Abstract
Background
As the research documenting loneliness as a risk factor for morbidity and mortality continues to grow, it becomes increasingly critical to understand the mechanics of this relationship. This study assessed whether sleep disturbance mediates the relationship between loneliness and health.
Method
Data came from the 2006, 2010, and 2014 waves of the Health and Retirement Study, a longitudinal study of older Americans; participants ≥ 65 who completed the Psychosocial and Lifestyle Questionnaire in 2006 were included (n = 5067). Measures include the Hughes loneliness scales, a modified version of the Jenkins sleep scale, and self-reported health. Cross-lagged mediation models (i.e., path analysis) were used to model the relationships between loneliness, sleep disturbance, and self-reported health over the 8-year span.
Results
Loneliness predicted subsequent sleep disturbance, which in turn predicted subsequent self-reported health. Moreover, there was evidence of both direct and indirect effects (via sleep disturbance) of loneliness on self-reported health. These effects remained after controlling for demographics, isolation, and depression.
Conclusion
Sleep disturbance partially mediates the relationship between loneliness and self-reported health over 8 years. These findings are not attributable to isolation or depression. Further research is necessary to develop and assess a more comprehensive model of how loneliness shapes health. This study indicates that targeting sleep disturbance may mitigate the health risks of loneliness in older Americans.
Keywords: Loneliness, Sleep, Health, Older adults, Aging
Introduction
In 1988, House, Landis, and Umber published a review contending that social relationships shape health and emphasized the importance of research to identify the mechanisms underlying this association. The past 30 years have marked the proliferation of research substantiating this conclusion—several meta-analyses confirm that social factors predict morbidity and mortality—yet the mechanisms underlying this association remain unclear [1–5].
As the field has sought to unravel the links between social factors and health, loneliness (i.e., perceived social isolation) has gained growing attention as a risk factor. Loneliness has been linked to increased risk for coronary heart disease [6, 7], functional decline [8], and mortality [2], among other health outcomes, yet it remains unclear how loneliness may contribute to poor health. Cacioppo et al. (2002) proposed sleep disturbance as a mechanism explaining the effect of loneliness on health after showing that lonely college students have reduced sleep efficiency and increased wake time after sleep onset than their non-lonely counterparts [9]. A recent meta-analysis synthesized findings from 34,254 participants across 24 studies to show a medium-sized association (r = .27) between loneliness and self-reported sleep disturbance, whereby sleep disturbance was defined as either insomnia symptoms or impaired sleep quality [10]. Moreover, there is evidence that loneliness predicts subsequent sleep disturbance [11–14]. However, the research directly examining sleep disturbance as a mechanism linking loneliness and health outcomes remains limited.
Only three studies have examined sleep disturbance as a possible mediator of the association between loneliness and health [15–17]. First, Segrin and Passalacqua (2010) examined a convenience sample of 265 adults to show that sleep adequacy, in addition to other health behaviors, mediated the relationship between loneliness and health using the Baron and Kenny (1986) mediation analytical procedure [16]. Second, Segrin and Domschke (2011) used structural equation modeling to examine the relations between social support, loneliness, sleep quality, and health [15]. Loneliness was associated with poorer sleep quality, which in turn was associated with worse health (as measured by health quality of life, health problems, and global health rating). Furthermore, Segrin and Domschke found significant indirect effects of loneliness via sleep quality on both health quality of life and health problems. Third, Christiansen, Larsen, and Lasgaard (2016) showed that poor sleep mediated the relationship between loneliness and both diabetes and migraine in a sample of older adults (> 65 years) living in Denmark [17]. Collectively, these studies suggest that sleep disturbance mediates the association between loneliness and health. However, all three studies were cross-sectional, a critical limitation in light of the inherently longitudinal nature of mediation and the evidence that cross-sectional mediation analyses produce biased estimates [18]. To date, there is no longitudinal research examining sleep disturbance as a mediator of the association between loneliness and health.
It is critical to examine sleep as a mechanism underlying the association between loneliness and health in older Americans. Older adults represent a growing population in the USA [19]; the United States Census Bureau estimates that by 2035, the population of older Americans will surge to 78 million [20]. As the number of older adults rises, the impact of their health in terms of human suffering, medical utilization, and medical costs rises, making it increasingly critical to understand—and in turn target—the factors underlying healthy aging [21]. Furthermore, the associations among sleep, loneliness, and health may differ in older adults in comparison to younger populations.
The strength and vulnerability integration (SAVI) model outlines ways in which aging may color the associations between loneliness, sleep, and health (Charles, 2010). The SAVI model contends that older adults possess strengths, i.e., enhanced coping strategies, and vulnerabilities, i.e., decreased ability to recover from the sustained arousal accompanying stressful situations. Increased strengths in coping include improved emotional regulation [23–25], reduced goal discrepancies (the difference between the actual versus the ideal self [26, 27], greater tendency towards downward or lateral social comparisons [28, 29], more complex emotional processing [30–32], greater attention towards positive as opposed to negative stimuli [33, 34], more expedient disengagement from negative experiences [35, 36], and lower perception of the severity of negative events [37, 38]. The SAVI model also incorporates the socioemotional selectivity theory (SST) as part of these age-related strengths [39]. The SST argues that humans are constantly aware of time, and that this awareness of time—and its finiteness—informs social goals. According to SST, there are two broad categories of social goals: knowledge-related and emotional. When humans view time as open-ended, they tend towards knowledge-related goals; when humans view time as limited, they tend towards emotional goals. As humans age, they perceive time as increasingly finite, and thus their preferences shift from knowledge-related to emotional social goals. This shift in turn contributes to greater emotional health enjoyed by older adults [39].
