Abstract
Introduction
Traditionally, shift work for radiographers at our institution comprised of three shift patterns – morning (8am-2pm), afternoon (2pm–9pm) and night (9pm-8am). However, when COVID-19 was first detected in Singapore in January 2020, the 12-h shift was introduced for better team segregation and deployment to meet the service needs of the Emergency Department. The 12-h shift consisted of the day (9am-9pm) and night (9pm-9am) shifts. While the 12-h shift is common to nursing practices, it is new to the radiography profession within the study centre. This study explores the radiographers' perspectives of the new shift and the impact of shift patterns on radiographers' wellness and work performance compared to the original three shift patterns.
Methods
A mixed-methods design study was adopted for this single-centre evaluation. An anonymous online questionnaire was administered to radiographers who had experienced both shift types. Additionally, the number of radiographers who had taken sick leave, and images rejected and accepted from the X-ray consoles were retrospectively collected to measure the impact of the new shift.
Results
Radiographers experienced fatigue and appreciated the longer rest days associated with the 12-h shift. Additionally, the sick leave rates and image reject counts were more favourable with the 12-h shift pattern.
Conclusion
The findings indicate that the extended shift hours are effective during a pandemic but may result in radiographer burnout during a prolonged outbreak.
Implications for practice
Studying these variables will provide an effective starting point in understanding the efficacy and applicability of a 12-h shift system during pandemic periods.
Keywords: Radiographers, COVID-19, Shift working, Sickness absences, Image rejection rates
Introduction
Round-the-clock radiological services, such as general radiography and Computed Tomography (CT) in particular, are not peculiar to hospitals' Accident and Emergency (A&E) Departments in Singapore. Radiographers, as part of the multidisciplinary team, undergo shift work to provide care to patients in the acute setting. Until the Coronavirus disease (COVID-19) pandemic, the shift patterns for radiographers at the study centre have always comprised of three shift patterns (Table 1 a). Radiographers doing shift work would rotate between the in-patient location and A&E Department on a weekly or fortnightly basis, working with different colleagues at every rotation. However, when the disease was first detected in Singapore in January 2020, the 12-h-long shift (Table 1 b) was introduced for better team segregation and deployment to meet the service demands of the A&E Department. Radiographers providing radiological services at the in-patient location continued with the three-shift pattern and did not have any contact with suspected or confirmed COVID-19 patients. With these changes, radiographers would then remain in the same team for at least a month at their respective locations, only rotating to other locations depending on the department's operational needs. If more than 25% of the team were on sick leave simultaneously, the whole team would be replaced with a back-up team. Otherwise, no additional manpower would be provided.
Table 1a.
Three-shifts pattern showing a sample roster from Monday to Sunday.
| Three-shifts | Mon | Tue | Wed | Thu | Fri | Sat | Sun |
|---|---|---|---|---|---|---|---|
| Duty 1 | AM | AM | AM | AM | AM | OFF | NIGHT |
| Duty 2 | OFF | PM | PM | PM | NIGHT | NIGHT | OFF |
| Duty 3 | PM | OFF | NIGHT | NIGHT | OFF | AM | PM |
| Duty 4 | NIGHT | NIGHT | OFF | OFF | PM | PM | AM |
| Shift | AM | PM | NIGHT |
|---|---|---|---|
| Hours | 8am – 2pm | 2pm–9pm | 9pm – 8am |
Table 1b.
12-h shift pattern showing a sample roster from Monday to Saturday.
| 12-h shifts | Mon | Tue | Wed | Thu | Fri | Sat |
|---|---|---|---|---|---|---|
| Duty 1 | DAY | DAY | OFF | OFF | NIGHT | NIGHT |
| Duty 2 | NIGHT | NIGHT | OFF | OFF | DAY | DAY |
| Duty 3 | OFF | OFF | DAY | DAY | OFF | OFF |
| Duty 4 | OFF | OFF | NIGHT | NIGHT | OFF | OFF |
| Shift | DAY | NIGHT |
|---|---|---|
| Hours | 9am – 9pm | 9pm – 9am |
The study centre is a 1000-bed hospital located in the eastern sector of Singapore with a 6000 strong staff base. As a public hospital, it has a wide range of medical specialties serving the estimated one million adult populations in that region. The radiology department performs approximately 240,000 general radiography and 120,000 specialised examinations annually. The imaging examinations are supported by a group of 150 radiographers, 50 radiologists, 50 nurses and 50 administrative and support staff.
