Abstract
Background:
Aircraft noise may cause several non-auditory health effects, including annoyance, sleep disorders, hypertension, cardiovascular diseases, and impaired cognitive skills in children.
Objectives:
To perform a cross-sectional study among adult residents near the Orio al Serio International Airport (BGY), Italy to investigate the association between aircraft noise, annoyance, sleep disorders, blood pressure levels, and prevalence of hypertension.
Methods:
Residential addresses of subjects aged 45-70 years were geocoded and classified in three groups according to noise levels: <60 (Reference), 60-65 (Zone A), and 65-75 dBA (Zone B). A sample of subjects was invited to undergo a personal interview and blood pressure measurements. Multiple linear and robust Poisson regression models were used to analyze quantitative and categorical variables, respectively.
Results:
Between June and September 2013, we enrolled 400 subjects (166 in the Reference Zone, 164 in Zone A, and 70 in Zone B). Compared to the Reference Zone, we found elevated adjusted annoyance scores (day and night) in Zone A (+2.7) and Zone B (+4.0) (p<0.001) and about doubled proportions of severely annoyed subjects (p<0.001). Reported sleep disorders in the previous month were also more frequent in Zones A and B. Sleep disorders in general were 19.9% in the Reference Zone, 29.9% in Zone A, and 35.7% in Zone B (p<0.001).
Conclusions:
We found a strong association between aircraft noise levels, annoyance, and sleep disorders among adult residents near the Orio al Serio International Airport. We found no relationship with blood pressure levels and prevalence of hypertension.
Key words: Aircraft noise, blood pressure, annoyance, sleep disorders
Abstract
«Effetti del rumore aeroportuale su annoyance, disturbi del sonno e pressione arteriosa tra gli adulti residenti nelle vicinanze dell’Aeroporto Internazionale di Orio al Serio (BGY), Italia».
Introduzione:
Il rumore aeroportuale può causare effetti extra-uditivi quali annoyance, disturbi del sonno, ipertensione, patologie cardiovascolari e alterazioni delle abilità cognitive nei bambini.
Obiettivi:
Condurre un’indagine trasversale tra gli adulti residenti in prossimità dell’Aeroporto Internazionale di Orio al Serio (BGY), per studiare l’associazione tra rumore aeroportuale, annoyance, disturbi del sonno, pressione arteriosa e ipertensione.
Metodi:
Soggetti di età 45-70 anni sono stati suddivisi, sulla base della residenza, in tre zone acustiche di rumore aeroportuale: <60 (Riferimento), 60-65 (Zona A) e 65-75 dBA (Zona B). Un campione di soggetti è stato invitato a sottoporsi a intervista e misurazioni della pressione arteriosa. Per analizzare variabili quantitative e categoriche, sono stati utilizzati modelli di regressione lineare multipla e di Poisson robusta, rispettivamente.
Risultati:
Tra giugno e settembre 2013 sono stati reclutati 400 soggetti (166 nella Zona di Riferimento, 164 nella Zona A e 70 nella Zona B). Rispetto al riferimento, sono stati rilevati elevati punteggi di annoyance (diurni e notturni) nelle Zone A (+2,7) e B (+4,0) (p<0,001) e circa il doppio di soggetti fortemente infastiditi in entrambe le zone (p<0,001). Anche i disturbi del sonno riferiti nel mese precedente erano più frequenti nelle Zone A e B. I disturbi del sonno considerati complessivamente corrispondevano a 19,9% nella Zona di Riferimento, 29,9% nella Zona A e 35,7% nella Zona B (p<0,001).
Conclusioni:
È stata evidenziata una forte associazione tra rumore aeroportuale, annoyance e disturbi del sonno. Non è stata riscontrata alcuna relazione con i livelli di pressione arteriosa e la prevalenza di ipertensione.
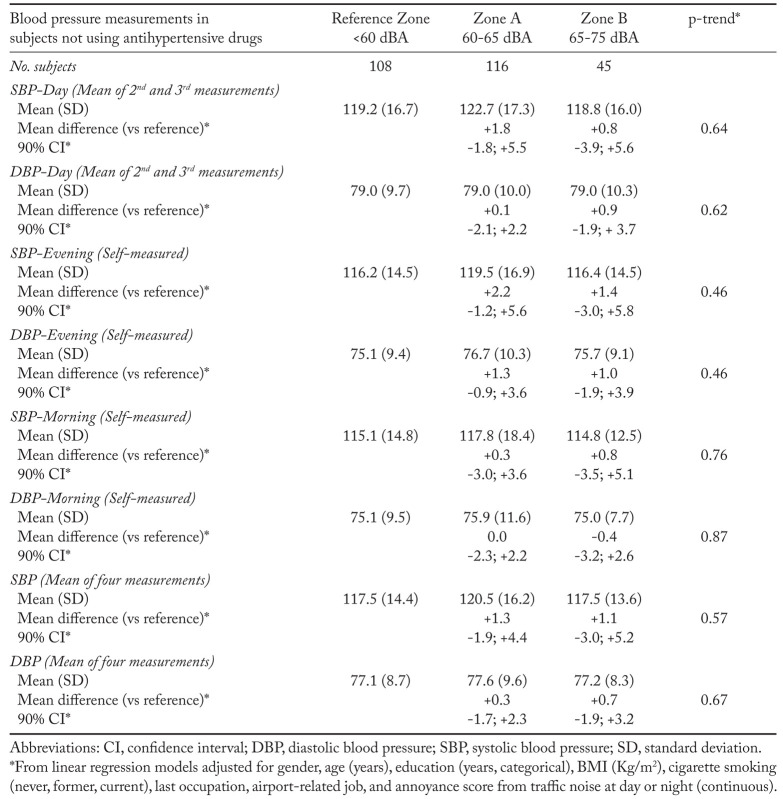
Supplementary Table 1.
