Abstract
Background
An estimated 12.8% of children and adolescents experience chronic health conditions that lead to poor quality of life, adjustment and coping issues, and concurrent mental health problems. Digital health deployment of psychosocial interventions to support youth with chronic illness has become increasingly popular with the advent of the technological advances in the digital age.
Objective
Our objectives were to systematically review published efficacy studies of eHealth and mHealth (mobile health) psychosocial interventions for youths with chronic illnesses and review intervention theory and treatment components.
Methods
PubMed, Embase, Web of Science, PsycInfo, and Cochrane Database of Systematic Reviews were searched for studies published from 2008 to 2019 of eHealth and mHealth psychosocial interventions designed for children and adolescents with chronic illnesses in which efficacy outcomes were reported. We excluded studies of interventions for caregivers, healthy youth, disease and medication management, and telehealth interventions that function solely as a platform to connect patients to providers via phone, text, or videoconference.
Results
We screened 2551 articles and 133 relevant full-text articles. Sixteen efficacy studies with psychosocial and health outcomes representing 12 unique interventions met the inclusion criteria. Of the included studies, 12 were randomized controlled trials and 4 were prospective cohort studies with no comparison group. Most interventions were based in cognitive behavioral theory and designed as eHealth interventions; only 2 were designed as mHealth interventions. All but 2 interventions provided access to support staff via text, phone, email, or discussion forums. The significant heterogeneity in intervention content, intervention structure, medical diagnoses, and outcomes precluded meta-analysis. For example, measurement time points ranged from immediately postcompletion of the mHealth program to 18 months later, and we identified 39 unique outcomes of interest. The majority of included studies (11/16, 69%) reported significant changes in measured health and/or psychosocial posttreatment outcomes, with small to large effect sizes.
Conclusions
Although the available literature on the efficacy of eHealth and mHealth psychosocial interventions for youth with chronic illnesses is limited, preliminary research suggests some evidence of positive treatment responses. Future studies should continue to evaluate whether digital health platforms may be a viable alternative model of delivery to traditional face-to-face approaches.
Keywords: pediatrics, chronic illness, mHealth, eHealth, psychosocial interventions, mental health
Introduction
An increasing number of youths (ie, children and adolescents aged 18 years and younger) are diagnosed with a chronic condition in the United States, with an estimated prevalence rate of 12.8% [1-3]. Chronic illness in childhood negatively impacts quality of life [4,5]. Chronic health conditions can lead to emotional challenges and heighten coping difficulties [6]. Up to 60% of children with a chronic illness have at least one co-occurring psychological disorder [7], compared with 10% to 20% of the general pediatric population [8]. Across illness type, stressors associated with chronic disease are vastly similar. Burdens to these populations include treatment-related stress, changes to daily life and routines, and uncertainty about the future [7,9].
Face-to-face psychosocial interventions such as cognitive behavioral therapy are designed to teach and bolster coping skills and improve psychological adjustment [10]. Such interventions have been developed for various illness populations to improve psychosocial outcomes and quality of life [11]. However, barriers to in-person treatment include limited availability of and access to psychosocial clinicians and high costs of treatment [12,13]. A majority of youths screened in school and primary care settings with elevated mental health symptoms do not follow-up with referrals to mental health clinicians, especially those who are racial/ethnic minorities, have public insurance, or come from low-income households [14]. Additionally, there are workforce shortages in proportion to demand and need, with wait times for psychiatric care appointments exceeding that of pediatricians [15]. A potential solution is leveraging technological advances and digital media to deploy behavioral health interventions on a larger scale. Internet-based interventions (otherwise known as eHealth interventions) confer the advantages of instant availability, anonymity, self-pacing, the ability to reach patients in remote areas, and cost-effectiveness due to reduced personnel and infrastructure requirements [16,17].
Internet-based interventions may be particularly appealing to younger generations who are digital natives accustomed to interacting on smartphones and the internet [16-18]. The internet serves as a primary means of health-related and mental health–related information-seeking and communication for youths [19,20]. Additionally, young people endorse reluctance to seek psychological services due to social stigma, discomfort discussing personal problems, and a preference for self-help [16,17,19,21]. Thus, there has been a rapid growth in the use of eHealth platforms to deploy skills-based behavioral health programs for youths. Moreover, in recent years with the increased use of smartphones there has been a corresponding increase in mobile health (mHealth) apps for symptom self-management on smartphone devices [22,23].
Previous systematic reviews have examined digital interventions in pediatric populations for disease self-management and alleviation of mental health symptoms. Examples include remote management of pediatric chronic pain [24] and technological interventions for asthma self-management in children and adolescents [25-27]. Other reviews have focused on digital health interventions for youth mental health problems [28,29] and internet-based cognitive behavioral therapy for children and adolescents [17,30]. The literature has addressed the benefits of eHealth interventions for anxiety and depression [31], technological tools for disease self-management [32], and technology-based family interventions for improving family functioning [33].
To our knowledge, no existing systematic review has been conducted to critically review the literature on eHealth and mHealth psychosocial interventions for youths with chronic illnesses. Previous reviews in this topic area have focused more narrowly on specific chronic conditions, constellations of mental health symptoms, or types of psychotherapy. Our study objectives were to systematically review the efficacy of eHealth and mHealth psychosocial interventions for youths with chronic illnesses and review underlying intervention theory and treatment components.
Methods
Literature Search
The search was executed by a research librarian in five databases for articles published from 2008 to 2019: PubMed/MEDLINE, Embase, Web of Science, PsycINFO, and Cochrane Database of Systematic Reviews. We used keywords and Boolean operators [34] to identify original articles on eHealth and mHealth psychosocial interventions designed for youths or young adults with chronic illnesses. Inclusion criteria were (1) available in English; (2) published in peer-reviewed journal; (3) experimental, quasi-experimental, and observational studies in which efficacy outcome(s) were reported; (4) eHealth or mHealth psychosocial interventions (with technology as the primary mode of content delivery, either entirely self-guided or human-assisted); and (5) designed for children and adolescents aged 18 years and younger with chronic disease (ie, a long-term medical condition lasting 3 months or longer [35]).
The original primary search strategy with generic chronic illness search terms is shown in Multimedia Appendix 1. Cancer is a specific condition of interest for our research group for which we were aware of existing digital intervention literature. Based on our primary search strategy, the authors identified several known published studies on digital interventions related to 10 specific chronic illnesses. To ensure all relevant articles were captured, a supplemental search strategy related to the specific chronic illnesses identified was then conducted to generate systematic reviews to search some of the more advanced digital intervention science in pediatrics (Multimedia Appendix 2). Our search strategy was guided and conducted by a medical librarian with extensive experience with systematic reviews; the list of search terms for specific chronic illnesses was modeled after published Cochrane reviews (eg, Law et al [36] on caregiver interventions for children with chronic illness). We excluded studies of interventions that target caregivers or health care providers only, interventions that target mental health problems/disorders not in the context of a chronic medical condition, prevention programs for healthy controls, disease and medication management programs, and programs in which the telehealth platform is only used to connect patients to providers via phone, text, or videoconference.
Selection of Studies
First, we screened titles and abstracts of studies retrieved for inclusion and exclusion. We then obtained full texts of articles designated as potentially meeting inclusion criteria to assess for eligibility. Screening of all titles, abstracts, and full-text articles was first independently double-coded by authors in pairs (NL, SW; NL, RP; NL, SFC); each dyad coded a subset of articles and NL coded all articles. Then, disagreements between the authors in each dyad were resolved through discussion while referencing the original source material to reach consensus. Finally, for articles meeting inclusion criteria, we independently double-coded relevant information from each study in pairs (NL, SW; NL, RP; NL, SFC), including study design, sample size, target illness, intervention characteristics (eg, intervention theory and components, eHealth or mHealth platform), and treatment outcomes data.