When Singapore confirmed its first COVID-19 case on 23 January 2020, public healthcare institutions such as the study centre were swift to identify the outbreak, drawing from previous lessons such as the Severe Acute Respiratory Syndrome (SARS)1 and avian influenza (H1N1)2 pandemic to begin implementing protocols and safety measures for patient treatment. The leadership of the department promptly initiated the escalation of responses for team segregation to ensure service continuity. As a result, the 12-h shifts were established with the department's roster committee members. The goals were to reduce contact between staff and to limit possible spread3 of coronavirus from the community or within the hospital. Concurrently, another centre in Singapore had re-organised their workforce4 for manpower deployment to areas of higher workload to meet the service needs. Other operational strategies in managing COVID-19 included dedicated imaging rooms and equipment,5 scanning of COVID-19 suspected cases in batches5 and staggering work and lunch hours4 to ensure safe distancing.
Internationally, the 12-h shifts have sparked debate amongst the nursing community, with fatigue and safety being the main concerns raised.6, 7, 8, 9 Longer working hours may have adverse fatigue-related effects on healthcare workers, with the higher rates of patient-care errors, needle-stick injuries, musculoskeletal disorders, drowsy driving, and sleep deprivation being reported.10 However, the 12-h shift system has remained popular as it allowed for lesser commuting and longer breaks, hence leading to more personal time and greater work satisfaction.8 , 11 Prior to the pandemic, radiographers in Singapore had minimal experience operating in 12-h shifts. Additionally, there is a lack of data with regard to radiographers' perspectives toward a new 12-h shift system in the current literature. Hence, the aims of this study is to (1) validate the 12-h shift system during the COVID-19 pandemic, (2) understand the perspectives of radiographers involved in COVID-19 medical imaging services whilst working the 12-h shifts, (3) understand the impact of shift patterns on sick leave rates in radiographers in the A&E and in-patient settings as well as (4) the reject analysis of images (surrogate measure of performance) of A&E radiographers.
Methods
A partially mixed concurrent equal status design was adopted to advance the understanding of the differences in radiographers' perspective and its applicability. This design included two phases of simultaneous data collection in which the quantitative and qualitative phases would weigh approximately the same.12 The results for both phases would only be integrated upon collection and interpretation of all data.
Ethics
Exemption from a full ethical review was approved from the Centralised Institutional Review Board (CIRB) as data collected from this study was considered to be a service evaluation and did not pose any anticipated risks to the study participants. Additionally, the research process would not increase the risk or burden of the radiological services beyond the usual clinical practice when managing patients.
Design
Qualitative phase: questionnaire on radiographers' shift preference
This study utilised a prospective ten-item questionnaire (Appendix A) for radiographers who had experienced working both shift patterns, evaluating their preferences using multiple-choice and open-ended questions. The qualitative questionnaire was distributed to all 48 radiographers who had worked the 12-h shifts in the A&E Department of the study centre from February to June 2020. This was because they were the only radiographers within the radiography department with experience of working the 12-h shifts and conventional three-shifts pattern prior to February 2020.
Quantitative phase: reject analysis of images acquired and sick leave
The impact of the 12-h shift was evaluated through retrospective data collection of reject analysis of images acquired in the A&E Department and radiographers' sick leave rates. The image reject rate was used as a surrogate marker of radiographer performance whilst sick leave was defined as a leave of absence granted by a certified medical practitioner because of illness.
Setting & procedure
Questionnaire on radiographers' shift preference
The questionnaire was created using an encrypted online survey platform by the Singapore government's GovTech agency and consisted of questions pertaining to census data and shift preferences, to assess the generalisability of the collected data. An epistemological assumption was integrated into the research to underpin how the 12-h shift would affect the radiographers' perspective and applicability during the COVID-19 pandemic, compared to the conventional three-shifts pattern. Face validity was established by getting a Principal Radiographer and a Statistician to read and evaluate the survey questions. Three radiographers who met the study criteria were chosen to run a pilot test of the survey. Improvements were then made following their feedback. To achieve a response rate of more than 80%, a short text message containing the questionnaire web link was sent to the 48 shortlisted radiographers by the head of department's personal assistant. The radiographers were invited to complete the voluntary, anonymous 5-min questionnaire within one week.
Reject analysis of images acquired and sick leave
The number of images that were rejected and sent to the hospital's Picture Archiving and Communications System (PACS) was collected from all X-ray consoles within the A&E Department. Only data from February to June in the years 2019 and 2020 was included in the analysis. The different year periods were deemed the non-pandemic three-shifts and the pandemic 12-h shifts respectively. Additionally, the collation of number of radiographers within the department who had been on sick leave was retrieved from the Departmental Sick Leave Management Record. Only radiographers who were working either the 12-h shift at the A&E Department or the three-shift pattern at the in-patient location from February to June 2020 were included in the analysis.
