in pigs. J Histochem Cytochem . 1996;44(11):1311–1322. doi: 10.1177/44.11.8918906. Available from:http://www.ncbi.nlm.nih.gov/pubmed/8918906 . [DOI] [PubMed] [Google Scholar]