For intervention characteristics, we relied on authors’ descriptions, either provided in the articles themselves or in prior publications of the intervention referenced in the included articles, and standard norms for psychosocial interventions. For example, if authors described an intervention as being based on cognitive behavioral theory, we coded the theory as cognitive behavioral; if the intervention followed a prespecified order mirroring the stepwise progression of traditional manualized evidence-based psychotherapies, it was coded as a modular treatment session per clinical norms [37]; and if patients could connect with research or psychosocial staff for support, we coded the intervention as human-assisted.
Unsurprisingly, measures collected in studies incorporated both psychosocial outcomes and physical health/disease-related outcomes. In the context of chronic medical conditions, physical and psychological consequences are intertwined and physical health/disease-related outcomes tend to improve alongside emotional and psychological functioning [38]. Outcome measures were categorized as either psychosocial (depression, social problem solving, fear and worry about symptoms, anxiety sensitivity, perceived stress, rewarding pain behavior, quality of life, social acceptance, family conflict, pain catastrophizing, psychological well-being, emotional functioning, parental protectiveness, anxiety, school attendance, self-efficacy, posttraumatic stress symptoms, somatic symptoms, coping strategies) or physical health/disease-related (fatigue, physical functioning, energy, disease symptoms, pain intensity and frequency, pain interference, pain reactivity, sleep, disease knowledge, activity limitations, functional disability). Categorizations were based on the psychosocial background literature [39-41] and agreed upon internally by our interdisciplinary research team which includes intervention science researchers, health services researchers, physicians, and psychologists; we acknowledge that some outcomes such as aspects of pain management, sleep, and functional impairments may fit either categorization. For study design, we used author designations. For example, a study was categorized as a pilot randomized controlled trial (RCT) if described as such in the article. We referred to the articles to resolve any discrepancies during consensus conversations and did not make inferences beyond authors’ definitions and descriptions.
After review of the articles, the team determined that heterogeneity in outcome variables and measurement time points precluded meta-analysis. Thus, we described the data systematically.
Quality Assessment
We independently assessed study quality in pairs (NL, SW; NL, RP; NL, SFC) using the Cochrane Collaboration’s tool for assessing risk of bias [42] to evaluate random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other biases. We coded each category as low, high, or unclear risk of bias according to established standards in the Cochrane handbook for systematic reviews of interventions [43]. We resolved discrepancies in coding during regularly scheduled consensus meetings by referring to the journal articles themselves.
Results
Literature Search
The results of the search and selection of studies are described in the preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram (Figure 1). We screened 2551 articles; 2418 were initially excluded because they did not meet selection criteria. Evaluation of the remaining 133 relevant full-text articles resulted in the exclusion of 117 articles, leaving us with 16 articles that met criteria for inclusion. We provide a synthesis of the findings from the included studies structured around the type of intervention, target population characteristics, intervention content, and type of outcomes.
Figure 1.
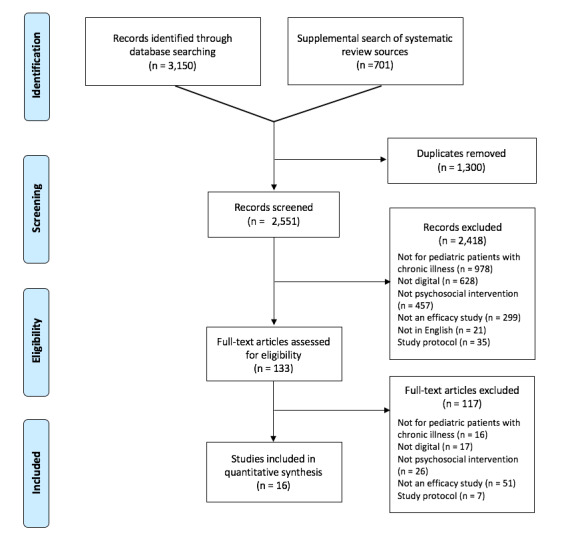
Preferred reporting items for systematic reviews and meta-analyses diagram.
Intervention Characteristics
We found 12 [44-60] unique digital interventions that were developed and tested in the United States [51,55,58], Australia [44], Canada [49,60], Germany [48,54], the Netherlands [47], and Sweden [45,61] (Table 1). Ten were eHealth interventions [44-48,51-59,61] and 2 mHealth interventions [49,60]. We found that over half (7/12, 58%) [45-48,53-58,61] were based on cognitive behavioral therapy principles [62,63]. Other treatment frameworks represented included disease self-management, problem solving, psychoeducation, and social-emotional learning. The interventions varied in length, duration, and number of sessions. All but two interventions incorporated modular treatment sessions that follow a prespecified order (Table 1).
Table 1.
Interventions targeted for youth chronic illness populations.
| Intervention name | Targeted illness |
Age rangea | Country of origin | Platform | Standalone intervention or supplement |
Iterative design process |
Modular or unstructured sessions | Intervention theory |
| Breathe Easier Online [44] | Chronic respiratory condition | 10-17 | Australia | eHealth | Standalone |
|
Modular | Evidence-based social support and problem-solving program following PACEb principle |
| Fatigue in Teenagers on the InterNET [45] | Chronic fatigue syndrome | 12-18 | Netherlands | eHealth | Standalone |
|
Modular | Evidence-based CBTc |
| iCanCope [60] | Chronic pain | 15-18 | Canada | mHealth | Standalone | x | Unstructured | Evidence-based psychological pain management, symptom monitoring |
| iCBTd for adolescents with FGIDe [46,61] | Pain-prominent FGID | 13-17 | Sweden | eHealth | Standalone | x | Modular | Evidence-based iCBT |
| Move It Now [47] | Chronic pain | 12-17 | Netherlands | eHealth | Standalone |
|
Modular | Evidence-based CBT |
| Onco-STEP [48] | Survivors of pediatric cancer | ≥15 | Germany | eHealth | Standalone |
|
Modular | Evidence-based CBT |
| PainSquad+ [49,50] | Cancer pain management | 12-18 | Canada | mHealth | Standalone | x | Unstructured | Evidence-based pharmacological and psychological pain management strategies |
| TeenCope [51] | Type 1 diabetes | 11-14 | US | eHealth | Standalone | x | Modular | Evidence-based psychoeducational intervention based on coping skills training |
| Teens Taking Charge: Managing Arthritis Online [52] | Juvenile idiopathic arthritis | 12-18 | Canada | eHealth | Standalone | x | Modular | Evidence-based self-management strategies |
| Trautmann self-help programs: internet-based CBT, internet-based applied relaxation [53,54] | Recurrent headache | 10-18a | Germany | eHealth | Standalone | x | Modular | Evidence-based CBT, relaxation |
| Web-based management of adolescent pain [55-57] | Chronic pain, recurrent headache, sickle cell disease | 11-18a | US | eHealth | Standalone | x | Modular | Evidence-based CBT |
| Web-based treatment for adolescents with IBDf [58] | Inflammatory bowel disease | 12-17 | US | eHealth | Supplement to face-to-face | x | Modular | Evidence-based CBT |
aAge range represents lowest and highest age range across all studies for the same intervention.
bPACE: problem identification, alternative solution generation, consequences of each alternative solution, execute solution and evaluate.
cCBT: cognitive behavioral therapy.
diCBT: internet-based cognitive behavioral therapy.
eFGID: functional gastrointestinal disorder.
fIBD: inflammatory bowel disease.