Data analysis
The responses obtained from the questionnaire, sick leave data, and image reject counts/rates were statistically analysed using the IBM SPSS version 20.0 (IBM Corp., Armonk, NY, USA), with statistical significance set at p < 0.05. Descriptive statistics, including frequencies, was employed to summarize the data from the open-ended questionnaire and grouped into overarching themes by two researchers. Additionally, the data for reject analysis of images acquired and sick leave was tabulated and presented as frequencies and proportions. Discrepancies were resolved through a consensus face-to-face discussion.
Questionnaire on radiographers' shift preference
Responses from the open-ended questionnaire were collected and analysed. Chi-square tests were performed to evaluate the association between the census data (i.e. age group, marital status), length of experience in the shift pattern, and preferred shift. Thematic analysis was conducted to identify and report reasons for the participants' shift preferences.
Reject analysis of images acquired and sick leave
The association in image reject count/rate between the pandemic (February to June 2020) and non-pandemic (February to June 2019) period was performed using Chi-square tests.
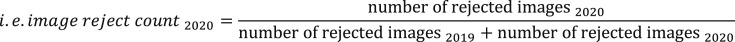
The image reject count (Fig. 1 ) for a particular period was calculated by dividing the total number of rejected images in a particular period by the total number of rejected images in both periods and presented as a percentage.
Figure 1.
Calculation for image reject count.
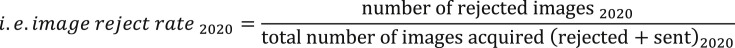
The image reject rate (Fig. 2 ) for a particular period was calculated by dividing the number of rejected images by the total number of acquired images for the same period and presented as a percentage.
Figure 2.
Calculation for image reject rate.
The number of days of sick leave taken by radiographers working at the A&E Department (12-h shifts) and the in-patient location (three-shifts pattern) were assessed using the independent t-test.
Results
Questionnaire on radiographers' shift preference
A 100% (n = 48) response rate was achieved from the A&E radiographers. The participants' demographics (Table 2 ) showed 17 (35%) male and 31 (65%) female participants of various age groups. The workforce consisted of young radiographers with only 15% of them are more than 40 years old.
Table 2.
Participants' demographics.
| n (%) | ||
|---|---|---|
| Total participants | 48 (100) | |
| Gender | Male | 17 (35) |
| Female | 31 (65) | |
| Age group | <26 years old | 3 (16) |
| 26–30 years old | 27 (56) | |
| 31–35 years old | 8 (17) | |
| 36–40 years old | 3 (6) | |
| >40 years old | 7 (15) | |
| Marital status | Married | 12 (25) |
| Single | 36 (75) | |
| Married with children | Yes | 6 (50) |
| No | 6 (50) | |
| Years of work experience | <5 years | 17 (35) |
| 5–10 years | 19 (40) | |
| >10 years | 12 (25) | |
Almost all participants (96%, n = 46) interacted with suspected COVID-19 patients, while only 83% (n = 40) had interactions with confirmed COVID-19 patients (Table 3 ). These were self-reported responses and that interaction with suspected/confirmed COVID-19 patients (nor the degree of interaction) could not be confirmed. There were mixed levels of experience working the 12-h shifts at the A&E Department, with three months being the most common duration experiencing the new shift pattern.
Table 3.
Responses to working at the A&E Department.