However, according to the SAVI model, older adults are more vulnerable to the sustained physiological arousal accompanying certain situations, such as the loss of social belonging, chronic uncontrollable stressors such as poverty, abuse, or a debilitating health condition, and neurological dysfunction [22]. Older adults are more at risk for many of these issues—as members of their social network die, chronic health conditions rise, and the incidence of cognitive impairment increases—yet are less equipped physiologically to cope with the sustained arousal accompanying these conditions. Aging is associated with changes in cardiovascular functioning and flattened patterns of cortisol (reflecting reduced flexibility in the neuroendocrine system), which may in turn amplify the harms of sustained arousal [22].
The SAVI and SST would predict increased resilience to loneliness in older adults; according to these models, older adults are more likely to seek out social partners who fulfill their emotional needs, more likely to attend to the positive aspects of these relationships, and less likely to seek out conflict within these relationships. However, older adults are more vulnerable to specific life events that could trigger or exacerbate loneliness—such as deaths of friends, family, and spouses and disability that increases the barriers to spending time with others—and the sustained arousal resulting from this loneliness.
The relationships between loneliness, sleep, and health may also differ in older adults due to the changes that occur in sleep over the lifespan (for a review, see Miner and Kryger, 2017 [40]). Older adults experience a phase advance in sleep, whereby they feel sleepy earlier in the evening and awake earlier in the morning [41]. Moreover, aging is associated with the following changes in sleep architecture: decreased total sleep time, sleep efficiency, slow wave sleep, and rapid eye movement sleep and increased time awake after sleep onset, arousals, and sleep latency [40, 42]. Older adults are at increased risk of insomnia symptoms, which in turn predict worse self-reported health, cognitive decline, depression, disability, institutionalization, cardiovascular disease, and death [43–48]. Older adults on average sleep less than younger adults, but this reduction in sleep does not appear to be due to a reduced need for sleep. The National Sleep Foundation recommends that older adults sleep 7–8 hours based on research showing that 6–9 hours of sleep in this population is associated with improved cognitive function, mental health, physical health, and quality of life [40, 49]. It is therefore of paramount importance to understand factors that may disrupt sleep in older adults, as this population is at increased risk for sleep disruption and this disruption is a risk factor for poor health outcomes.
The present study aimed to examine sleep disturbance as a possible mediator of the association between loneliness and self-reported health in a sample that resembles the population of older adults in the USA using a longitudinal cross-lagged mediation model over 8 years. We hypothesized that (1) there will be a direct effect of loneliness on sleep disturbance (i.e., loneliness will predict subsequent declines in sleep disturbance); (2) there will be a direct effect of sleep disturbance on self-reported health (i.e., sleep disturbance will predict subsequent decline in self-reported health); (3) there will be an indirect effect of loneliness on self-reported health via sleep disturbance (i.e., sleep disturbance will mediate the relationship between loneliness and health); and (4) controlling for demographics, isolation, and depression will attenuate the associations among all variables.
Methods
Sample
Data came from the 2006, 2010, and 2014 waves of the Health and Retirement Study (HRS), a nationally representative panel study of community-dwelling Americans entering retirement age [50]. Only participants aged 65 and above who completed the Psychosocial and Lifestyle Questionnaire in 2006, 2010, or 2014 were included in the present study. Characteristics of this sample are summarized in Table 1. In total, 5067 participants returned the Psychosocial and Lifestyle Questionnaire in 2006, 2010, or 2014. Of these, 4624 completed the Hughes Loneliness Scale in 2006, 3424 in 2010, and 2608 in 2014. In 2006, all 5067 participants completed the sleep disturbance scale, though only 4111 completed this scale in 2010 and 3121 in 2014. Similarly, 5059 participants reported on their self-reported health in 2006, 4111 in 2010, and 3120 in 2014. To assess for potential attrition bias, characteristics of the participants with data on any of the variables of interest (i.e., loneliness, sleep disturbance, and self-reported health; n = 3125) are presented in juxtaposition to those without data for any of these variables (n = 1942) in Table 1 alongside the characteristics of the full sample.
Table 1.