All except two were human-assisted (10/12, 83%); human-assisted interventions allowed patients to connect with research or psychosocial staff (ie, psychologist, psychology trainee, nurse, peer counselor) for support via emails, texts, phone calls, private online messaging centers, or message boards (Multimedia Appendix 3). Half of the interventions (6/12, 50%) had some element of caregiver involvement [45-47,52,55-58,61]. Skills practice was notably the only component shared across all interventions. Other components incorporated that lend themselves well to digital intervention platforms include ecological momentary assessment, which allows symptom tracking in real time (4/12, 33%) [64]; tailoring of content to individual users (6/12, 50%); didactic videos (4/12, 33%); online discussion forums (6/12, 50%); and gamification to increase engagement (3/12, 25%).
Participants and Study Characteristics
Participant ages ranged from 10 to 18 years. The targeted chronic illnesses included diabetes, chronic pain, juvenile arthritis, cancer, chronic fatigue syndrome, recurrent headache, chronic respiratory condition, sickle cell disease, and gastrointestinal disorders (Table 1).
Of the 16 included efficacy studies (Tables 2 and 3), there were 3 single-site prospective cohort studies [44,53,57], 1 multisite prospective cohort study [52], 5 pilot RCTs (3 single-site [46,48,58], 2 multisite [49,60]), and 7 phase 2-3 RCTs (4 single-site [45,46,54,56,61], 3 multisite [47,55,59]). The 4 non-RCT prospective cohort studies were pilot studies with small sample sizes ranging from 2061 to 4049 participants with no comparison groups. For the pilot RCTs, sample sizes ranged from 1853 to 8357; one was described as powered for between-groups analyses [57]. The majority had an active treatment comparison condition, with only one using a wait-list control [56]. For the RCTs, sample sizes ranged from 4856 to 32,059; five were described as powered for between-groups analyses [45,55,56,59,61]. A little over half (4/7, 57%) [45,53-55,57,59,61] were compared with an active treatment condition, and the rest were compared with a wait-list control group.
Table 2.
Original research publications with quantitative outcomes: randomized controlled trials only.
| Intervention name | Type of study | Control group | Sample size | Powered for analyses? |
Posttreatment outcomesa.b | Longitudinal outcomesa.b | ||||||
| Breathe Easier Online [44] | Pilot RCTc | Wait-list control | 42 |
|
Psychosocial outcomes: no significant results for depression or social problem solving | N/Ad | ||||||
| Fatigue in Teenagers on the InterNET [45] | RCT | Usual care | 135 | x | Psychosocial outcomes: intervention improved school attendance (P≤.01, 95% CI 2.7 to 8.9) Physical health outcomes: intervention improved fatigue (P≤.01, 95% CI 2.1 to 4.9) and physical functioning (P≤.01, 95% CI 2.3 to 6.3) |
Psychosocial outcomes: intervention improved school attendance at 12 months Physical health outcomes: intervention improved fatigue and physical functioning at 12 months |
||||||
| iCanCope [60] | Pilot multisite RCT | iCanCope version A (symptom tracking only) | 59 |
|
Psychosocial outcomes: no significant results for mood Physical health outcomes: no significant results for pain intensity and interference, physical activity, sleep quality, or energy |
N/A | ||||||
| ICBTe for adolescents with FGIDf [61] | RCT | Wait-list control | 101 | x | Psychosocial outcomes: intervention improved fear and worry about symptoms (95% CI 0.39 to 1.09, dg=0.74), and anxiety sensitivity (95% CI –0.07 to 0.47, d=0.20) No significant results for perceived stress or depressive symptoms Physical health outcomes: intervention improved gastrointestinal symptoms (95% CI 0.16 to 0.84, d=0.50) and pain intensity and frequency (95% CI 0.11 to 0.61, d=0.36) |
Psychosocial outcomes: intervention improved fear and worry about symptoms (95% CI 0.59 to 1.59, d=1.05) and anxiety sensitivity (95% CI 0.10 to 1.04, d=0.57) at 6 months No significant results for perceived stress (95% CI –0.10 to 0.73, d=0.31) or depressive symptoms (95% CI –0.14 to 0.46, d=0.16) at 6 months Physical health outcomes: intervention improved gastrointestinal symptoms (95% CI 0.24 to 1.02, d=0.63) and pain intensity and frequency (95% CI 0.41 to 1.12, d=0.76) at 6 months |
||||||
| Move It Now [47] | Multisite RCT | Wait-list control | 69 |
|
Psychosocial outcomes: intervention improved rewarding pain behavior by parents (P≤.01) and quality of life (P≤.01 to .04, d=–0.87 to 0.34) Physical health outcomes: intervention improved pain intensity (P=.03, d=–0.42), pain interference (P=.03, d=–0.46) and sleep problems (P≤.01, d=–0.60) |
Psychosocial outcomes: intervention improved quality of life (besides mental health subdomain) at 3 months No significant results for rewarding pain behavior by parents at 3 months Physical health outcomes: no significant results for pain intensity, pain interference, or sleep problems at 3 months |
||||||
| TeenCope [59] | Multisite RCT | eHealth managing diabetes psychoeducation for self-management | 320 | x | Psychosocial outcomes: no significant results for quality of life, social acceptance, self-efficacy, perceived stress, or diabetes family conflict Physical health outcomes: no significant results for HbA1ch |
Psychosocial outcomes: no significant results for quality of life, social acceptance, self-efficacy, perceived stress, or diabetes family conflict at 18 months Physical health outcomes: no significant results for HbA1c at 18 months |
||||||
| Teens Taking Charge: Managing Arthritis Online [52] | Pilot multisite RCT | Attentional control | 46 |
|
Psychosocial outcomes: no significant results for quality of life, self-efficacy, or stress Physical health outcomes: intervention improved disease knowledge (P≤.01, d=1.32) and pain intensity (P=.03, d=0.78) |
N/A | ||||||
| Trautmann self-help programs: internet-based CBT, internet-based applied relaxation [54] | 3-arm RCT | Internet psychoeducation intervention | 65 |
|
Psychosocial outcomes: no significant results for pain catastrophizing or psychological well-being Physical health outcomes: no significant results for headache frequency and duration |
Psychosocial outcomes: no significant results for pain catastrophizing or psychological well-being at 6 months Physical health outcomes: no significant results for headache frequency and duration at 6 months |
||||||
| Trautmann’s internet-based CBT [53] | Pilot RCT | Internet psychoeducation intervention | 18 |
|
Psychosocial outcomes: intervention improved pain catastrophizing (P≤.05) Physical health outcomes: intervention improved headache frequency (P≤.05) No significant results for headache intensity or headache duration |
Psychosocial outcomes: intervention improved pain catastrophizing (P≤.05) at 6 months Physical health outcomes: intervention improved headache frequency (P≤.05) at 6 months No significant results for headache intensity or headache duration at 6 months |
||||||
| Web-based management of adolescent pain | ||||||||||||
|
|
Multisite RCT [55] | Internet education control | 273 | x | Psychosocial outcomes: intervention improved emotional functioning (P=.04, d=–0.09) Physical health outcomes: no significant results for activity limitations, pain intensity, or sleep quality |
Psychosocial outcomes: no significant results for emotional functioning at 6 months Physical health outcomes: intervention improved activity limitations (P=.03; d=–0.25) and sleep quality (P=.04, d=0.16) at 6 months No significant results for pain intensity at 6 months |
||||||
|
|
RCT [56] | Wait-list control | 48 | x | Psychosocial outcomes: no significant results for depression or parental protectiveness Physical health outcomes: intervention improved activity limitations (P≤.01, η2i=.17) and pain intensity (P=.03, η2=.11) |
Psychosocial outcomes: no significant results for depression and parental protectiveness at 3 months Physical health outcomes: intervention improved activity limitations and pain intensity at 3 months |
||||||
|
|
Pilot RCT [57] | Specialized headache treatment | 83 | x | Psychosocial outcomes: no significant results for anxiety or depression Physical health outcomes: no significant results for headache frequency, pain intensity, activity limitations, sleep duration, or sleep efficiency |
Psychosocial outcomes: no significant results for anxiety or depression at 3 months Physical health outcomes: no significant results for headache frequency, pain intensity, activity limitations, sleep duration, or sleep efficiency at 3 months |
||||||
aOnly analyses of between-group differences comparing the intervention and control arms are reported.
bInformation regarding confidence intervals, effect size, and P values is included when reported in the original research publication.
cRCT: randomized controlled trial.
dN/A: not applicable.
eiCBT: internet-based cognitive behavioral therapy.
fFGID: functional gastrointestinal disorder.
gd: Cohen d.
hHbA1c: hemoglobin A1c.
iη2: eta squared.