Systolic and diastolic blood pressure (SBP, DBP) mean values (mmHg), by acoustic zone, in subjects not using antihypertensive drugs, Orio al Serio International Airport (BGY), Italy - June-September 2013
Introduction
Noise pollution is an important and increasing problem in modern society. The major source of environmental noise is road traffic, with estimated 100 million people in Europe living in areas with noise levels above 55 dB (as Lden: annual average day, evening and night exposure); railways, aircraft, and industrial noise levels above 55 dB are estimated to affect about 19, 4.1, and 1.0 million people, respectively (https://goo.gl/qAAooi).
The main source of noise around airports is represented by aircrafts, especially during take-off and landing operations, even if other airport activities may influence noise levels. Moreover, the presence of an airport indirectly determines an increase of noise from traffic. Several studies documented non-auditory health effects of aircraft noise (5), including annoyance (4, 17-19), sleep disorders or anxiolytic/hypnotic drug consumption (10, 11, 16, 19), hypertension (14, 15, 20), cardiovascular diseases (including myocardial infarction and stroke) (3, 9), and a variety of other effects (19). Several studies focused on children also found adverse health effects, including annoyance and impairment of cognitive skills (memory and reading ability) (6, 7, 12, 13, 22, 24).
In Italy, the large cross-sectional study SERA (Studio sugli Effetti del Rumore Aeroportuale, Study on the Effects of Aircraft Noise) in the period 2010-2012 estimated the effects of aircraft noise on annoyance, sleep disorders, and hypertension in a sample of adults residing near six airports (Rome Ciampino, Milan Malpensa, Milan Linate, Pisa San Giusto, Turin Caselle, and Venice Marco Polo) (21) and assessed the health burden (as regard those outcomes and myocardial infarction as well) attributable to noise (1, 2).
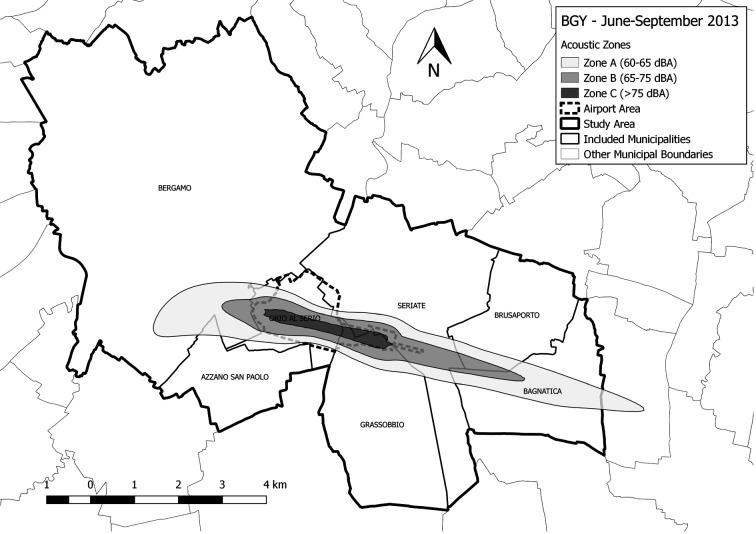
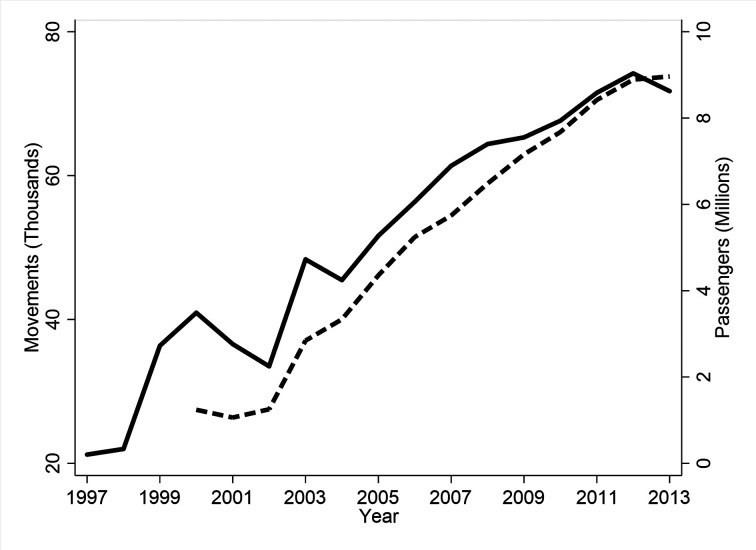
The Orio al Serio International Airport (IATA code: BGY) is located in the municipality of Orio al Serio, province of Bergamo, Lombardy, North-West Italy (figure 1). Built in the ‘70s, it has been operating as a charter airport until the ‘90s. In 2003, low-cost travel companies started operating within it and a huge increase in the number of passengers and movements occurred in the following years (figure 2). In the last years, it ranked among the first five Italian airports for number of movements and it is now the leading airport for low-cost travels. In this paper, we present the results of a cross-sectional study performed in the period June-September 2013 among adults living near BGY, to investigate the effects of aircraft noise on annoyance, sleep disorders, blood pressure levels, and hypertension, using methods and instruments similar to those used in the SERA study.
Figure 1.
Study area, Orio al Serio International Airport (BGY), Italy - June-September 2013
Figure 2.