Sample Characteristics
| Full sample | Not lost to follow-up | Lost to follow-up | ||||
|---|---|---|---|---|---|---|
| n = 5,067 | n = 3,125 | n = 1,942 | ||||
| Frequency (%) | Mean (SD) [Range] | Frequency (%) | Mean (SD), [Range] | Frequency (%) | Mean (SD), [Range] | |
| Lonelinessa | −0.53 | −0.57 | −0.46 | |||
| (.53) | (0.51) | (0.56) | ||||
| [−1, 1] | [−1, 1] | [−1, 1] | ||||
| Sleep Disturbancea | 1.64 | 1.62 | 1.66 | |||
| (.51) | (0.51) | (0.52) | ||||
| [1,3] | [1,3] | [1,3] | ||||
| Self-reported Healtha,b | 2.92 | 2.72 | 3.24 | |||
| (1.08) | (1.02) | (1.10) | ||||
| [1,5] | [1,5] | [1,5] | ||||
| Agea | 74.31 | 72.48 | 77.26 | |||
| (7.12) | (5.88) | (7.92) | ||||
| [65, 104] | [65, 96] | [65, 104] | ||||
| Isolationa | 3.41 | 3.34 | 3.54 | |||
| (.75) | (.73) | (.76) | ||||
| [1,6] | [1,6] | [1.11,6] | ||||
| Depressiona | 1.44 | 1.24 | 1.76 | |||
| (1.91) | (1.82) | (2.02) | ||||
| [0, 8] | [0, 8] | [0, 8] | ||||
| Sex | ||||||
| Male | 2,188 (43.18) | 1,270 (40.64) | 918 (47.27) | |||
| Female | 2,879 (56.82) | 1,855 (59.36) | 1,024 (52.73) | |||
| Education | ||||||
| Less than high school | 1,214 (23.96) | 656 (20.99) | 558 (28.73) | |||
| GED | 234 (4.62) | 138 (4.42) | 96 (4.94) | |||
| High-school graduate | 1,702 (33.59) | 1,068 (34.18) | 634 (32.65) | |||
| Some college | 978 (19.30) | 620 (19.84) | 358 (18.43) | |||
| College and above | 939 (18.53) | 643 (20.58) | 296 (15.24) | |||
| Race | ||||||
| White/Caucasian | 4,281 (84.49) | 2,628 (84.10) | 1,653 (85.12) | |||
| Black/African American | 628 (12.39) | 391 (12.51) | 237 (12.20) | |||
| Other | 158 (3.12) | 106 (3.39) | 52 (2.68) | |||
| Ethnicity | ||||||
| Not Hispanic | 4,688 (95.52) | 2,881 (92.19) | 1,807 (93.05) | |||
| Hispanic | 379 (7.48) | 244 (7.81) | 135 (6.95) | |||
| Socioeconomic Status | ||||||
| Lower | 855 (16.87) | 455 (14.56) | 400 (20.60) | |||
| Lower Middle | 967 (19.08) | 537 (17.18) | 430 (22.14) | |||
| Middle | 1,058 (20.88) | 665 (21.28) | 393 (20.24) | |||
| Upper Middle | 1,122 (22.14) | 734 (23.49) | 388 (19.98) | |||
| Upper | 1,065 (21.02) | 734 (23.49) | 331 (17.04) | |||
| Marital Status | ||||||
| Married | 3,081 (60.81) | 2,003 (64.10) | 1,078 (55.51) | |||
| Partnered | 90 (1.78) | 58 (1.86) | 32 (1.65) | |||
| Separated/divorced | 415 (8.19) | 273 (8.74) | 142 (7.31) | |||
| Widowed | 1,363 (26.90) | 719 (23.01) | 644 (33.16) | |||
| Never married | 118 (2.33) | 72 (2.30) | 46 (2.37) | |||
At baseline
Higher values represent worse self-reported health
Lost to follow-up is defined as missing all three variables of interest (loneliness, sleep disturbance, and self-reported health) in 2014. SD = standard deviation.
The present study used data from the HRS, a publicly available dataset. The HRS has received approval from the University of Michigan Institutional Review Board (IRB) and all participants provided informed consent. All procedures performed in this study that involved human participants were in accordance with the ethical standards of the University of Michigan IRB and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Measures
Loneliness
Loneliness was measured using the Hughes Loneliness Scale [51]. This scale contains the following three questions: (1) “How often do you feel isolated from others?” (2) “How often do you feel left out?” and (3) “How often do you feel isolated from others?” [51]. Responses consist of “1 = Often,” “2 = Some of the time,” and “3 = Hardly ever or never.” Items were reverse coded then averaged to create a scale, whereby higher values represent higher levels of loneliness. When more than one item was missing, the scale score was also assigned missing [51]. The Hughes Loneliness Scale has demonstrated adequate validity and reliability in older adult samples [52].
Sleep Disturbance
Sleep disturbance was measured using a modified form of the Jenkins sleep scale [53] and included four items assessing feeling rested, difficulty falling asleep, difficulty staying asleep, and waking up too early. Responses include “Rarely or never,” “Sometimes,” and “Most of the time.” Sleep items were reverse coded and then averaged to create a total score, consistent with prior use in the literature [54]. Cronbach’s alpha statistics were .64 (in 2006), .62 (in 2010), and .63 (in 2014), consistent with the internal consistency demonstrated by the Jenkins sleep scale [53].
Self-Reported Health
Health was assessed via the question: “Would you say your health is excellent, very good, good, fair, or poor?” Higher values reflected worse self-reported health. Although a single-item and self-report measure, self-reported health is a well-supported measure of health: a meta-analysis synthesized 20 articles to show that self-reported health predicted all-cause mortality [55]. Moreover, the single-item self-reported health question strongly predicted mortality even after controlling for factors such as functional status, depression, and comorbidity is a strong predictor of mortality even after accounting for covariates [55].
Demographics
Participants answered questions about their age, sex (male, female), race (White/Caucasian, Black/African American, and other), ethnicity (Hispanic/not Hispanic), level of education (less than high school, high school graduate, General Educational Development, some college, college and higher), marital status (married, single, separated/divorced, widowed), and socioeconomic status (SES), which was calculated by subtracting total debt from the net worth variable [56] or the sum of all wealth components (e.g., house, automobile, salary). Then, the net worth variable was divided into quintiles. All categorical variables were dummy coded.