Table 3.
Original research publications with quantitative outcomes: nonrandomized controlled trials.
| Intervention name | Type of study | Sample size | Posttreatment outcomesa | Longitudinal outcomesa |
| ICBTb for adolescents with FGIDc [46] | Pilot study | 29 | Psychosocial outcomes: intervention improved stress (P<.05, 95% CI 0.02 to 0.69, dd=0.35) at posttreatment No significant results for anxiety or depression at posttreatment Physical health outcomes: intervention improved gastrointestinal symptoms (P<.05, 95% CI 2.37 to 10.58, d=0.50), pain interference (P<.05, 95% CI 0.11 to 0.61, d=0.36), and pain reactivity (P<.05, 95% CI 0.39 to 1.09, d=0.74) at posttreatment No significant results for functional disability at posttreatment |
Psychosocial outcomes: intervention improved anxiety (P<.05, 95% CI 0.08 to 0.81, d=0.44) at 6 months No significant results for depression or stress at 6 months Physical health outcomes: intervention improved gastrointestinal symptoms (95% CI 3.43 to 12.21, d=0.63), pain interference (P<.05, 95% CI 0.41 to 1.12, d=0.76), pain reactivity (P<.05, 95% CI 0.59 to 1.59, d=1.05), and functional disability (P<.05, 95% CI 0.10 to 1.04, d=0.56) at 6 months |
| PainSquad+ [49] | Multisite pilot study | 40 | Psychosocial outcomes: intervention improved emotional functioning (P≤.01, d=0.66), social functioning (P≤.01, d=0.46), and overall HRQOLe (P=.02, d=0.43) at posttreatment No significant results for self-efficacy, or school functioning at posttreatment Physical health outcomes: intervention improved pain intensity (P≤.01, d=0.67) and pain interference (P=.03, d=0.38) at posttreatment No significant results for physical functioning at posttreatment |
N/A |
| Onco-STEP [48] | Pilot study | 20 | Psychosocial outcomes: intervention improved posttraumatic stress symptoms (P≤.01, d=0.63), anxiety (P≤.01, d=0.74), fear of progression/relapse (P<.05, d=0.48), and depression (P≤.01, d=1.0) at posttreatment | Psychosocial outcomes: intervention improved posttraumatic stress symptoms (P<.01), fear of progression/relapse (P<.01), and anxiety (P<.01) at 3 months No significant results for depression at 3 months |
| Web-based treatment for adolescents with IBDf [58] | Pilot study | 24 | Psychosocial outcomes: intervention improved somatic symptoms (P≤.01, η2g=.41), approach coping strategies (P≤.01, η2=.43), distraction techniques (P≤.01, η2=.35), protective parenting behaviors (P=.03, η2=.27) at posttreatment Physical health outcomes: no significant results for abdominal pain at posttreatment |
Psychosocial outcomes: intervention improved protective parenting behaviors (P=.01, η2=.44) at 6 months No significant results for somatic symptoms, approach coping strategies, or distraction techniques at 6 months Physical health outcomes: no significant results for abdominal pain at 6 months |
aICBT: internet-based cognitive behavioral therapy.
bInformation regarding confidence intervals, effect size, and P values are included when reported in the original research publication.
cFGID: functional gastrointestinal disorder.
dd: Cohen d.
eHRQOL: health-related quality of life.
fIBD: inflammatory bowel disease.
gη2: eta squared.
Measures of psychosocial outcomes were collected across all studies, and physical health outcomes were collected in 88% (14/16) of studies [45-47,49,52-61] (Tables 2 and 3). However, outcomes assessed were heterogeneous, which prevents holistic synthesis across studies. At posttreatment, 56% (9/16) of the reviewed studies reported significant improvements in psychosocial outcomes (eg, anxiety, depression) [46,48,49,55,58,61]; effect sizes, where reported, ranged from small to large for RCTs and non-RCTs alike [46-49,55,58,61]. At posttreatment, half (8/16, 50%) [45-47,49,52,53,56] of the reviewed studies reported significant improvements in health-related outcomes (eg, physical functioning, disease knowledge); effect sizes, where reported, ranged from small to large for RCTs and non-RCTs alike [46,47,49,52,55,56,61]. In combination, a majority (11/16, 69%) of included studies reported some evidence of efficacy on psychosocial outcomes and/or health-related outcomes at posttreatment [45-49,52,53,55,56,58,59]. Findings across RCTs and non-RCTs were similar, with the exception that all non-RCTs reported some improvements in psychosocial outcomes.
A subset of 75% (12/16) of studies [45-48,53-59,61] evaluated longer term assessment time points ranging from 3 to 18 months (Tables 2 and 3). Nine studies (9/16, 56%) [45-48,53,55,56,58,61] showed promise of longer term gains from the intervention.
Risk of Bias
Risk of bias was evaluated for all included studies (Figure 2). Of the 16 studies, 12 reported random sequence generation and allocation concealment (ie, the pilot RCTs and RCTs). For the blinding of participants and personnel domain, 10 were high risk and 6 low risk; high-risk studies consisted of study designs with no control group or a wait-list control group. For the blinding of outcome assessment domain, 9 were high risk and 7 low risk. For attrition bias, 8 were low risk, 5 high risk, and 3 unclear; note that attrition rates for internet-based interventions (with an anchor point of around 50%) tend to be higher than traditional face-to-face psychosocial interventions [65]. For selective reporting bias, studies were split in half between low risk and unclear; studies were rated as unclear due to a lack of clinical trial registration or published protocol. For other biases, 12 were considered low risk and 4 high risk.
Figure 2.

Risk of bias.
Discussion
Overview
A majority of youth with chronic illnesses struggle with issues that psychosocial interventions effectively manage such as anxiety, stress, depression, maladjustment, pain, and poor coping skills [4,7]. Within the past decade, digital health interventions have been increasingly popular with widespread access to the internet and smartphones. To our knowledge, this is the first systematic review summarizing the research evidence in support of the efficacy of eHealth and mHealth psychosocial interventions for youth chronic illnesses. Each of the interventions identified was designed for a specific chronic illness population. The state of the science is still in its nascent stages, with only 16 published efficacy studies of 12 unique interventions identified. We provided information on the structure and content of included interventions and relationships between each of the interventions and various psychosocial and health outcomes. Given the substantial number of studies in which full articles were reviewed for eligibility (n=133, Figure 1), this points to growing interest in digital interventions for youth with chronic illnesses. Few digital interventions have advanced to the stages of efficacy testing (n=16), and even fewer in an RCT with an active comparison condition (n=8). This systematic review suggests that disseminating traditional evidence-based psychotherapies via novel digital health technologies may be efficacious.