Number of movements (solid line) and passengers (dashed line), Orio al Serio International Airport (BGY), Italy - 1997-2013. Source: Associazione Italiana Gestori Aeroporti (Assaeroporti), www.assaeroporti.it
Methods
The study was performed in the summer season, when aircraft traffic is the highest, to maximize the likelihood of uncovering adverse health effects. We followed the same protocol applied in the SERA project, which in turn was similar to the one of the European HYENA project (Hypertension and Exposure to Noise near Airports) (15). In particular, we used the same questionnaire, database, and type of sphygmomanometers, and followed a similar statistical analysis plan. Our approach differed only for the exposure assessment criteria, for which we relied on data from the regional environmental protection agency (ARPA Lombardia, see below). The study was approved by the Institutional Review Board of the local health authority (ATS Bergamo).
Sampling of subjects
The study area included seven municipalities: Azzano San Paolo, Bagnatica, Bergamo, Brusaporto, Grassobbio, Orio al Serio, Seriate (figure 1). Residential addresses of subjects aged 45-70 years were geocoded and classified in three groups according to noise levels (as LVA, Livello di Valutazione del Rumore Aeroportuale, a method to measure aircraft noise issued by the Italian Ministry of the Environment, DM 31/10/1997): Reference Zone (<60 dBA), 57,571 subjects; Zone A (60-65 dBA), 1,695 subjects; Zone B (65-75 dBA), 130 subjects. No subjects lived in Zone C (>75 dBA), where only airport-related activities are allowed. Aiming to enroll 400 subjects in total, we sampled 751 subjects: 346 in the Reference Zone, 295 in Zone A, and 110 in Zone B. Maps of noise levels were made available by ARPA Lombardia.
Subjects’ tracing and study procedures
The start of the study was announced through newspaper, radio, and TV news. Mayors of the seven municipalities were informed. Family physicians were also involved to inform and sometimes contact their patients. Subjects were sent a letter and a follow-up phone call was made to ask for participation. People willing to participate signed an informed consent and underwent a personal interview. The questionnaire contained sections on demographics, clinical history, drug use, annoyance, sleep disorders, and noise exposure from different sources. Interviews were performed by 16 interviewers (trained during two meetings) and lasted on average 45-60 minutes. The interviewers also measured blood pressure (BP) thrice, as follows: 1) before beginning the interview, after a five-minute rest; 2) before beginning the interview, after an additional one-minute rest; 3) at the end of the interview. Once the interview was concluded, the sphygmomanometer and a form to be filled were handed to the participant, with the instruction to measure BP two other times: 1) at evening, between 7 and 9 p.m., before dinner; 2) the day after at awakening, before breakfast.
Statistical analysis
Study outcomes were: annoyance, sleep quality, systolic and diastolic BP (SBP, DBP), and hypertension. Annoyance (at day and night) from several sources (including airport-related activities, motor vehicles, railway, industrial and commercial activities) was measured by an analogic scale ranging from 0 (no annoyance) to 10 (maximum annoyance). It was used either as a quantitative discrete or as a dichotomous variable (with a cutoff value ≥8, corresponding to “very annoyed”) (15). Sleep quality was considered both generally and specifically during the month preceding the interview. We analyzed four SBP and DBP measurements: 1) the average of second and third measurements performed by the interviewer (the first one was discarded); 2) evening self-measurements; 3) morning self-measurement; 4) average of all four measurements. Hypertension was defined in two ways: 1) SBP (mean of four measurements) ≥140 mmHg or DBP (mean of four measurements) ≥90 mmHg (World Health Organization [WHO] definition); 2) Either BP level above the WHO cutoff values or a diagnosis of hypertension (by a physician), together with antihypertensive medication use (HYENA/SERA definition).
Quantitative variables were analyzed using multivariable linear regression models. Dichotomous variables were analyzed using multivariable Poisson regression models with robust standard error to calculate prevalence ratios (25). We calculated 90% confidence intervals (CI) (8). Adjustment covariates were: gender, age (years), education (categorical, <6, 6-9, 10-13, 14+ years), BMI (Kg/m2), cigarette smoking (never, former, current), last occupation, airport-related job, and annoyance score (day) from traffic noise (continuous). Analyses on BP levels were initially stratified by and subsequently adjusted for anti-hypertensive drug use. In supplementary analyses for BP measurements and hypertension, we additionally adjusted for cardiac frequency and/or interviewer (N=16). Moreover, we performed supplementary analyses of the association between BP/hypertension and noise in which we used annoyance score (day or night, when relevant) from airport-related activities (continuous variable) as a subjective surrogate of aircraft-noise exposure, rather than using the actual acoustic zone. Statistical analyses were performed with Stata 14 (23).
Results
Subjects’ tracing and participation
Out of 346, 295, and 110 subjects that were randomly sampled in the <60, 60-65, and 65-75 dBA zones, respectively, we found 320 (92.5%), 275 (93.2%), and 100 (90.9%) subjects eligible for the study (table 1). Exclusions (N=56 in total) were due to lack of tracing (N=28), death (N=2), and non-eligibility for health problems or language difficulties (N=26). Participation showed a gradient according to acoustic zone: 166 in the Reference Zone (51.9% of the 320 eligible), 164 in Zone A (59.6% of the 275 eligible), and 70 in Zone B (70% of the 100 eligible).
Table 1.