Isolation
Participants were asked to report the frequency of their contact with their social network as a measure of isolation. Contacts included meeting, speaking on the phone, or written/email communication; frequencies included “Three or more times a week,” “Once or twice a week,” “Once or twice a month,” “Every few months,” “Once or twice a year,” and “Less than once a year or never.” An overall score of isolation was calculated by reverse coding and averaging all items. The total score was set to missing if more than one item was missing [57].
Depression
Depression was assessed using the Center for Epidemiologic Studies Depression Scale – Revised (CESDR). Participants were asked to report whether (yes/no) they had certain experiences over the past week. Items included in this study were “I felt depressed,” “I felt that everything I did was an effort,” “I was happy,” “I enjoyed life,” “I felt sad,” and “I could not get going.” Items relating to sleep and loneliness were excluded. The total score was calculated by subtracting positively valanced items from the sum of other items [56].
Analyses
A longitudinal cross-lagged mediation model (time points: 2006, 2010, 2014) was conducted using path analysis to examine sleep disturbance as a potential mediator of the association between loneliness and self-reported health [58]. The model included paths from loneliness to subsequent sleep disturbance, sleep disturbance to subsequent self-reported health, and baseline loneliness to 2014 self-reported health; additionally, the model included cross-sectional associations at each time point across all variables or their error terms (e.g., loneliness in 2006 was set to correlate with sleep disturbance in 2006) and paths were drawn from each variable to subsequent time points of the same variable (e.g., path between loneliness in 2006 and loneliness in 2010).
A second cross-lagged mediation model, controlling for demographics, depression, and isolation, was then calculated. Specifically, the model controlled for the effect of age, race, ethnicity, and education on loneliness, sleep disturbance, and self-reported health in 2010 and 2014. The model also controlled for the effect of prior isolation, depression, marital status, and socioeconomic status on subsequent on loneliness, sleep disturbance, and self-reported health. For example, in the case of depression: depression in 2006 was included as a predictor of loneliness, sleep disturbance, and self-reported health in both 2010 and 2014 and depression in 2010 was included as a predictor of loneliness, sleep disturbance, and self-reported health in 2014 (for more information, please see study materials/result files available on the Open Science Framework).
To address the potential threat of bias due to missing data, expectation maximization was used for the path analyses, due to evidence that data were not missing completely at random (MCAR) from examination of the data and significant findings on Little’s MCAR test (ps < .001) [59]. Bootstrapping (2000 bootstrap samples) was used to calculate indirect effects and confidence intervals. Output and code for this study are available on the Open Science Framework (OSF): https://osf.io/jzk5g/?view_only=e9d52146d4ab4e1cac4d0fb89ba6eb46. Expectation maximization was conducted in IBM SPSS Statistics 25 and path analysis was conducted in IBM SPSS AMOS 25.
Results
The cross-lagged panel model fit using time points 2006, 2010, and 2014 with standardized path estimates is presented in Fig. 1. All paths were significant (ps < .001), but effect sizes were small. Loneliness predicted subsequent sleep disturbance (2006 to 2010: β = .09, B = .08, SE = .01, p < .001; 2010 to 2014: β = .06, B = .05, SE = .01, p < .001), which in turn predicted subsequent self-reported health (2006 to 2010: β = .08, B = .16, SE = .02, p < .001; 2010 to 2014: β = .03, B = .07, SE = .02, p < .001). There was a direct (β = .06, B = .10, SE = .02, p = .001) and an indirect (β = .003, 95% CI [.001, .005], p = .001) effect via sleep disturbance of loneliness in 2006 on self-reported health in 2014.
Fig. 1.