| n (%) | ||
|---|---|---|
| Total participants | 48 (100) | |
| Interaction with suspected COVID-19 patients | Yes | 46 (96) |
| No | 2 (4) | |
| Interaction with confirmed COVID-19 patients | Yes | 40 (83) |
| No | 8 (17) | |
| Experience with 12-h shift | 1 month | 13 (27) |
| 2 months | 3 (6) | |
| 3 months | 15 (31) | |
| 4 months | 13 (27) | |
| 5 months | 4 (8) | |
| Preferred shift | 12-h shift | 27 (56) |
| three-shift pattern | 21 (44) | |
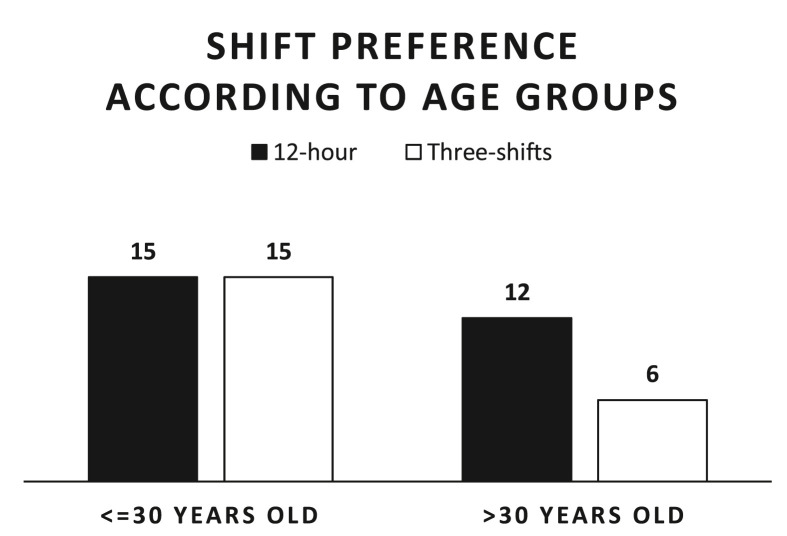
When it came to indicating their preference for shift types during the pandemic, 56% (n = 27) said they preferred the 12-h shifts, while 44% preferred the three-shifts pattern (Table 3). On further analysis, the study also found that there were equal preferences for the 12-h shifts and the three-shifts pattern amongst the younger participants, whilst 67% (n = 15) of the participants over 30 years old preferred the 12-h shifts over the three-shifts pattern (Fig. 3 ).
Figure 3.
Participants' shift preference according to age groups.
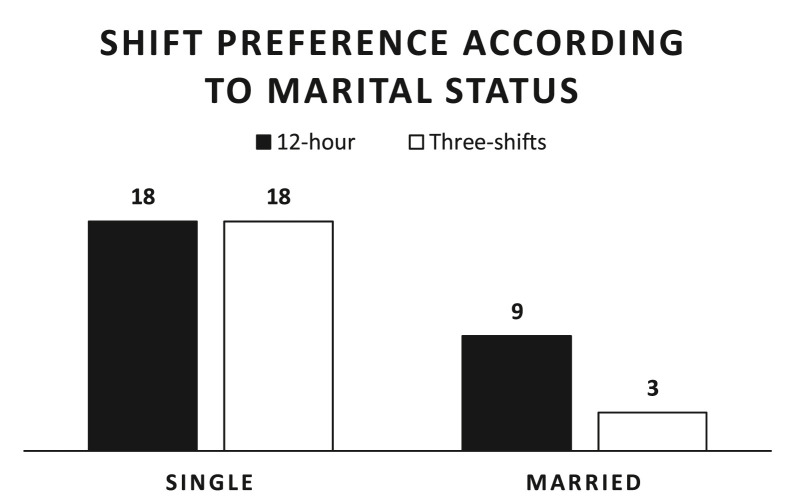
It was observed that more married participants favoured the 12-h shift, whilst the shift preferences were equivocal amongst the single participants (Fig. 4 ).
Figure 4.
Participants' shift preference according to marital status.
Participants with preference for the 12-h shift had often worked more than three months (mean = 3.07 months, SD = 1.33) in the new shift pattern. On the other hand, participants who preferred the three-shifts pattern had lesser experience (mean = 2.52 months, SD = 1.29) in the 12-h shift.
Two themes – rest days and fatigue, were derived from the responses of the open-ended question in the questionnaire. Majority of the participants reported feeling more fatigued during the 12-h shift, but favoured the shift for the increased number of rest days (p < 0.001):
“I get better rest days even though the working day can be long and tiring.” - Participant 5
“More off days and I can get sufficient rest mentally and physically.” - Participant 19
Participants who preferred the three-shifts pattern valued more time for their personal life, whilst others cited sleep pattern disruptions during their experience with the 12-h shift:
“I get more time every day with my family with the three-shifts pattern. Otherwise once I'm home, my family would already be preparing to sleep.” - Participant 32
“I prefer to have lesser working hours in a day so that I can still run my errands or continue with my exercises.” - Participant 42
“In the long run, the 12-h shift can really affect my sleeping pattern. It can be too tiring on a busy day and we may still have another 12-h shift to go on the next day.” - Participant 34
Reject analysis of images and sick leave
The total images acquired during the 2019 non-pandemic three-shifts period was 17% (81,227 vs 69,050) more than during the 2020 pandemic 12-h shifts period (Table 4 ). Comparing the image reject count, the year 2019 had significantly more (p < 0.001) rejected images than in 2020, with a similar trend observed in the image acceptance count as well. The image reject rate was 0.9% (9.1% vs 8.2%) higher in 2020 during the pandemic, than in 2019 when there was no pandemic, but was not statistically significant.
Table 4.