Subjects’ participation by acoustic zone, Orio al Serio International Airport (BGY), Italy - June-September 2013
| Reference Zone <60 dBA | Zone A 60-65 dBA | Zone B 65-75 dBA | p* | ||||
| N | % | N | % | N | % | ||
| Population | |||||||
| (age 45-70 years) | 57,571 | 1,695 | 100 | 130 | |||
| Sampled | 346 | 100 | 295 | 100 | 110 | 100 | 0.06 |
| Not traced | 15 | 4.3 | 10 | 3.4 | 3 | 2.7 | |
| Dead | 1 | 0.3 | 1 | 0.3 | 0 | 0.0 | |
| Non-eligible** | 10 | 2.9 | 9 | 3.0 | 7 | 6.4 | |
| Refusals | 154 | 44.5 | 111 | 37.6 | 30 | 27.3 | |
| Enrolled | 166 | 48.0 | 164 | 55.6 | 70 | 63.6 | |
| Eligible | 320 | 100 | 275 | 100 | 100 | 100 | 0.004 |
| Refusals | 154 | 48.1 | 111 | 40.4 | 30 | 30.0 | |
| Enrolled | 166 | 51.9 | 164 | 59.6 | 70 | 70.0 | |
*From chi-square test
**Because of health problems or language difficulties
Characteristics of the participants
The majority of subjects in Zone B were residing in the municipalities of Seriate and Orio al Serio, while those in Zone A were living in Orio al Serio, Bergamo, and Grassobbio (table 2). Gender, education, and smoking distributions showed slight differences across the three acoustic zones. Subjects in Zone A were on average slightly older, while BMI was higher in Zone B residents. Zones A and B had a lower proportion of white collars (<15%) and higher proportions of unemployed/housewives and retired subjects (>50%). The percentage of subjects employed in airport-related occupations was overall low. Subjects were long-time residents in all zones (more than 90% being living in the current house for at least 5 years), while house type differed across zones. More subjects in Zones A and B reported they had performed structural interventions (such as creation of dead-air spaces, window change, or ceiling isolation) to reduce noise within the house (>30%), and had been avoiding spending time outdoor because of aircraft noise (>40%).
Table 2.
Characteristics of participants by acoustic zone, Orio al Serio International Airport (BGY), Italy - June-September 2013
| Reference Zone <60 dBA | Zone A 60-65 dBA | Zone B 65-75 dBA | p* | ||||
| N/Mean | %/SD | N/Mean | %/SD | N/Mean | %/SD | ||
| Interviewed | 166 | 100 | 164 | 100 | 70 | 100 | |
| Municipality | |||||||
| Azzano San Paolo | 33 | 19.9 | 7 | 4.3 | 0 | 0.0 | <0.001 |
| Bagnatica | 24 | 14.5 | 13 | 7.9 | 2 | 2.9 | |
| Bergamo | 18 | 10.8 | 45 | 27.4 | 1 | 1.4 | |
| Brusaporto | 12 | 7.2 | 0 | 0.0 | 0 | 0.0 | |
| Grassobbio | 22 | 13.2 | 41 | 25.0 | 3 | 4.3 | |
| Orio al Serio | 31 | 18.7 | 50 | 30.5 | 22 | 31.4 | |
| Seriate | 26 | 15.7 | 8 | 4.9 | 42 | 60.0 | |
| Gender | |||||||
| Male | 86 | 51.8 | 87 | 53.0 | 31 | 44.3 | 0.45 |
| Female | 80 | 48.2 | 77 | 47.0 | 39 | 55.7 | |
| Age (years) | 56.8 | 7.2 | 58.8 | 7.2 | 56.0 | 7.7 | 0.01 |
| BMI (kg/m2) | 24.8 | 3.9 | 25.2 | 4.5 | 26.1 | 4.1 | 0.07 |
| Education (years) | |||||||
| <6 | 24 | 14.5 | 37 | 22.6 | 18 | 25.7 | 0.40 |
| 6-9 | 55 | 33.1 | 53 | 32.3 | 25 | 35.7 | |
| 10-13 | 61 | 36.7 | 48 | 29.3 | 16 | 22.9 | |
| 14+ | 25 | 15.1 | 25 | 15.2 | 10 | 14.3 | |
| Missing | 1 | 0.6 | 1 | 0.6 | 1 | 1.4 | |
| Cigarette smoking | |||||||
| Never | 73 | 44.0 | 73 | 44.5 | 28 | 40.0 | 0.59 |
| Former | 54 | 32.5 | 56 | 34.2 | 20 | 28.6 | |
| Current | 39 | 23.5 | 35 | 21.3 | 22 | 31.4 | |
| Last occupation | |||||||
| Director/entrepreneur | 19 | 11.4 | 11 | 6.7 | 5 | 7.1 | 0.05 |
| Self-employed | 23 | 13.9 | 17 | 10.4 | 7 | 10.0 | |
| White collar | 40 | 24.1 | 24 | 14.6 | 8 | 11.4 | |
| Blue collar | 14 | 8.4 | 16 | 9.8 | 12 | 17.1 | |
| None/housewife | 21 | 12.7 | 27 | 16.5 | 16 | 22.9 | |
| Retired | 48 | 28.9 | 67 | 40.8 | 22 | 31.4 | |
| Other/Missing | 1 | 0.6 | 2 | 1.2 | 0 | 0.0 | |
| Airport-related job | 8 | 4.8 | 7 | 4.3 | 6 | 8.6 | 0.38 |
| Years lived in the current house | 22.1 | 14.7 | 25.4 | 15.7 | 28.0 | 15.7 | 0.01 |
| Lived in the current house for at least 5 yrs House type | 155 | 93.4 | 151 | 92.0 | 69 | 99.0 | 0.17 |
| Villa | 94 | 56.6 | 68 | 41.5 | 53 | 75.7 | <0.001 |
| Apartment | 71 | 42.8 | 96 | 58.5 | 17 | 24.3 | |
| Missing | 1 | 0.6 | |||||
| Performed structural interventions to reduce noise | 41 | 24.7 | 53 | 32.3 | 29 | 41.4 | 0.07 |
| Avoid staying outdoor | 46 | 27.7 | 70 | 42.7 | 28 | 40.0 | 0.01 |
Abbreviations: BMI, body mass index; SD, standard deviation
*From chi-squared (categorical variables) or Kruskal-Wallis (quantitative variables) test
Annoyance from airport-related activities and other sources
Subjects in Zone A reported a higher annoyance score from road traffic (mean scores: 3.5 during the day and 2.7 at night) than in the Reference Zone (2.3 and 1.8) and in Zone B (2.8 and 1.9) (p<0.001 during the day and p=0.02 at night, from Kruskal-Wallis test). Subjects in the Reference Zone reported an annoyance score during the day from neighbourhood (mean 1.5) that was higher than in Zones A (1.2) and B (0.9) (p=0.03 from Kruskal-Wallis test). Annoyance from various activities (e.g., building and road maintenance) during daytime was higher in the Reference Zone (mean 2.5) and in Zone A (2.8) in comparison with Zone B (0.9) (p=0.004 from Kruskal-Wallis test). Annoyance from other sources (train, industries, shops and restaurants) did not differ across zones.