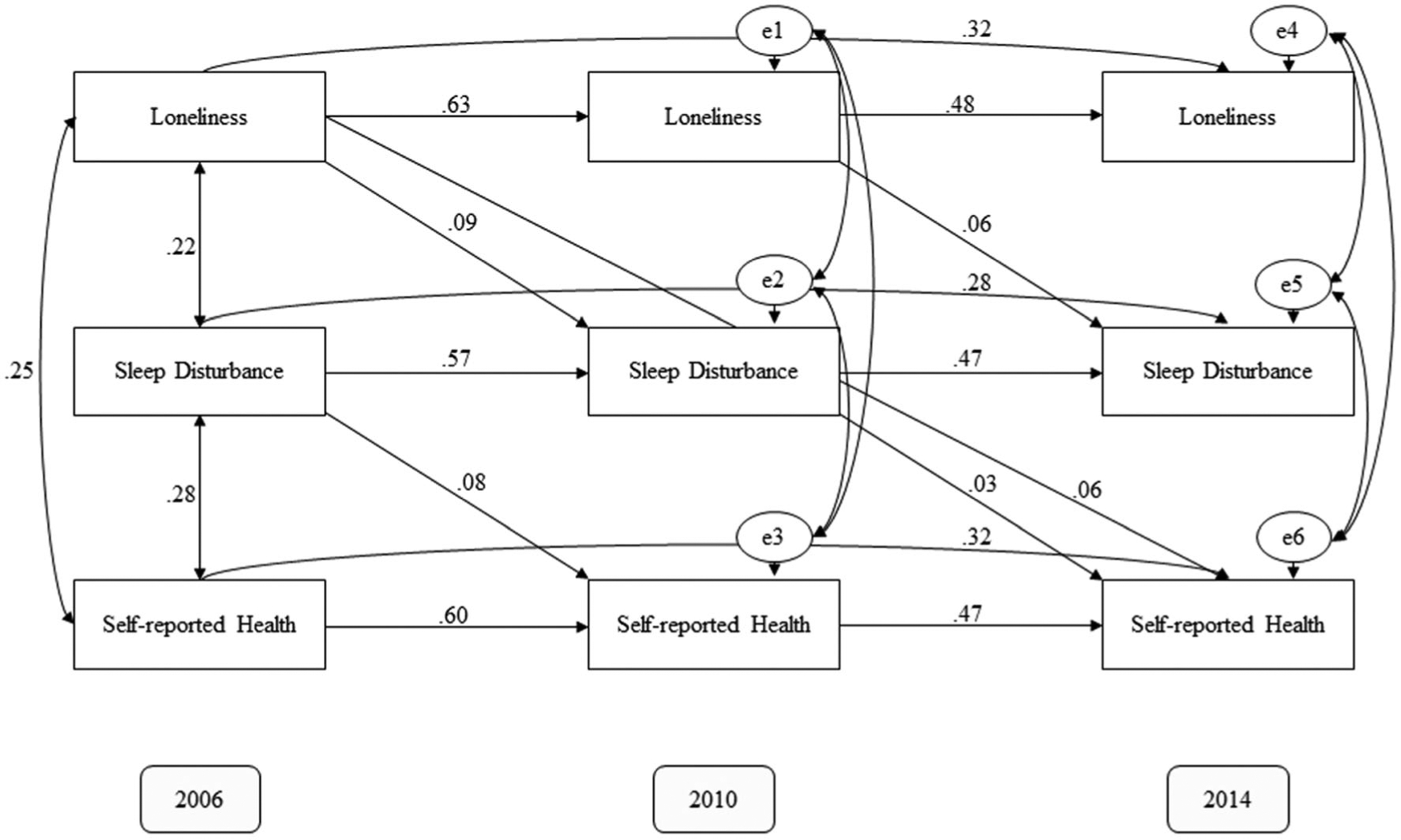
Cross-lagged mediation model (2006, 2010, 2014), with standardized regression weights. All paths are statistically significant
The chi-square (χ2) goodness-of-fit test was significant, χ2(13) = 573.86, p < .001, which is generally indicative of poor fit but not a good index for studies with a large sample size [60]. The root mean square of approximation (RMSEA) was .09 (≤ .08 is reflective of adequate fit); the comparative fit index (CFI) was .97 and the goodness-of-fit index (GFI) was .98 (≥ .95 is reflective of good fit). Overall, these indices are consistent with adequate model fit. However, the purpose of this analysis was to test the mediation hypothesis rather than identify the model that best captures the associations between loneliness, sleep disturbance, and self-reported health. Therefore, the specific paths assessed in this model were of greater relevance to this study’s hypotheses than the model’s fit statistics.
Accounting for age, gender, education, race, ethnicity, isolation, depression, marital status, and SES attenuated the paths from loneliness to sleep disturbance (2006 to 2010: β = .06, B = .05, SE = .01, p < .001; 2010 to 2014: β = .06, B = .06, SE = .01, p < .001) and the paths from sleep disturbance to self-reported health (2006 to 2010: β = .06, B = .12, SE = .02, p < .001; 2010 to 2014: β = .05, B = .10, SE = .02, p < .001). The direct (β = .03, B = .04, SE = .02, p = .014) and indirect effect (β = .00, 95% CI [.00, .01], p < .001) via sleep disturbance of loneliness in 2006 on self-reported health in 2014 were similarly attenuated but still statistically significant.
Fit indices were poor, as would be expected for a model controlling for potential confounds: χ2 goodness-of-fit test was significant, χ2(566) = 65,848.71, p < .001, RMSEA = .15, CFI = .25, GFI = .62. However, the purpose of this model was to ensure that the relationships of interest could not be entirely attributed to these additional factors, not to evaluate a model of the relationships between loneliness, sleep disturbance, self-reported health, and potential confounds. Therefore, fit statistics would be expected to be poor, as it is likely that many of the associations included in this model do not explain the relationship between loneliness, sleep, and health.
Discussion
Loneliness predicted subsequent sleep disturbance, which in turn predicted subsequent self-reported health. Moreover, there was evidence of both direct and indirect effects (via sleep disturbance) of loneliness on self-reported health. These effects remained after controlling for demographics, isolation, and depression; as such, findings cannot be attributed to these potential confounds. Collectively, these findings indicate that sleep disturbance partially mediates the association between loneliness and self-reported health.
This study is the first to longitudinally replicate previous cross-sectional research identifying sleep disturbance as a mediator of the association between loneliness and a subsequent health outcome [15–17]. Longitudinal mediational models are better equipped to speak to sleep disturbance as a mechanism underlying the relationship between loneliness and health because they can speak to direction of effects [58]. The detection of a partial mediation is consistent with previous cross-sectional work [15–17], despite the use of different measures (e.g., the general health subscale of the Medical Outcomes study versus a single-item rating of overall health) and constructs (e.g., diabetes versus global self-reported health) of health. Furthermore, this study’s findings are consistent with the theory proposed by Cacioppo, Hawkley, and colleagues [9, 61] that loneliness influences health through disrupting sleep. Moreover, the present study is the first to examine these relations in a sample that resembles the population of older adults in the USA: the previous cross-sectional work was limited to convenience samples [15, 16] and a sample of older adults living in Denmark [17], neither of which can speak to the US older adult population.