Consistent with evidence-based digital health practices and recent systematic reviews of digital interventions with youth chronic illness and mental health populations [17,24,25,28,33], our systematic review of eHealth and mHealth psychosocial interventions for youth chronic illness populations found (a) early evidence of improvements in psychosocial and physical health outcomes immediately posttreatment; (b) early evidence of the maintenance of treatment gains at longer term follow-up extending to 3+ months; (c) a prevalence of computerized cognitive behavioral therapy interventions; (d) varying levels of psychosocial staff support via text, email, phone, online discussion forums, or private online messaging centers; and (e) key methodological limitations for a majority of included studies such as lack of blinded outcomes assessment, limited number of RCTs, and few studies with active treatment comparison groups.
This review also suggests several gaps in the existing literature. Future research should focus on optimizing digital intervention design and implementation, namely how to efficiently streamline resource-intensive personnel assistance and encourage self-direction in order to sustain intervention efficacy and engagement while minimizing costs [66]. Notably, only two of the included interventions did not involve some form of contact with providers or research staff. In addition to clinician involvement, given that half of the interventions reviewed included caregiver support, new digital intervention research should continue to explore the additive value of caregiver involvement where appropriate with unique content designed for parent caregivers [55,56]. Next, as each of the interventions included in our review was designed for a specific chronic illness, further research is needed to ascertain whether a disease nonspecific transdiagnostic approach [67,68] to designing digital psychosocial interventions applicable across heterogeneous disease groups is warranted. In particular, online mindfulness-based interventions have been shown to be successful in chronic illness and other populations [69-71]. Interventions also had multiple components, which may benefit from dismantling studies to identify which active therapeutic ingredients lead to positive outcomes [72]. Similarly, emphasis should be placed on identifying and targeting the aspects of digital engagement that lead to the intended behavior change rather than just encouraging more frequent use [73]. The use of analytics in eHealth and mHealth can provide invaluable insights into active therapeutic ingredients, aspects of effective digital engagement, treatment moderators (for whom interventions work), and treatment mediators (how treatments work) [74,75]. Finally, future studies might assess the value of more novel technologically enabled features such as just-in-time adaptive intervention designs (JITAIs). Indeed, JITAIs use causal modeling to identify the appropriate type and dose of intervention at the optimal point in time by measuring and responding to an individual’s changing health states [76,77]. These innovative programs have the potential to meet evolving real-time needs of youth at risk.
Given the interest in and rapidly changing landscape of digital health, it is likely that new publications have been released during the typical time frame it had taken us to rigorously complete our systematic review. We intend to publish a 5-year systematic review update populated with new efficacy studies and trials. The median timing of Cochrane systematic review updates is greater than 5 years [78]. Although previous research suggests only 4% of systematic review updates report a change in conclusions [79], our overarching findings may be subject to change given the limited number of included studies and the quickly evolving digital health landscape.
Limitations
Limitations to consider are as follows. First, most of the interventions were designed and tested as web-based eHealth interventions, with only two mHealth intervention designed for use on smartphone devices. We anticipate that more mHealth interventions will be tested for efficacy and come down the pipeline in the years to come as smartphones become more and more ubiquitous. Previous research suggests that mHealth apps are widely accepted by the general public for coping skills and stress management, and beliefs and attitudes toward mHealth are positive [80]. Second, the majority of studies were not powered to detect meaningful changes in health outcomes of interest nor did they designate primary versus secondary outcomes in their research designs. Third, only half of the studies used an active treatment comparison condition or blinded participants to assigned treatment condition, and findings of favorable treatment response may be susceptible to the placebo effect [81]. Fourth, there exists the possibility of publication bias because nonsignificant findings are often difficult to publish. Fifth, although our search was executed by a medical librarian in five well-established library databases, other databases to which our university does not have access (eg, Scopus) may have uncovered additional relevant publications. Finally, given the heterogeneity of disease groups, measurement time points, and study outcomes measures, it was not possible to conduct a meta-analysis and provide synthesized results of the efficacy studies included in our systematic review.
Conclusions
The strengths of this paper include the systematic approach to synthesizing the great breadth of literature across pediatric illness populations and the eHealth and mHealth focus increasingly popular among youths. This publication is especially timely given heightened psychological distress and exacerbating mental health symptoms for youth in the context of the COVID-19 pandemic, in-home confinement, school closures, social distancing, and a shift toward online and telehealth services [82-85]. We found intervention features unique to digital platforms such as gamification, ecological momentary assessment, and machine learning algorithms. Such features capitalize on technological advances to intervene during distressing situations in real time and tailor content to individual preferences and needs. Leveraging such technological advances allows movement toward a data-driven and personalized approach to precision mental health [86]. The state of the science is still in its early stages, and further clinical trials research is needed to confirm whether evidence-based psychosocial interventions traditionally delivered in-person may be successfully translated to digital formats for a range of youth chronic illness populations.
Acknowledgments
NL is funded as an Implementation Science Scholar through the National Heart, Lung, and Blood Institute of the National Institutes of Health (grant number: 5K12 HL137940-02).
Abbreviations
- JITAI
just-in-time adaptive intervention design
- mHealth
mobile health apps
- PRISMA
preferred reporting items for systematic reviews and meta-analyses
- RCT
randomized controlled trial
Appendix
Primary search strategy.
Supplemental search strategy.