Average levels of annoyance (either at day or night) from airport-related activities were higher (>5) than those from other sources and showed a clear trend across acoustic zones in either univariate or multiple regression analyses (table 3); in particular, adjusted mean annoyance scores exceeded by 2.7 (Zone A) and 3.5 (Zone B) units those in the Reference Zone. Severe annoyance (score ≥8) affected one third of subjects in the Reference Zone, about two-thirds in Zone A, and about 80% in Zone B, with adjusted prevalence ratios close to 2 in Zone A and about 2.5 in Zone B.
Table 3.
Annoyance from airport-related activities by acoustic zone, Orio al Serio International Airport (BGY), Italy - June-September 2013
| Annoyance from airport-related activities | Reference Zone <60 dBA | Zone A 60-65 dBA | Zone B 65-75 dBA | p-trend* |
| No. subjects | 166 | 164 | 70 | |
| Annoyance-Day | ||||
| Mean score (SD) | 5.1 (3.5) | 8.1 (2.7) | 8.5 (2.2) | |
| Mean difference (vs reference)* | +2.7 | +3.5 | <0.001 | |
| 90% CI* | +2.1; +3.2 | +2.8; +4.2 | ||
| Annoyance-Night | ||||
| Mean score (SD) | 4.7 (3.9) | 7.8 (2.9) | 8.7 (2.3) | |
| Mean difference (vs reference)* | +2.8 | +4.0 | <0.001 | |
| 90% CI* | +2.2; +3.4 | +3.2; +4.7 | ||
| Annoyance-Day (Score ≥8) | ||||
| N (%) | 55 (33.1) | 116 (70.7) | 56 (80.0) | |
| Prevalence ratio* | 1.92 | 2.40 | <0.001 | |
| 90% CI* | 1.57; 2.35 | 1.95; 2.97 | ||
| Annoyance-Night (Score ≥8) | ||||
| N (%) | 51 (30.7) | 110 (67.1) | 55 (78.6) | |
| Prevalence ratio* | 1.97 | 2.51 | <0.001 | |
| 90% CI* | 1.59; 2.44 | 2.02; 3.11 |
Abbreviations: CI, confidence interval; SD, standard deviation
*From linear (annoyance score) or robust Poisson (annoyance score ≥8) regression models adjusted for gender, age (years), education (years, categorical), BMI (Kg/m2), cigarette smoking (never, former, current), last occupation, airport-related job, and annoyance score from traffic noise at day or night (continuous)
Sleep disorders
Compared to referents, subjects in Zones A and B reported a greater frequency of sleep disorders in the month before the interview, including: long time to fall asleep, early morning awakening, insufficient sleep duration, and poor sleep quality, with positive trends across acoustic zones (table 4). Subjects in Zones A and B also reported an increased prevalence of sleep disorders in general, while hypnotic drug consumption was around 10% and did not differ across zones.
Table 4.