It is important to note that, although statistically significant, effects were small. The small size of effects could be due to the 4-year lag across data points: large effect sizes would be unlikely even if sleep disturbance were a major mechanism underlying the association between loneliness and health because of the assessment of these variables over the course of years. Further research is necessary to examine the association between daily and monthly fluctuations in loneliness, sleep disturbance, and health. It is also likely that sleep disturbance is but one of several routes through which loneliness may shape health; research is necessary to assess other potential mediators to develop a comprehensive understanding of how loneliness shapes health.
Certain limitations must be addressed. First, there was a high rate of attrition, which was not random. Expectation maximization was employed to mitigate the potential threat of attrition bias, but it remains possible that selective attrition biased results. Next, the measurement of sleep disturbance is not from a validated scale but rather a composite of sleep items. Future research is necessary to replicate findings using a validated scale of sleep disturbance as well as objective sleep measures. Finally, the present study controlled for potential confounds rather than examining the relationships among loneliness, sleep disturbance, and self-reported health in the context of these factors. The fit statistics for the model that included these controls was poor, as would be expected for a model that includes all potential confounds. Future research is necessary to understand how isolation, depressive symptoms, and demographics may interact with or moderate the links among loneliness, sleep, and health. Such an approach could be used to create a model for how loneliness, sleep, and health relate to one another in the context of other factors. Moreover, this study did not account for other potential confounds, to include cognitive decline (due to Alzheimer’s disease or other etiology) and trauma. Finally, although this study’s longitudinal design and use of path analysis allows for the careful study of direction of effects, experimental research is necessary to establish causality and thus speak to sleep disturbance as a mechanism underlying the association between loneliness and health.
Implications and Conclusion
The present study provides evidence for sleep disturbance as a pathway through which loneliness affects health in older adults. Understanding the impact of psychosocial factors on health outcomes is crucial to the continued, nuanced care of the expanding population of older adults in the USA. Loneliness is of particular relevance to older adults. Aging is associated with strengths such as greater positivity bias, present awareness, and emotion regulation, all of which likely protect against loneliness [22]. However, older adults are at heightened risk of health conditions—which may hinder their ability to interact with others—and of losses to their social network [22, 39]. Moreover, the sustained stress stemming from chronic loneliness may be particularly damaging for older adults due to changes in endocrine and cardiovascular functioning and sleep [22]. As such, it is critical to understand the web of social, biological, and psychological factors involved in the health and quality of life of this population.
The present study identifies sleep disturbance as a partial mediator of the connection between loneliness and self-reported health, thereby uncovering sleep disturbance as a treatment target to mitigate the potential effect of loneliness on health. This finding is promising in light of the efficacy of behavioral sleep medicine interventions for late-life insomnia [62, 63]: treating sleep disturbance in older adults may protect against the health risks of loneliness. The impact of research on healthy aging is of increasing importance. As the population of older Americans rises, so too does the opportunity to provide the best quality of life possible to this growing population. A steadily growing body of literature documents the importance of social relationships to healthy aging. Further research is necessary to understand how aging interacts with social processes and thereby gain an understanding of how to best direct policy and intervention efforts to optimize quality of life for older Americans.
Funding information
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number K23AG049955 (PI: Dzierzewski).
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References
- 1.Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10:227–37. 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- 2.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7:e1000316. 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sbarra DA, Law RW, Portley RM. Divorce and death: a meta-analysis and research agenda for clinical, social, and health psychology. Perspect Psychol Sci. 2011;6:454–74. 10.1177/1745691611414724. [DOI] [PubMed] [Google Scholar]