Statistics of images acquired during the 2019 non-pandemic three-shifts and 2020 pandemic 12-h shifts period in the A&E Department.
| 2019 | 2020 | Total | ||
|---|---|---|---|---|
| Rejected images | Count | 6666 | 6310 | 12,976 |
| Image reject count (%) | 51.4 | 48.6∗ | 100 | |
| Image reject rate (%) | 8.2 | 9.1 | 8.6 | |
| Accepted images | Count | 74,561 | 62,740 | 137,301 |
| Image accept count (%) | 54.3 | 45.7 | 100 | |
| Image accept rate (%) | 91.8 | 90.9 | 91.4 | |
| Total | Count | 81,227 | 69,050 | 150,277 |
| Image total count (%) | 54.1 | 45.9 | 100 | |
∗p < 0.001.
The average number of days of sick leave taken by radiographers working the 12-h shift at the A&E Department was 3.33 (SD = 2.88) days compared to 4.60 (SD = 3.88) days in radiographers working the three-shifts pattern at the in-patient location. This data was not statistically significant.
Discussion
The COVID-19 pandemic has highlighted the importance of timely response in operational strategies to ensure the continuity of services in all healthcare institutions. To date, this is the first study that strives to understand the radiography viewpoint of implementing a new shift pattern in the midst of a healthcare crisis. Being part of the hospital's frontline medical team, radiographers are critical in providing for timely radiological services. One approach to ensure service sustainability was the implementation of the 12-h shift for radiographers working in the A&E Department, providing for 24-h round-the-clock medical imaging services.
In the already strained workforce, who required additional processes and more stringent infection control measures dealing with the pandemic, the 12-h shift implementation did not necessarily reduce the manpower requirements. However, it provided two very distinct advantages to the department. Firstly, the 12-h shift facilitated clear team segregation due to its fixed shift patterns (i.e. a day and a night shift), hence resulting in limited to no interaction between the teams. Secondly, the 12-h shift enabled the activation of a back-up team in the event that one team was required to be quarantined due to unprotected exposure to the coronavirus.
Despite more female radiographers working the 12-h shift, the teams were an accurate and exact representation13 of the female to male radiographer ratio in Singapore. A systematic review done by Wagstaff and Sigstad Lie on shift work and long working hours showed that no particular gender would be more susceptible to or protected against the effects of work durations on risks of errors in the workplace.14 This study found that most radiographers older than 30 years or who were married with children preferred the 12-h shifts. Conversely, some radiographers preferred the three-shifts pattern because it allowed for more family-time. These differences in shift preferences were echoed by a Canadian study on radiation therapists undergoing the 12-h shift.15 It was discussed in the study that the daily care for dependent children and elderly parents may not be suitable for either shift work arrangement, depending on whether the radiation therapists had extra help from family or spouses at home. The consensus from both shift preferences was the desire for more or longer rest days, considering what was more worthwhile – extra total days off or extra rest time per day respectively. Nevertheless, rest days to overcome fatigue is an important factor in achieving good work-life balance, with this study sharing the same sentiments as others in literature.15 , 16
Radiographers with more than three months of experience working at the A&E Department were more likely to prefer the 12-h shift. A similar study of critical care nurses in Scotland undergoing the 12-h shift,17 explained that the benefits of such shift work include greater flexibility, lesser travel, and more time with family. Unlike the nursing profession where extensive handovers are required at each change of shift, handover processes for radiographers are often minimal. As such, radiographers are less likely to remain at work beyond their appointed shift hours.
Although there was a consensus of the 12-h shift being complemented with more rest days, several felt that it was more physically tiring and mentally draining in the long term despite the younger workforce within the team. Another centre in Singapore reported that the 12-h shift pattern is sustainable and provided fixed work–rest cycle.4 However, the ratio of staffing based on daily workload was higher (8 radiographers for general radiography alone versus 8 radiographers for general radiography, Computed Tomography services and image commenting in our study centre).
The 12-h shift is longer compared to the conventional three-shifts, with the peak hours for the A&E Department occurring during the day shift (surge of patients during the 10th to 20th hour of the day according to a 2017 study18). Hence, radiographers on the 12-h day shift were more likely to experience fatigue, compared to the three-shifts pattern where the peak hours were spread between the morning (8am-2pm) and afternoon (2pm–9pm) shifts. Inevitably, radiographers would then welcome more rest days to recuperate from their physical and mental exhaustion.
The novelty of this study is that radiographer-specific error rates and health statuses are evaluated with the implementation of this new shift pattern. Systematic review found no other studies investigating how changes in shift work impact radiography errors.19 We hope that findings from this study will assist to guide workflow and staffing optimisation interventions to ensure safe and effective care delivery. The reject analysis of images acquired and sick leave days were used as variables to measure the outcome of the 12-h shift.