Intervention and personnel-supported components.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. JAMA. 2010 Feb 17;303(7):623–630. doi: 10.1001/jama.2010.104. [DOI] [PubMed] [Google Scholar]
- 2.van Dyck PC, Kogan MD, McPherson MG, Weissman GR, Newacheck PW. Prevalence and characteristics of children with special health care needs. Arch Pediatr Adolesc Med. 2004 Sep;158(9):884–890. doi: 10.1001/archpedi.158.9.884. [DOI] [PubMed] [Google Scholar]
- 3.Miller GF, Coffield E, Leroy Z, Wallin R. Prevalence and costs of five chronic conditions in children. J Sch Nurs. 2016 Oct;32(5):357–364. doi: 10.1177/1059840516641190. http://europepmc.org/abstract/MED/27044668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wallander JL, Varni JW. Effects of pediatric chronic physical disorders on child and family adjustment. J Child Psychol Psychiatry. 1998 Jan;39(1):29–46. [PubMed] [Google Scholar]
- 5.Yeo M, Sawyer S. Chronic illness and disability. BMJ. 2005 Mar 26;330(7493):721–723. doi: 10.1136/bmj.330.7493.721. http://europepmc.org/abstract/MED/15790645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Warschburger P, Hänig J, Friedt M, Posovszky C, Schier M, Calvano C. Health-related quality of life in children with abdominal pain due to functional or organic gastrointestinal disorders. J Pediatr Psychol. 2014;39(1):45–54. doi: 10.1093/jpepsy/jst070. [DOI] [PubMed] [Google Scholar]
- 7.Butler A, Van Lieshout RJ, Lipman EL, MacMillan HL, Gonzalez A, Gorter JW, Georgiades K, Speechley KN, Boyle MH, Ferro MA. Mental disorder in children with physical conditions: a pilot study. BMJ Open. 2018 Dec 03;8(1):e019011. doi: 10.1136/bmjopen-2017-019011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, Rohde LA, Srinath S, Ulkuer N, Rahman A. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011 Oct 22;378(9801):1515–1525. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- 9.Compas BE, Jaser SS, Dunn MJ, Rodriguez EM. Coping with chronic illness in childhood and adolescence. Annu Rev Clin Psychol. 2012;8:455–480. doi: 10.1146/annurev-clinpsy-032511-143108. http://europepmc.org/abstract/MED/22224836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ruiz F. Acceptance and commitment therapy versus traditional cognitive behavioral therapy: a systematic review and meta-analysis of current empirical evidence. In J Psychol Psychologic Ther. 2012;12(3):333–358. https://dialnet.unirioja.es/servlet/articulo?codigo=4019738. [Google Scholar]
- 11.Tark R, Metelitsa M, Akkermann K, Saks K, Mikkel S, Haljas K. Usability, acceptability, feasibility, and effectiveness of a gamified mobile health intervention (Triumf) for pediatric patients: qualitative study. JMIR Serious Games. 2019 Sep 30;7(3):e13776. doi: 10.2196/13776. https://games.jmir.org/2019/3/e13776/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pai ALH, McGrady M. Systematic review and meta-analysis of psychological interventions to promote treatment adherence in children, adolescents, and young adults with chronic illness. J Pediatr Psychol. 2014 Sep;39(8):918–931. doi: 10.1093/jpepsy/jsu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barlow JH, Ellard DR. Psycho-educational interventions for children with chronic disease, parents and siblings: an overview of the research evidence base. Child Care Health Dev. 2004 Nov;30(6):637–645. doi: 10.1111/j.1365-2214.2004.00474.x. [DOI] [PubMed] [Google Scholar]
- 14.Mojtabai R, Olfson M. National trends in mental health care for US adolescents. JAMA Psychiatry. 2020 Jul 01;77(7):703–714. doi: 10.1001/jamapsychiatry.2020.0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cama S, Malowney M, Smith AJB, Spottswood M, Cheng E, Ostrowsky L, Rengifo J, Boyd JW. Availability of outpatient mental health care by pediatricians and child psychiatrists in five U.S. cities. Int J Health Serv. 2017 Oct;47(4):621–635. doi: 10.1177/0020731417707492. [DOI] [PubMed] [Google Scholar]
- 16.Ybarra ML, Eaton WW. Internet-based mental health interventions. Ment Health Serv Res. 2005 Jun;7(2):75–87. doi: 10.1007/s11020-005-3779-8. [DOI] [PubMed] [Google Scholar]
- 17.Ebert DD, Zarski A, Christensen H, Stikkelbroek Y, Cuijpers P, Berking M, Riper H. Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: a meta-analysis of randomized controlled outcome trials. PLoS One. 2015;10(3):e0119895. doi: 10.1371/journal.pone.0119895. http://dx.plos.org/10.1371/journal.pone.0119895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Granger D, Vandelanotte C, Duncan MJ, Alley S, Schoeppe S, Short C, Rebar A. Is preference for mHealth intervention delivery platform associated with delivery platform familiarity? BMC Public Health. 2016 Jul 22;16:619. doi: 10.1186/s12889-016-3316-2. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-016-3316-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113. doi: 10.1186/1471-244X-10-113. http://www.biomedcentral.com/1471-244X/10/113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gray NJ, Klein JD, Noyce PR, Sesselberg TS, Cantrill JA. Health information-seeking behaviour in adolescence: the place of the internet. Soc Sci Med. 2005 Apr;60(7):1467–1478. doi: 10.1016/j.socscimed.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 21.Spek V, Cuijpers P, Nyklícek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med. 2007 Mar;37(3):319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- 22.Clarke AM, Kuosmanen T, Barry MM. A systematic review of online youth mental health promotion and prevention interventions. J Youth Adolesc. 2015 Jan;44(1):90–113. doi: 10.1007/s10964-014-0165-0. [DOI] [PubMed] [Google Scholar]
- 23.Proudfoot J, Parker G, Hadzi PD, Manicavasagar V, Adler E, Whitton A. Community attitudes to the appropriation of mobile phones for monitoring and managing depression, anxiety, and stress. J Med Internet Res. 2010;12(5):e64. doi: 10.2196/jmir.1475. http://www.jmir.org/2010/5/e64/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fisher E, Law E, Dudeney J, Eccleston C, Palermo TM. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2019 Apr 02;4:CD011118. doi: 10.1002/14651858.CD011118.pub3. http://europepmc.org/abstract/MED/30939227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ramsey RR, Plevinsky JM, Kollin SR, Gibler RC, Guilbert TW, Hommel KA. Systematic review of digital interventions for pediatric asthma management. J Allergy Clin Immunol Pract. 2020 Apr;8(4):1284–1293. doi: 10.1016/j.jaip.2019.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nickels A, Dimov V. Innovations in technology: social media and mobile technology in the care of adolescents with asthma. Curr Allergy Asthma Rep. 2012 Dec;12(6):607–612. doi: 10.1007/s11882-012-0299-7. [DOI] [PubMed] [Google Scholar]
- 27.Alquran A, Lambert KA, Farouque A, Holland A, Davies J, Lampugnani ER, Erbas B. Smartphone applications for encouraging asthma self-management in adolescents: a systematic review. Int J Environ Res Public Health. 2018 Dec 29;15(11) doi: 10.3390/ijerph15112403. http://www.mdpi.com/resolver?pii=ijerph15112403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hollis C, Falconer CJ, Martin JL, Whittington C, Stockton S, Glazebrook C, Davies EB. Annual research review: digital health interventions for children and young people with mental health problems: a systematic and meta-review. J Child Psychol Psychiatry. 2016 Dec 10;58(4):474–503. doi: 10.1111/jcpp.12663. [DOI] [PubMed] [Google Scholar]
- 29.Grist R, Porter J, Stallard P. Mental health mobile apps for preadolescents and adolescents: a systematic review. J Med Internet Res. 2017 May 25;19(5):e176. doi: 10.2196/jmir.7332. http://www.jmir.org/2017/5/e176/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vigerland S, Lenhard F, Bonnert M, Lalouni M, Hedman E, Ahlen J, Olén O, Serlachius E, Ljótsson B. Internet-delivered cognitive behavior therapy for children and adolescents: a systematic review and meta-analysis. Clin Psychol Rev. 2016 Dec;50:1–10. doi: 10.1016/j.cpr.2016.09.005. https://linkinghub.elsevier.com/retrieve/pii/S0272-7358(15)30090-8. [DOI] [PubMed] [Google Scholar]