- 4.Manzoli L, Villari P, Pirone G, Boccia A. Marital status and mortality in the elderly: a systematic review and meta-analysis. Soc Sci Med. 2007;64:77–94. 10.1016/j.socscimed.2006.08.031. [DOI] [PubMed] [Google Scholar]
- 5.Shor E, Roelfs DJ, Yogev T. The strength of family ties: a meta-analysis and meta-regression of self-reported social support and mortality. Soc Networks. 2013;35:626–38. 10.1016/j.socnet.2013.08.004. [DOI] [Google Scholar]
- 6.Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102:1009–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thurston RC, Kubzansky LD. Women, loneliness, and incident coronary heart disease. Psychosom Med. 2009;71:836–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perissinotto CM, Cenzer IS, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012;172:1078–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cacioppo JT, Hawkley LC, Bernston GC, Ernst JM, Gibbs AC, Stickgold R, et al. Do lonely days invade the nights? Potential social modualation of sleep efficiency. Psychol Sci. 2002;13:384–7. 10.1111/j.0956-7976.2002.00469.x. [DOI] [PubMed] [Google Scholar]
- 10.Griffin SC, Williams AB, Ravyts S, Mladen S, Rybarczyk B. Loneliness and sleep: a systematic review and meta-analysis. Heal Psychol Open n.d. [DOI] [PMC free article] [PubMed]
- 11.Hom MA, Hames JL, Bodell LP, Buchman-Schmitt JM, Chu C, Rogers ML, et al. Investigating insomnia as a cross-sectional and longitudinal predictor of loneliness: findings from six samples. Psychiatry Res. 2017;253:116–28. 10.1016/j.psychres.2017.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobs JM, Cohen A, Hammerman-Rozenberg R, Stessman J. Global sleep satisfaction of older people: the Jerusalem Cohort Study. J Am Geriatr Soc. 2006;54:325–9. 10.1111/j.1532-5415.2005.00579.x. [DOI] [PubMed] [Google Scholar]
- 13.Jaremka LM, Andridge RR, Fagundes CP, Alfano CM, Povoski SP, Lipari AM, et al. Pain, depression, and fatigue: loneliness as a longitudinal risk factor. Health Psychol. 2014;33:948–57. 10.1037/a0034012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McHugh JE, Lawlor BA. Perceived stress mediates the relationship between emotional loneliness and sleep quality over time in older adults. Br J Health Psychol. 2013;18:546–55. 10.1111/j.2044-8287.2012.02101.x. [DOI] [PubMed] [Google Scholar]
- 15.Segrin C, Domschke T. Social support, loneliness, recuperative processes, and their direct and indirect effects on health. Health Commun. 2011;26:221–32. 10.1080/10410236.2010.546771. [DOI] [PubMed] [Google Scholar]
- 16.Segrin C, Passalacqua SA. Functions of loneliness, social support, health behaviors, and stress in association with poor health. Health Commun. 2010;25:312–22. 10.1080/10410231003773334. [DOI] [PubMed] [Google Scholar]
- 17.Christiansen J, Larsen FB, Lasgaard M. Do stress, health behavior, and sleep mediate the association between loneliness and adverse health conditions among older people? Soc Sci Med. 2016;152:80–6. 10.1016/j.socscimed.2016.01.020. [DOI] [PubMed] [Google Scholar]
- 18.Mitchell MA, Maxwell SE. A comparison of the cross-sectional and sequential designs when assessing longitudinal mediation. Multivariate Behav Res. 2013;48:301–39. 10.1080/00273171.2013.784696. [DOI] [PubMed] [Google Scholar]
- 19.Cohen JE. Human population: the next half century. Science (80-) 2003;302:1172–5. [DOI] [PubMed] [Google Scholar]
- 20.Bureau UC. Older people projected to outnumber children. US Census Bur Https//WwwCensusGov/Newsroom/Press-Releases/2018/Cb18-41-Population-Projections Html Accessed 2019;18. [Google Scholar]
- 21.Schneider EL, Guralnik JM. The aging of America: impact on health care costs. Jama. 1990;263:2335–40. [PubMed] [Google Scholar]
- 22.Charles ST. Strength and vulnerability integration (SAVI): a model of emotional well-being across adulthood. Psychol Bull. 2010;136: 1068–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gross JJ, Carstensen LL, Pasupathi M, Tsai J, Götestam Skorpen C, Hsu AYC. Emotion and aging: experience, expression, and control. Psychol Aging. 1997;12:590–9. [DOI] [PubMed] [Google Scholar]
- 24.Phillips LH, Henry JD, Hosie JA, Milne AB. Age, anger regulation and well-being. Aging Ment Heal. 2006;10:250–6. [DOI] [PubMed] [Google Scholar]
- 25.Charles ST, Carstensen LL. Emotion regulation and aging. Handb Emot Regul. 2007;307:327. [Google Scholar]
- 26.Cheng S-T. Age and subjective well-being revisited: a discrepancy perspective. Psychol Aging 2004;19:409, 415. [DOI] [PubMed] [Google Scholar]
- 27.Ryff CD. Possible selves in adulthood and old age: a tale of shifting horizons. Psychol Aging. 1991;6:286–95. [DOI] [PubMed] [Google Scholar]
- 28.Frey KS, Ruble DN. Strategies for comparative evaluation: maintaining a sense of competence across the life span. 1990.