The image reject rates were used as a surrogate marker to radiographers' performance. In 2020, there was an overall decrease in caseload, most likely occurred due to implementation of the COVID-19 (Temporary Measures) Act 2020 by the Singapore Parliament, thereby limiting the public's movement around the country unless for important valid reasons, such as seeking medical treatment, doing essential work, exercising and obtaining essential goods.20 With these restrictions, patients were more likely to present to the A&E Department only in the event of serious emergencies or if they had come into contact with patients who were suspected or confirmed of having COVID-19. As such, the radiographic projections for many of the severely ill patients may be technically challenging, resulting in higher image reject rate in 2020 than 2019 (9.1% vs 8.2%). Another possible reason for the increase in image rejection rate could be that radiographers were more fatigued during the longer 12-h shift, resulting in loss of concentration. Other studies have also reported a drop in staff performance with longer shift hours resulting in a loss of focus, a sign of burnout.14 , 27 If the 12-h shift is still necessary in a prolonged pandemic period, departments may consider arranging their staff to have staggered short breaks during the shift to combat burnout.28 , 29 Additionally, chest radiographs, the most common radiological investigation for COVID-1924 in the A&E setting, are simpler to perform than other studies, hence radiographers are able to complete such studies promptly,25 , 26 resulting in significantly lower image repeat count in 2020 when compared to 2019 (48.6% vs 51.4%).
On the other hand, the caseload was higher in 2019 (non-pandemic period), when more than half of the patients21 presented to the A&E Department with non-acute complaints. In the literature, patients preferred doing so due to it being a more accessible 24-h facility providing extensive diagnostic procedures, whilst others had a misaligned social understanding of symptom severity and believed they required urgent, immediate care.21, 22, 23 With less acute patients presenting to the A&E in 2019, the image acceptance rate was higher (91.8% vs 90.9%).
It was observed that radiographers working the 12-h shift at the A&E Department were taking fewer sick days compared to radiographers working the three-shifts pattern at the in-patient location. Several reasons could have attributed to this: (1) radiographers working the 12-h shifts were compelled to remain healthy in the spirit of teamwork; (2) stricter infection control measures implemented during the pandemic, such as the emphasis on hand hygiene and the compulsory usage of masks during clinical practice, which have been shown to reduce COVID-19 transmission30 , 31; (3) provision of influenza flu vaccination for all staff– an initiative that has also been advocated for in the United Kingdom32 and the United States of America.33 Such measures would inevitably reduce the spread of infection from within the team, and with sick patients.
Limitations
This study has several limitations. Firstly, given that the study was limited to a single medical imaging centre, the generalisability of the results across other geographic locations or differing demographics would be unclear. Secondly, the study duration was limited to five months. The duration of exposure to the 12-h shift may not have been sufficient for radiographers to conclude on their preferences for the different shift types. Similarly, the study analysis of images acquired and sick days, were only from the five months duration and may not have accurately reflected the outcomes of the new shift type. Thirdly, despite the ratio of participants working the new shift being typical of the radiographer ratio in Singapore, the sample size was small. This small size may not have been representative of the entire radiography profession's sentiments and contributed to several lack of statistical differences in the data. Therefore, future adequately powered studies would be recommended. This study was not able to determine whether, and to what extent, the observed differences between the two aforementioned shift systems can be attributed to just a change in workflow pattern or institutional and global changes brought about as a result of the pandemic.
Conclusion
The shift preferences amongst the radiographers were inconclusive, with 12% more participants favouring the 12-h shifts over the three-shift pattern. Majority opined that the 12-h shifts had longer rest days, but shift work itself became more tiring. There were more favourable image reject counts and lesser sick leave taken with the 12-h shift, possibly related to circumstances brought about by the pandemic. Studying these variables will provide an effective starting point in understanding the efficacy and applicability of the 12-h shifts system at a Radiography department of a local centre during the COVID-19 pandemic.
Conflict of interest statement
None.
Acknowledgements
We wish to thank various individuals for their contributions to this study; Mr Gabriel Leong (Head Radiography), for his support in this study; Ms. Tan Pei Ting (Biostatistician), for her valuable support on the statistical analysis portion of the project; Mr. Tsai Koh Tzan (Principal Radiographer) and Mr. Bradley Keith Emuang (Radiographer), for their help in collecting data on the questionnaire and images acquired respectively.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Appendix A.
Survey questions
Demographics
-
1.
Age group
-
2.
Gender
-
3.
Marital status
-
4.
Married with children?
-
5.