- 31.Thabrew H, Stasiak K, Hetrick SE, Wong S, Huss JH, Merry SN. E-Health interventions for anxiety and depression in children and adolescents with long-term physical conditions. Cochrane Database Syst Rev. 2018 Aug 15;8:CD012489. doi: 10.1002/14651858.CD012489.pub2. http://europepmc.org/abstract/MED/30110718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Low JK, Manias E. Use of technology-based tools to support adolescents and young adults with chronic disease: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2019 Jul 18;7(7):e12042. doi: 10.2196/12042. https://mhealth.jmir.org/2019/7/e12042/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Canter KS, Christofferson J, Scialla MA, Kazak AE. Technology-focused family interventions in pediatric chronic illness: a systematic review. J Clin Psychol Med Settings. 2018 Apr 20;26(1):68–87. doi: 10.1007/s10880-018-9565-8. [DOI] [PubMed] [Google Scholar]
- 34.Rousseau GK, Jamieson BA, Rogers WA, Mead SE, Sit RA. Assessing the usability of on-line library systems. Behav Inf Technol. 1998 Jan;17(5):274–281. doi: 10.1080/014492998119346. [DOI] [Google Scholar]
- 35.Bernell S, Howard SW. Use your words carefully: what is a chronic disease? Front Public Health. 2016;4:159. doi: 10.3389/fpubh.2016.00159. doi: 10.3389/fpubh.2016.00159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Law E, Fisher E, Eccleston C, Palermo TM. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst Rev. 2019 Mar 18;3:CD009660. doi: 10.1002/14651858.CD009660.pub4. http://europepmc.org/abstract/MED/30883665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scaturo DJ. The evolution of psychotherapy and the concept of manualization: an integrative perspective. Prof Psychol Res Pract. 2001;32(5):522–530. doi: 10.1037/0735-7028.32.5.522. [DOI] [Google Scholar]
- 38.McFarlane AC. The long-term costs of traumatic stress: intertwined physical and psychological consequences. World Psychiatry. 2010 Feb;9(1):3–10. doi: 10.1002/j.2051-5545.2010.tb00254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vannatta K, Gerhardt C. Pediatric oncology: psychosocial outcomes for children and families. In: Roberts MC, editor. Handbook of Pediatric Psychology. New York: Guilford Press; 2003. pp. 342–357. [Google Scholar]
- 40.Hanson CL, Henggeler SW, Burghen GA. Model of associations between psychosocial variables and health-outcome measures of adolescents with IDDM. Diabetes Care. 1987;10(6):752–758. doi: 10.2337/diacare.10.6.752. [DOI] [PubMed] [Google Scholar]
- 41.Livneh H. Psychosocial adaptation to chronic illness and disability. Rehabil Couns Bull. 2016 Aug 13;44(3):151–160. doi: 10.1177/003435520104400305. [DOI] [Google Scholar]
- 42.Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. http://europepmc.org/abstract/MED/22008217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Higgins J, Thomas J, Chandler J. Cochrane Handbook for Systematic Reviews of Interventions. Hoboken: John Wiley & Sons; 2019. [Google Scholar]
- 44.Newcombe PA, Dunn TL, Casey LM, Sheffield JK, Petsky H, Anderson-James S, Chang AB. Breathe Easier Online: evaluation of a randomized controlled pilot trial of an Internet-based intervention to improve well-being in children and adolescents with a chronic respiratory condition. J Med Internet Res. 2012 Feb 08;14(1):e23. doi: 10.2196/jmir.1997. http://www.jmir.org/2012/1/e23/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nijhof SL, Bleijenberg G, Uiterwaal CSPM, Kimpen JLL, van de Putte EM. Effectiveness of internet-based cognitive behavioural treatment for adolescents with chronic fatigue syndrome (FITNET): a randomised controlled trial. Lancet. 2012 Apr 14;379(9824):1412–1418. doi: 10.1016/S0140-6736(12)60025-7. [DOI] [PubMed] [Google Scholar]
- 46.Bonnert M, Ljótsson B, Hedman E, Andersson J, Arnell H, Benninga MA, Simrén M, Thulin H, Thulin U, Vigerland S, Serlachius E, Olén O. Internet-delivered cognitive behavior therapy for adolescents with functional gastrointestinal disorders: an open trial. Internet Interv. 2014 Jul;1(3):141–148. doi: 10.1016/j.invent.2014.07.002. [DOI] [Google Scholar]
- 47.Voerman JS, Remerie S, Westendorp T, Timman R, Busschbach JJV, Passchier J, de Klerk C. Effects of a guided internet-delivered self-help intervention for adolescents with chronic pain. J Pain. 2015 Nov;16(11):1115–1126. doi: 10.1016/j.jpain.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 48.Seitz DCM, Knaevelsrud C, Duran G, Waadt S, Loos S, Goldbeck L. Efficacy of an internet-based cognitive-behavioral intervention for long-term survivors of pediatric cancer: a pilot study. Support Care Cancer. 2014 Aug;22(8):2075–2083. doi: 10.1007/s00520-014-2193-4. [DOI] [PubMed] [Google Scholar]
- 49.Jibb LA, Stevens BJ, Nathan PC, Seto E, Cafazzo JA, Johnston DL, Hum V, Stinson JN. Implementation and preliminary effectiveness of a real-time pain management smartphone app for adolescents with cancer: a multicenter pilot clinical study. Pediatr Blood Cancer. 2017 Oct;64(10) doi: 10.1002/pbc.26554. [DOI] [PubMed] [Google Scholar]
- 50.Jibb LA, Stevens BJ, Nathan PC, Seto E, Cafazzo JA, Johnston DL, Hum V, Stinson JN. Perceptions of adolescents with cancer related to a pain management app and its evaluation: qualitative study nested within a multicenter pilot feasibility study. JMIR Mhealth Uhealth. 2018 Apr 06;6(4):e80. doi: 10.2196/mhealth.9319. http://mhealth.jmir.org/2018/4/e80/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Whittemore R, Jaser SS, Faulkner MS, Murphy K, Delamater A, Grey M. Type 1 diabetes eHealth psychoeducation: youth recruitment, participation, and satisfaction. J Med Internet Res. 2013;15(1):e15. doi: 10.2196/jmir.2170. http://www.jmir.org/2013/1/e15/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stinson J, McGrath P, Hodnett E, Feldman B, Duffy C, Huber A, Tucker L, Hetherington R, Tse S, Spiegel L, Campillo S, Gill N, White M. Usability testing of an online self-management program for adolescents with juvenile idiopathic arthritis. J Med Internet Res. 2010;12(3):e30. doi: 10.2196/jmir.1349. http://www.jmir.org/2010/3/e30/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Trautmann E, Kröner-Herwig B. Internet-based self-help training for children and adolescents with recurrent headache: a pilot study. Behav Cogn Psychother. 2008 Apr 15;36(2):241–245. doi: 10.1017/s1352465808004219. [DOI] [Google Scholar]
- 54.Trautmann E, Kröner-Herwig B. A randomized controlled trial of Internet-based self-help training for recurrent headache in childhood and adolescence. Behav Res Ther. 2010 Jan;48(1):28–37. doi: 10.1016/j.brat.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 55.Palermo TM, Law EF, Fales J, Bromberg MH, Jessen-Fiddick T, Tai G. Internet-delivered cognitive-behavioral treatment for adolescents with chronic pain and their parents: a randomized controlled multicenter trial. Pain. 2016 Jan;157(1):174–185. doi: 10.1097/j.pain.0000000000000348. http://europepmc.org/abstract/MED/26335910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Palermo TM, Wilson AC, Peters M, Lewandowski A, Somhegyi H. Randomized controlled trial of an Internet-delivered family cognitive-behavioral therapy intervention for children and adolescents with chronic pain. Pain. 2009 Nov;146(1-2):205–213. doi: 10.1016/j.pain.2009.07.034. http://europepmc.org/abstract/MED/19695776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Law EF, Beals-Erickson SE, Noel M, Claar R, Palermo TM. Pilot randomized controlled trial of internet-delivered cognitive-behavioral treatment for pediatric headache. Headache. 2015;55(10):1410–1425. doi: 10.1111/head.12635. http://europepmc.org/abstract/MED/26316194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McCormick M, Reed-Knight B, Lewis JD, Gold BD, Blount RL. Coping skills for reducing pain and somatic symptoms in adolescents with IBD. Inflamm Bowel Dis. 2010 Dec;16(12):2148–2157. doi: 10.1002/ibd.21302. [DOI] [PubMed] [Google Scholar]