Sleep disorders by acoustic zone, Orio al Serio International Airport (BGY), Italy - June-September 2013
| Sleep disorders | Reference Zone <60 dBA | Zone A 60-65 dBA | Zone B 65-75 dBA | p-trend* |
| No. subjects | 166 | 164 | 70 | |
| Long time to fall asleep (Last month) | ||||
| N (%) | 22 (13.2) | 36 (22.0) | 16 (22.9) | |
| Prevalence ratio* | 1.43 | 1.67 | 0.07 | |
| 90% CI* | 0.96; 2.13 | 1.01; 2.77 | ||
| Frequent nocturnal awakening (Last month) | ||||
| N (%) | 67 (40.4) | 75 (45.7) | 30 (42.9) | |
| Prevalence ratio* | 1.02 | 0.99 | 0.99 | |
| 90% CI* | 0.82; 1.26 | 0.75; 1.32 | ||
| Early morning awakening (Last month) | ||||
| N (%) | 60 (36.1) | 64 (39.0) | 34 (48.6) | |
| Prevalence ratio* | 1.04 | 1.43 | 0.07 | |
| 90% CI* | 0.81; 1.32 | 1.08; 1.88 | ||
| Insufficient sleep duration (Last month) | ||||
| N (%) | 26 (15.7) | 42 (25.6) | 28 (40.0) | |
| Prevalence ratio* | 1.54 | 2.85 | <0.001 | |
| 90% CI* | 1.07; 2.23 | 1.90; 4.26 | ||
| Poor sleep quality (Last month) | ||||
| N (%) | 45 (27.1) | 62 (37.8) | 30 (42.9) | |
| Prevalence ratio* | 1.26 | 1.55 | 0.02 | |
| 90% CI* | 0.97; 1.64 | 1.13; 2.14 | ||
| Sleep disorders in general | ||||
| N (%) | 32 (19.3) | 49 (29.9) | 25 (35.7) | |
| Prevalence ratio* | 1.34 | 1.82 | 0.01 | |
| 90% CI* | 0.97; 1.85 | 1.25; 2.66 | ||
| Regular hypnotic drug consumption | ||||
| N (%) | 16 (9.6) | 20 (12.2) | 6 (8.6) | |
| Prevalence ratio* | 1.02 | 0.70 | 0.54 | |
| 90% CI* | 0.59; 1.74 | 0.30; 1.63 |
Abbreviations: CI, confidence interval
* From robust Poisson regression models adjusted for gender, age (years), education (years, categorical), BMI (Kg/m2), cigarette smoking (never, former, current), last occupation, airport-related job, and annoyance score from traffic noise at night (continuous)
Blood pressure levels and hypertension
We found no evidence of differences in systolic or diastolic blood pressure levels across zones, whether measured by the interviewers or by the participants themselves. Prevalence of hypertension did not differ across zones (table 5). To take into account possible differences in blood pressure measurement conditions, we performed some sensitivity analyses (not shown), in details: i) we additionally adjusted for cardiac frequency recorded at the same time of each BP measurement, and results were virtually unchanged; ii) we found similar findings after stratifying by antihypertensive drug use (Supplementary table 1 reports analyses restricted to subjects not using antihypertensive drugs); iii) we found no association between blood pressure and annoyance levels from airport-related activities (used as a surrogate of aircraft-noise exposure).
Table 5.
Systolic and diastolic blood pressure (SBP, DBP) mean values (mmHg) and prevalence of hypertension according to WHO and HYENA study, by acoustic zone, Orio al Serio International Airport (BGY), Italy - June-September 2013
| Blood pressure measurements and prevalence of hypertension | Reference Zone <60 dBA | Zone A 60-65 dBA | Zone B 65-75 dBA | p-trend* |
| No. subjects | 166 | 164 | 70 | |
| SBP-Day (Mean of 2nd and 3rd measurements) | ||||
| Mean (SD) | 121.9 (16.5) | 122.8 (16.7) | 120.3 (16.8) | |
| Mean difference (vs reference)* | +0.2 | -0.2 | 0.96 | |
| 90% CI* | -2.7; +3.2 | -4.1; +3.6 | ||
| DBP-Day (Mean of 2nd and 3rd measurements) | ||||
| Mean (SD) | 79.7 (9.9) | 78.5 (9.4) | 79.5 (10.6) | |
| Mean difference (vs reference)* | -0.9 | +0.4 | 0.99 | |
| 90% CI* | -2.6; +0.9 | -1.9; + 2.7 | ||
| SBP-Evening (Self-measured) | ||||
| Mean (SD) | 118.0 (14.3) | 120.2 (15.9) | 117.6 (14.2) | |
| Mean difference (vs reference)* | +1.7 | +0.2 | 0.71 | |
| 90% CI* | -1.0; +4.4 | -3.3; +3.6 | ||
| DBP-Evening (Self-measured) | ||||
| Mean (SD) | 75.6 (9.3) | 76.0 (10.0) | 75.2 (8.6) | |
| Mean difference (vs reference)* | +0.6 | 0.0 | 0.86 | |
| 90% CI* | -1.1; +2.4 | -2.3; +2.3 | ||
| SBP-Morning (Self-measured) | ||||
| Mean (SD) | 118.5 (15.1) | 120.7 (18.5) | 118.1 (13.8) | |
| Mean difference (vs reference)* | +1.3 | -0.2 | 0.90 | |
| 90% CI* | -1.5; +4.0 | -3.8; +3.3 | ||
| DBP-Morning (Self-measured) | ||||
| Mean (SD) | 76.3 (10.0) | 76.4 (11.2) | 76.5 (8.5) | |
| Mean difference (vs reference)* | 0.0 | -0.4 | 0.81 | |
| 90% CI* | -1.9; +1.8 | -2.8; +2.0 | ||
| SBP (Mean of four measurements) | ||||
| Mean (SD) | 120.2 (14.1) | 121.5 (15.5) | 119.2 (13.3) | |
| Mean difference (vs reference)* | +0.7 | -0.1 | 0.92 | |
| 90% CI* | -1.8; +3.2 | -3.3; +3.2 | ||
| DBP (Mean of four measurements) | ||||
| Mean (SD) | 77.9 (8.7) | 77.3 (8.9) | 77.7 (8.0) | |
| Mean difference (vs reference)* | -0.3 | +0.1 | 0.99 | |
| 90% CI* | -1.8; +1.3 | -1.9; +2.1 | ||
| Hypertension (WHO definition**) | ||||
| N (%) | 21 (12.6) | 21 (12.8) | 7 (10.0) | |
| Prevalence ratio* | 0.94 | 0.74 | 0.51 | |
| 90% CI* | 0.60; 1.50 | 0.36; 1.51 | ||
| Hypertension (HYENA study definition***) | ||||
| N (%) | 61 (36.8) | 56 (34.1) | 29 (41.4) | |
| Prevalence ratio* | 0.86 | 1.04 | 0.91 | |
| 90% CI* | 0.68; 1.10 | 0.77; 1.39 |
Abbreviations: CI, confidence interval; DBP, diastolic blood pressure; HYENA, Hypertension and Exposure to Noise near Airports; SBP, systolic blood pressure; SD, standard deviation; WHO, World Health Organisation.