Years of work experience
Your opinion
-
6.
Have you attended to suspected COVID-19 patients?
-
7.
Have you attended to CONFIRMED COVID-10 patients?
-
8.
How many months of 12-h shift at A&E have you done?
-
9.
Which shift patter would you prefer?
-
10.
Why does the shift pattern you've selected above work for you?
References
- 1.Wong T.Y., Koh G., Cheong S.K., Lee H.Y., Fong Y.T., Sundram M. Concerns, perceived impact and preparedness in an avian influenza pandemic-a comparative study between healthcare workers in primary and tertiary care. Ann Acad Med Singapore. 2008;37(2):96–102. [PubMed] [Google Scholar]
- 2.Koh D., Lim M.K., Chia S.E. SARS: health care work can be hazardous to health. Occup Med. 2003;53(4):241–243. doi: 10.1093/occmed/kqg090. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organisation Infection prevention and control during health care when coronavirus disease (COVID-19) is suspected or confirmed. 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-2020.4 1–5. Available from:
- 4.Sim W.Y., Chen R.C., Aw L.P., Abu Bakar R., Tan C.C., Heng A.L. How to safetly and sustainabily reorganise a large general radiography service faving the COVID-19 pandemic. Radiography. 2020:e303–e311. doi: 10.1016/j.radi.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zanardo M., Martini C., Monti C.B., Cattaneo F., Ciaralli C., Cornocchione P. Management of patients with suspected or confirmed COVID-19, in the radiology department. Radiography. 2020:264–268. doi: 10.1016/j.radi.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ball J., Dall'Ora C., Griffiths P., editors. The 12-hour shift: friend or foe? 2015. [Google Scholar]
- 7.Tucker P., Smith L., Macdonald I., Folkard S. Distribution of rest days in 12 hour shift systems: impacts on health, wellbeing, and on shift alertness. Occup Environ Med. 1999;56(3):206–214. doi: 10.1136/oem.56.3.206. https://pubmed.ncbi.nlm.nih.gov/10448331 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1757706/ Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brachet T., David G., Drechsler A.M. The effect of shift structure on performance. Am Econ J Appl Econ. 2012;4(2):219–246. https://www.aeaweb.org/articles?id=10.1257/app.4.2.219 Available from: [Google Scholar]
- 9.Smith L., Folkard S., Tucker P., Macdonald I. Work shift duration: a review comparing eight hour and 12 hour shift systems. Occup Environ Med. 1998;55(4):217–229. doi: 10.1136/oem.55.4.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geiger-Brown J., Trinkoff A.M. Is it time to pull the plug on 12-hour shifts?: Part 1. The evidence. J Nurs Adm. 2010;40(3):100–102. doi: 10.1097/NNA.0b013e3181d0414e. [DOI] [PubMed] [Google Scholar]
- 11.Battle C., Temblett P. 12-hour nursing shifts in critical care: a service evaluation. J Inten Care Soc. 2018;19(3):214–218. doi: 10.1177/1751143717748094. https://journals.sagepub.com/doi/abs/10.1177/1751143717748094 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leech N.L., Onwuegbuzie A.J. A typology of mixed methods research designs. Qual Quantity. 2009;43(2):265–275. doi: 10.1007/s11135-007-9105-3. Available from: [DOI] [Google Scholar]
- 13.Allied Health Professions Council AHPC 2019 Annual report. 2020. https://www.healthprofessionals.gov.sg/ahpc/home/announcement/Index/ahpc-2019-annual-report 24. Available from:
- 14.Wagstaff A.S., Sigstad Lie J.-A. Shift and night work and long working hours – a systematic review of safety implications. Scand J Work Environ Health. 2011;(3):173–185. doi: 10.5271/sjweh.3146. https://www.sjweh.fi/show_abstract.php?abstract_id=3146 Available from: [DOI] [PubMed] [Google Scholar]
- 15.Young C., Smoke M., Farrell T., Ho E. 12-hour shifts for radiation therapists. J Med Imag Radiat Sci. 2017;48(3):294–300. doi: 10.1016/j.jmir.2017.05.002. Available from: [DOI] [PubMed] [Google Scholar]
- 16.National Academies of Sciences E Medicine . The National Academies Press; Washington, DC: 2019. Taking action against clinician burnout: a systems approach to professional well-being; p. 334. [PubMed] [Google Scholar]