- 59.Grey M, Whittemore R, Jeon S, Murphy K, Faulkner MS, Delamater A, TeenCope SG. Internet psycho-education programs improve outcomes in youth with type 1 diabetes. Diabetes Care. 2013 Sep;36(9):2475–2482. doi: 10.2337/dc12-2199. http://europepmc.org/abstract/MED/23579179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lalloo C, Hundert A, Harris L, Pham Q, Campbell F, Chorney J, Dick B, Simmonds M, Cafazzo J, Stinson J. Capturing daily disease experiences of adolescents with chronic pain: mhealth-mediated symptom tracking. JMIR Mhealth Uhealth. 2019 Jan 17;7(1):e11838. doi: 10.2196/11838. http://mhealth.jmir.org/2019/1/e11838/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bonnert M, Olén O, Lalouni M, Benninga MA, Bottai M, Engelbrektsson J, Hedman E, Lenhard F, Melin B, Simrén M, Vigerland S, Serlachius E, Ljótsson B. Internet-delivered cognitive behavior therapy for adolescents with irritable bowel syndrome: a randomized controlled trial. Am J Gastroenterol. 2017 Jan;112(1):152–162. doi: 10.1038/ajg.2016.503. [DOI] [PubMed] [Google Scholar]
- 62.Hofmann SG, Asnaani A, Vonk IJJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit Ther Res. 2012 Oct 1;36(5):427–440. doi: 10.1007/s10608-012-9476-1. http://europepmc.org/abstract/MED/23459093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sperry L. Treatment of Chronic Medical Conditions: Cognitive-Behavioral Therapy Strategies and Integrative Treatment Protocols. Washington: American Psychological Association; 2009. [Google Scholar]
- 64.Firth J, Torous J, Yung AR. Ecological momentary assessment and beyond: the rising interest in e-mental health research. J Psychiatr Res. 2016 Sep;80:3–4. doi: 10.1016/j.jpsychires.2016.05.002. http://linkinghub.elsevier.com/retrieve/pii/S0022-3956(16)30085-1. [DOI] [PubMed] [Google Scholar]
- 65.Eysenbach G. The law of attrition. J Med Internet Res. 2005;7(1):e11. doi: 10.2196/jmir.7.1.e11. http://www.jmir.org/2005/1/e11/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mohr DC, Burns MN, Schueller SM, Clarke G, Klinkman M. Behavioral intervention technologies: evidence review and recommendations for future research in mental health. Gen Hosp Psychiatry. 2013 Aug;35(4):332–338. doi: 10.1016/j.genhosppsych.2013.03.008. http://linkinghub.elsevier.com/retrieve/pii/S0163-8343(13)00069-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S, Bentley KH, Thompson-Hollands J, Conklin LR, Boswell JF, Ametaj A, Carl JR, Boettcher HT, Cassiello-Robbins C. The unified protocol for transdiagnostic treatment of emotional disorders compared with diagnosis-specific protocols for anxiety disorders: a randomized clinical trial. JAMA Psychiatry. 2017 Aug 02;74(9):875–884. doi: 10.1001/jamapsychiatry.2017.2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Steele SJ, Farchione TJ, Cassiello-Robbins C, Ametaj A, Sbi S, Sauer-Zavala S, Barlow DH. Efficacy of the unified protocol for transdiagnostic treatment of comorbid psychopathology accompanying emotional disorders compared to treatments targeting single disorders. J Psychiatr Res. 2018 Sep;104:211–216. doi: 10.1016/j.jpsychires.2018.08.005. http://europepmc.org/abstract/MED/30103069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Abujaradeh H, Safadi R, Sereika SM, Kahle CT, Cohen SM. Mindfulness-based interventions among adolescents with chronic diseases in clinical settings: a systematic review. J Pediatr Health Care. 2018;32(5):455–472. doi: 10.1016/j.pedhc.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 70.Zou L, Yeung A, Quan X, Boyden SD, Wang H. A systematic review and meta-analysis of mindfulness-based (Baduanjin) exercise for alleviating musculoskeletal pain and improving sleep quality in people with chronic diseases. Int J Environ Res Public Health. 2018 Jan 25;15(2) doi: 10.3390/ijerph15020206. http://www.mdpi.com/resolver?pii=ijerph15020206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ahmad F, Wang J, El Morr C. Online mindfulness interventions: a systematic review. In: Ahmad F, Wang J, El Morr C, editors. Novel Applications of Virtual Communities in Healthcare Settings. Hershey: IGI Global; 2018. pp. 1–27. [Google Scholar]
- 72.Papa A, Follette W. Dismantling studies of psychotherapy. In: Papa A, Follette W, editors. The Encyclopedia of Clinical Psychology. Hoboken: John Wiley & Sons; 2014. pp. 1–6. [Google Scholar]
- 73.Yardley L, Spring BJ, Riper H, Morrison LG, Crane DH, Curtis K, Merchant GC, Naughton F, Blandford A. Understanding and promoting effective engagement with digital behavior change interventions. Am J Prev Med. 2016 Nov;51(5):833–842. doi: 10.1016/j.amepre.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 74.El Morr C, Ali-Hassan H. Analytics in Healthcare: A Practical Introduction. Berlin: Springer; 2019. [Google Scholar]
- 75.El Morr C, Ritvo P, Ahmad F, Moineddin R. Effectiveness of an 8-week web-based mindfulness virtual community intervention for university students on symptoms of stress, anxiety, and depression: randomized controlled trial. JMIR Ment Health. 2020 Jul 17;7(7):e18595. doi: 10.2196/18595. https://mental.jmir.org/2020/7/e18595/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nahum-Shani I, Smith SN, Spring BJ, Collins LM, Witkiewitz K, Tewari A, Murphy SA. Just-in-time adaptive interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support. Ann Behav Med. 2018 May 18;52(6):446–462. doi: 10.1007/s12160-016-9830-8. http://europepmc.org/abstract/MED/27663578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Klasnja P, Hekler EB, Shiffman S, Boruvka A, Almirall D, Tewari A, Murphy SA. Microrandomized trials: an experimental design for developing just-in-time adaptive interventions. Health Psychol. 2015 Dec;34 Suppl:1220–1228. doi: 10.1037/hea0000305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bashir R, Surian D, Dunn AG. Time-to-update of systematic reviews relative to the availability of new evidence. Syst Rev. 2018 Nov 17;7(1):195. doi: 10.1186/s13643-018-0856-9. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-018-0856-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.French SD, McDonald S, McKenzie JE, Green SE. Investing in updating: how do conclusions change when Cochrane systematic reviews are updated? BMC Med Res Methodol. 2005 Oct 14;5:33. doi: 10.1186/1471-2288-5-33. https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-5-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Apolinário-Hagen J, Hennemann S, Fritsche L, Drüge M, Breil B. Determinant factors of public acceptance of stress management apps: survey study. JMIR Ment Health. 2019 Nov 07;6(11):e15373. doi: 10.2196/15373. https://mental.jmir.org/2019/11/e15373/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Price DD, Finniss DG, Benedetti F. A comprehensive review of the placebo effect: recent advances and current thought. Annu Rev Psychol. 2008;59:565–590. doi: 10.1146/annurev.psych.59.113006.095941. [DOI] [PubMed] [Google Scholar]
- 82.Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singapore. 2020 Jan;49(1):1–3. http://www.annals.edu.sg/pdf/special/COM20043_HoCSH_2.pdf. [PubMed] [Google Scholar]
- 83.Liu S, Yang L, Zhang C, Xiang Y, Liu Z, Hu S, Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020 Apr;7(4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020 Mar 21;395(10228):945–947. doi: 10.1016/S0140-6736(20)30547-X. http://europepmc.org/abstract/MED/32145186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020 Apr 14; doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- 86.Bickman L, Lyon AR, Wolpert M. Achieving precision mental health through effective assessment, monitoring, and feedback processes: introduction to the special issue. Adm Policy Ment Health. 2016 May;43(3):271–276. doi: 10.1007/s10488-016-0718-5. http://europepmc.org/abstract/MED/26887937. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Primary search strategy.
Supplemental search strategy.
Intervention and personnel-supported components.