*From linear (blood pressure measurements) or robust Poisson (hypertension) regression models adjusted for gender, age (years), education (years, categorical), BMI (Kg/m2), cigarette smoking (never, former, current), last occupation, airport-related job, use of antihypertensive drugs, and annoyance score from traffic noise at day or night (continuous).
**SBP (mean of four measurements) ≥140 mmHg or DBP (mean of four measurements) ≥90 mm Hg.
***Either BP level above the WHO cutoff values or a diagnosis of hypertension (by a physician), together with antihypertensive medication use.
Discussion
In this study we found a clear association between noise levels over 60 dBA, annoyance, and sleep disorders among adult residents in the vicinity of the Orio al Serio International Airport. On the other hand, we found no evidence of a relationship with blood pressure levels or prevalence of hypertension.
Our findings on annoyance and sleep quality are in agreement with those found in the SERA study, where increasing frequencies of subjects with severe annoyance and sleep disorders were found alongside increasing noise levels (21). Similarly, the HYENA study had identified a clear dose-response relationship between the percentage of highly annoyed subjects and increasing aircraft noise values (4). International investigations also supported the role of aircraft noise exposure in determining sleep disturbances, even if findings were slightly less consistent across studies (10, 11).
Results on hypertension and blood pressure levels from national and international studies return a more heterogeneous picture. In SERA, average SBP was 5.1 mmHg higher in the noisiest zone among 50 subjects not in treatment with antihypertensive drugs (21). We did not find important relationships between BP and noise levels, even after restricting our analysis to subjects not using antihypertensive drugs. Noise categorization in SERA was based on Lden and five areas were used: <50 (902 subjects, reference), 50-55 (N=313), 55-60 (N=363), 60-65 (N=259), >65 dB (N=61). The >65 dB zone included subjects living near the Rome Ciampino (N=20), Milan Linate (N=23), and Turin Caselle (N=18) airports. Although our noise definition and categorization was different, we found no association in our sensitivity analysis where annoyance was used as a (potentially) finer surrogate of individual exposure. In any case, neither our investigation nor the SERA study found clear-cut evidence of increased prevalence of hypertension in the noisiest zones (21). The exposure-response relationship between aircraft noise and hypertension was indeed clearer in the HYENA study, especially when the analysis was limited to night noise levels (14, 15). As our measure of exposure (LVA) is expected to return a picture representing a 24h summary rather than a daily or nightly estimate, our results cannot be directly compared. Nonetheless, one possible explanation of the difference in our findings might be related to the lower cut-off point chosen in HYENA to define non-exposed subjects (i.e. <50 dBA), that might have produced a greater contrast between exposed subjects and the referents.
The major strength of this study is the study design, which strictly followed the protocol and used the same procedures and instruments of a European project (HYENA) and an Italian investigation (SERA) specifically designed to evaluate health effects of aircraft noise exposure. The only difference was that noise levels were classified in acoustic zones according to the LVA measures defined above, while HYENA/SERA used Lden. As we used categories rather than absolute values in our analysis of non-, mildly-, and highly-exposed subjects, we can assume this difference did not greatly influence our results, even if it might hamper a full comparability with the published literature. We were also able to enrol subjects in the period of maximum activity of the airport (June through September), which might be relevant for effects such as change in blood pressure levels, annoyance, and sleep disturbances. Finally, we managed to enrol the majority (N=70) of the 130 subjects living in the noisiest Zone B.
Our study has also limitations. Data collection was based on interviews and could thus be theoretically prone to report bias. Such distortion may hardly apply to annoyance, which indeed is a perceived disturbance, but could apply to sleep disorders. Another potential weakness is represented by the relatively low participation rate, in particular in the Reference Zone as well as in Zone A. However, we found only slight gender and age differences between participants and non-responders, both when considering all acoustic zones together and when looking within each zone.
Conclusions
In this study we found a strong association between noise levels over 60 dBA, annoyance, and sleep disorders among adult residents near the Orio al Serio International Airport. Although we found no evidence of a relationship with blood pressure levels or prevalence of hypertension, the presence of subjective disorders suggests the need of further preventive actions, including efforts to reduce aircraft noise, structural interventions in houses (where needed), and the implementation of periodical monitoring programs of residents’ health (adults and children).
No potential conflict of interest relevant to this article was reported by the authors
Acknowledgements:
We wish to thank: the study participants; the ATS personnel who performed interviews; the SERA study coordinators from the Department of Epidemiology of the Lazio Regional Health Service for sharing the study protocol, statistical plan, questionnaire, and database; Gaetano Gramano for IT assistance in implementing the database; Chiara Bettoni and Silvia Ranghetti for data input.