- 17.McGettrick K.S., O'Neill M.A. Critical care nurses – perceptions of 12-h shifts. Nurs Crit Care. 2006;11(4):188–197. doi: 10.1111/j.1362-1017.2006.00171.x. Available from: [DOI] [PubMed] [Google Scholar]
- 18.Hong-Choon O., Chow W.L., Peter L., Tiah L., Pak-Liang G., Hoon-Chin S. Patient experience enhancement at accident and emergency department: junior doctor manpower reallocation optimization. J Manag Sci Eng. 2017;2:193. doi: 10.3724/SP.J.1383.203009. [DOI] [Google Scholar]
- 19.Elliot J., Williamson K. The radiology impact of healthcare errors during shift work. Radiography. 2020:248–253. doi: 10.1016/j.radi.2019.12.007. [DOI] [PubMed] [Google Scholar]
- 20.COVID-19 (Temporary measures) Act 2020. Sect. 2020;34 [Google Scholar]
- 21.Idil H., Kilic T.Y., Toker İ., Dura Turan K., Yesilaras M. Non-urgent adult patients in the emergency department: causes and patient characteristics. Turk J Emerg Med. 2018;18(2):71–74. doi: 10.1016/j.tjem.2017.10.002. http://www.sciencedirect.com/science/article/pii/S2452247317301632 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burchard R., Oikonomoulas V., Soost C., Zoremba M., Graw J.A. Indicated trauma emergency department utilization – a comparison between patients' self-assessment and professional evaluation. Int Emerg Nurs. 2019;44:30–34. doi: 10.1016/j.ienj.2019.02.006. http://www.sciencedirect.com/science/article/pii/S1755599X19300175 Available from: [DOI] [PubMed] [Google Scholar]
- 23.Yip J. Overcrowding in emergency departments: revealing the social perspectives through a medical sociological analysis. J Health Soc Sci. 2019;4:305–312. doi: 10.19204/2019/vrcr7. [DOI] [Google Scholar]
- 24.Pung R., Chiew C.J., Young B.E., Chin S., Chen M.I.C., Clapham H.E. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet. 2020;395(10229):1039–1046. doi: 10.1016/S0140-6736(20)30528-6. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cowan I.A., MacDonald S.L., Floyd R.A. Measuring and managing radiologist workload: measuring radiologist reporting times using data from a Radiology information system. J Med Imag Radiat Oncol. 2013;57(5):558–566. doi: 10.1111/1754-9485.12092. https://onlinelibrary.wiley.com/doi/abs/10.1111/1754-9485.12092 Available from: [DOI] [PubMed] [Google Scholar]
- 26.Woznitza N., Piper K., Rowe S., Bhowmik A. Immediate reporting of chest X-rays referred from general practice by reporting radiographers: a single centre feasibility study. Clin Radiol. 2018;73(5) doi: 10.1016/j.crad.2017.11.016. http://www.sciencedirect.com/science/article/pii/S0009926017305366 507.e1-.e8. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Magnan M.A., Beaver C., Suchy S. Workplace fatigue among oncology nursing personnel. Clin J Oncol Nurs. 2015;19(3):370–372. doi: 10.1188/15.CJON.370-372. http://europepmc.org/abstract/MED/26000588 Available from: [DOI] [PubMed] [Google Scholar]
- 28.Tucker P. International Labour Organization; 2006. Compressed working weeks. [Google Scholar]
- 29.Samra H.A., Smith B.A. The effect of staff nurses' shift length and fatigue on patient safety and nurses' health: from the National Association of Neonatal Nurses. Adv Neonatal Care. 2015;15(5):311. doi: 10.1097/anc.0000000000000230. [DOI] [PubMed] [Google Scholar]
- 30.Lai T.H.T., Tang E.W.H., Fung K.S.C., Li K.K.W. Reply to "Does hand hygiene reduce SARS-CoV-2 transmission?". Graefe’s Arch Clin Exp Ophthalmol. 2020;258(5):1135. doi: 10.1007/s00417-020-04653-4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7103093/ Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arav Y., Klausner Z., Fattal E. Understanding the indoor pre-symptomatic transmission mechanism of COVID-19. medRxiv. 2020 http://medrxiv.org/content/early/2020/05/17/2020.05.12.20099085.abstract Available from: [Google Scholar]
- 32.Mahase E. Covid-19: GPs raise workload concerns as government extends flu vaccination programme. BMJ. 2020;370:m2990. doi: 10.1136/bmj.m2990. http://www.bmj.com/content/370/bmj.m2990.abstract Available from: [DOI] [PubMed] [Google Scholar]
- 33.Belongia E.A., Osterholm M.T. COVID-19 and flu, a perfect storm. Science. 2020;368(6496):1163. doi: 10.1126/science.abd2220. http://science.sciencemag.org/content/368/6496/1163.abstract Available from: [DOI] [PubMed] [Google Scholar]