- 29.Sheldon JP. Age and gender differences in the sources of self-evaluation valued by adult athletes. J Adult Dev. 2004;11:47–53. [Google Scholar]
- 30.Charles ST. Viewing injustice: age differences in emotional experience. Psychol Aging. 2005;20:159–64. [DOI] [PubMed] [Google Scholar]
- 31.Ong AD, Bergeman CS. The complexity of emotions in later life. Journals Gerontol Ser B Psychol Sci Soc Sci. 2004;59:P117–22. [DOI] [PubMed] [Google Scholar]
- 32.Magai C, Consedine NS, Krivoshekova YS, Kudadjie-Gyamfi E, McPherson R. Emotion experience and expression across the adult life span: insights from a multimodal assessment study. Psychol Aging. 2006;21:303–17. [DOI] [PubMed] [Google Scholar]
- 33.Isaacowitz DM. Motivated gaze: the view from the gazer. Curr Dir Psychol Sci. 2006;15:68–72. [Google Scholar]
- 34.Carstensen LL, Mikels JA. At the intersection of emotion and cognition: aging and the positivity effect. Curr Dir Psychol Sci. 2005;14:117–21. [Google Scholar]
- 35.Birditt KS, Fingerman KL. Age and gender differences in adults’ descriptions of emotional reactions to interpersonal problems. Journals Gerontol Ser B Psychol Sci Soc Sci. 2003;58:P237–45. [DOI] [PubMed] [Google Scholar]
- 36.Diehl M, Coyle N, Labouvie-Vief G. Age and sex differences in strategies of coping and defense across the life span. Psychol Aging. 1996;11:127–39. [DOI] [PubMed] [Google Scholar]
- 37.Story TN, Berg CA, Smith TW, Beveridge R, Henry NJM, Pearce G. Age, marital satisfaction, and optimism as predictors of positive sentiment override in middle-aged and older married couples. Psychol Aging. 2007;22:719–27. [DOI] [PubMed] [Google Scholar]
- 38.Lefkowitz ES, Fingerman KL. Positive and negative emotional feelings and behaviors in mother-daughter ties in late life. J Fam Psychol. 2003;17:607–17. [DOI] [PubMed] [Google Scholar]
- 39.Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously: a theory of socioemotional selectivity. Am Psychol. 1999;54:165–81. [DOI] [PubMed] [Google Scholar]
- 40.Miner B, Kryger MH. Sleep in the aging population. Sleep Med Clin. 2017;12:31–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Monk TH. Aging human circadian rhythms: conventional wisdom may not always be right. J Biol Rhythm. 2005;20:366–74. [DOI] [PubMed] [Google Scholar]
- 42.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. [DOI] [PubMed] [Google Scholar]
- 43.Dew MA, Hoch CC, Buysse DJ, Monk TH, Begley AE, Houck PR, et al. Healthy older adults’ sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom Med. 2003;65:63–73. [DOI] [PubMed] [Google Scholar]
- 44.Vaz Fragoso CA, Gill TM. Sleep complaints in community-living older persons: a multifactorial geriatric syndrome: (see editorial comments by Dr. Michael V. Vitiello on pp 1882–1883). J Am Geriatr Soc. 2007;55:1853–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bloom HG, Ahmed I, Alessi CA, Ancoli-Israel S, Buysse DJ, Kryger MH, et al. Evidence-based recommendations for the assessment and management of sleep disorders in older persons. J Am Geriatr Soc. 2009;57:761–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ayling K, Fairclough L, Tighe P, Todd I, Halliday V, Garibaldi J, et al. Sleep and stressor exposure in relation to circadian rhythms in catecholamine excretion. Sleep 2016;13:No Pagination Specified-No Pagination Specified. doi: 10.3389/fnagi.2015.00232. [DOI] [Google Scholar]
- 47.Stone KL, Ensrud KE, Ancoli-Israel S. Sleep, insomnia and falls in elderly patients. Sleep Med. 2008;9:S18–22. [DOI] [PubMed] [Google Scholar]
- 48.Ancoli-Israel S, Cooke JR. Prevalence and comorbidity of insomnia and effect on functioning in elderly populations. J Am Geriatr Soc. 2005;53:S264–71. [DOI] [PubMed] [Google Scholar]
- 49.Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Heal. 2015;1:40–3. [DOI] [PubMed] [Google Scholar]
- 50.Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JWR, Weir DR. Cohort profile: The Health and Retirement Study (HRS). Int J Epidemiol. 2014;43:576–85. 10.1093/ije/dyu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clarke P, Fisher G, House J, Smith J, Weir D. Guide to content of the HRS Psychosocial Leave-Behind Participant Lifestyle Questionnaires: 2004 & 2006. HRS Psychosoc Work Gr Surv Res Center, Inst Soc Res Univ Michigan 2008:1–48. [Google Scholar]
- 52.Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26:655–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jenkins CD, Stanton B-A, Niemcryk SJ, Rose RM. A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 1988;41:313–21. [DOI] [PubMed] [Google Scholar]
- 54.Lee JH, Chopik WJ, Schiamberg LB. Longitudinal associations between marital quality and sleep quality in older adulthood. J Behav Med. 2017;40:821–31. [DOI] [PubMed] [Google Scholar]
- 55.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question: a meta-analysis. J Gen Intern Med. 2006;21:267–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chien S, Campbell N, Hayden O, Hurd M, Main R, Mallett J, et al. RAND HRS data documentation, version M. St Monica, CA RAND Cent Study Aging 2013.
- 57.Smith J, Fisher G, Ryan L, Clarke P, House J, Sonnega A, et al. Psychosocial and lifestyle questionnaire 2006–2010: Documentation Report Core Section LB 2013:1–72. [Google Scholar]
- 58.Selig JP, Preacher KJ. Mediation models for longitudinal data in developmental research. Res Hum Dev. 2009;6:144–64. 10.1080/15427600902911247. [DOI] [Google Scholar]
- 59.Little RJA. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83:1198–202. [Google Scholar]
- 60.Bowen NK, Guo S. Structural equation modeling. Oxford University Press; 2011. [Google Scholar]
- 61.Cacioppo JT, Hawkley LC. Social isolation and health, with an emphasis on underlying mechanisms. Perspect Biol Med. 2003;46:S39–52. 10.1353/pbm.2003.0049. [DOI] [PubMed] [Google Scholar]
- 62.Dzierzewski JM, Griffin SC, Ravyts S, Rybarczyk B. Psychological interventions for late-life insomnia: current and emerging science. Curr Sleep Med Reports. 2018;4:268–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg T. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165:125–33. 10.7326/M15-2175. [DOI] [PubMed] [Google Scholar]