Funding:
This study was funded by the local health authority (ATS Bergamo, formerly ASL della Provincia di Bergamo)
References
- 1.Ancona C, Forastiere F. Noise and air pollution: the effect of airports on the health of residents. Epidemiol Prev. 2014;38:164–166. [PubMed] [Google Scholar]
- 2.Ancona C, Golini MN, Mataloni F, et al. Health impact assessment of airport noise on people living nearby six Italian airports. Epidemiol Prev. 2014;38:227–236. [PubMed] [Google Scholar]
- 3.Babisch W, Beule B, Schust M, et al. Traffic noise and risk of myocardial infarction. Epidemiology. 2005;16:33–40. doi: 10.1097/01.ede.0000147104.84424.24. [DOI] [PubMed] [Google Scholar]
- 4.Babisch W, Houthuijs D, Pershagen G, et al. Annoyance due to aircraft noise has increased over the years-results of the HYENA study. Environment international. 2009;35:1169–1176. doi: 10.1016/j.envint.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 5.Basner M, Clark C, Hansell A, et al. Aviation Noise Impacts: State of the Science. Noise & health. 2017;19:41–50. doi: 10.4103/nah.NAH_104_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clark C, Crombie R, Head J, et al. Does traffic-related air pollution explain associations of aircraft and road traffic noise exposure on children’s health and cognition? A secondary analysis of the United Kingdom sample from the RANCH project. American journal of epidemiology. 2012;176:327–337. doi: 10.1093/aje/kws012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clark C, Martin R, Van Kempen E, et al. Exposure-effect relations between aircraft and road traffic noise exposure at school and reading comprehension: the RANCH project. American journal of epidemiology. 2006;163:27–37. doi: 10.1093/aje/kwj001. [DOI] [PubMed] [Google Scholar]
- 8.Consonni D, Bertazzi PA. Health significance and statistical uncertainty. The value of P-value. La Medicina del lavoro. 2017;108:6603. doi: 10.23749/mdl.v108i5.6603. [DOI] [PubMed] [Google Scholar]
- 9.Floud S, Blangiardo M, Clark C, et al. Exposure to aircraft and road traffic noise and associations with heart disease and stroke in six European countries: a cross-sectional study. Environmental health : a global access science source. 2013;12:89. doi: 10.1186/1476-069X-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Floud S, Vigna-Taglianti F, Hansell A, et al. Medication use in relation to noise from aircraft and road traffic in six European countries: results of the HYENA study. Occupational and environmental medicine. 2011;68:518–524. doi: 10.1136/oem.2010.058586. [DOI] [PubMed] [Google Scholar]
- 11.Franssen EA, Van Wiechen CM, Nagelkerke NJ, Lebret E. Aircraft noise around a large international airport and its impact on general health and medication use. Occupational and environmental medicine. 2004;61:405–413. doi: 10.1136/oem.2002.005488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haines MM, Stansfeld SA, Job RF, et al. A follow-up study of effects of chronic aircraft noise exposure on child stress responses and cognition. Int J Epidemiol. 2001;30:839–845. doi: 10.1093/ije/30.4.839. [DOI] [PubMed] [Google Scholar]
- 13.Hygge S, Evans GW, Bullinger M. A prospective study of some effects of aircraft noise on cognitive performance in schoolchildren. Psychological science. 2002;13:469–474. doi: 10.1111/1467-9280.00483. [DOI] [PubMed] [Google Scholar]
- 14.Jarup L, Babisch W, Houthuijs D, et al. Hypertension and exposure to noise near airports: the HYENA study. Environmental health perspectives. 2008;116:329–333. doi: 10.1289/ehp.10775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jarup L, Dudley ML, Babisch W, et al. Hypertension and Exposure to Noise near Airports (HYENA): study design and noise exposure assessment. Environmental healthperspectives. 2005;113:1473–1478. doi: 10.1289/ehp.8037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Michaud DS, Fidell S, Pearsons K, et al. Review of field studies of aircraft noise-induced sleep disturbance. The Journal of the Acoustical Society of America. 2007;121:32–41. doi: 10.1121/1.2400613. [DOI] [PubMed] [Google Scholar]
- 17.Miedema HM, Oudshoorn CG. Annoyance from transportation noise: relationships with exposure metrics DNL and DENL and their confidence intervals. Environmental healthperspectives. 2001;109:409–416. doi: 10.1289/ehp.01109409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miedema HM, Vos H. Exposure-response relationships for transportation noise. The Journal of the Acoustical Society of America. 1998;104:3432–3445. doi: 10.1121/1.423927. [DOI] [PubMed] [Google Scholar]
- 19.Passchier-Vermeer W, Passchier WF. Noise exposure and public health. Environmental healthperspectives. 2000;(108 Suppl 1):123–131. doi: 10.1289/ehp.00108s1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenlund M, Berglind N, Pershagen G, et al. Increased prevalence of hypertension in a population exposed to aircraft noise. Occupational and environmental medicine. 2001;58:769–773. doi: 10.1136/oem.58.12.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.SERA Italia: Impatto dell’inquinamento ambientale prodotto dagli aeroporti sulla salute dei residenti: risultati dello studio campionario. 2012:1-49 [in Italian] avaiable at: https://goo.gl/ew7jFE . [Google Scholar]
- 22.Stansfeld SA, Berglund B, Clark C, et al. Aircraft and road traffic noise and children’s cognition and health: a cross-national study. Lancet. 2005;365:1942–1949. doi: 10.1016/S0140-6736(05)66660-3. [DOI] [PubMed] [Google Scholar]
- 23.Statacorp: Stata: Release 14. Statistical Software. College Station, TX: StataCorp LP, 2015 [Google Scholar]
- 24.Van Kempen EE, Van Kamp I, Stellato RK, et al. Children’s annoyance reactions to aircraft and road traffic noise. The Journal of the Acoustical Society of America. 2009;125:895–904. doi: 10.1121/1.3058635. [DOI] [PubMed] [Google Scholar]
- 25.Zou G. A modified poisson regression approach to prospective studies with binary data. American journal of epidemiology. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]