Abstract
Background
Glucocorticoids may impact the accuracy of serum cystatin C (sCysC) in reflecting renal function. We aimed to assess the effect of glucocorticoids on the performance of sCysC in detecting acute kidney injury (AKI) in critically ill patients.
Methods
A prospective observational cohort study was performed in a general intensive care unit (ICU). Using propensity score matching, we successfully matched 240 glucocorticoid users with 960 non-users among 2716 patients. Serum creatinine (SCr) and sCysC were measured for all patients at ICU admission. Patients were divided into four groups based on cumulative doses of glucocorticoids within 5 days before ICU admission (Group I: non-users; Group II: 0 mg < prednisone ≤50 mg; Group III: 50 mg < prednisone ≤150 mg; Group IV: prednisone > 150 mg). We compared the performance of sCysC for diagnosing and predicting AKI in different groups using the area under the receiver operator characteristic curve (AUC).
Results
A total of 240 patients received glucocorticoid medication within 5 days before ICU admission. Before and after matching, the differences of sCysC levels between glucocorticoid users and non-users were both significant (P < 0.001). The multiple linear regression analysis revealed that glucocorticoids were independently associated with sCysC (P < 0.001). After matching, the group I had significantly lower sCysC levels than the group III and group IV (P < 0.05), but there were no significant differences in sCysC levels within different glucocorticoids recipient groups (P > 0.05). Simultaneously, we did not find significant differences in the AUC between any two groups in the matched cohort (P > 0.05).
Conclusions
Glucocorticoids did not impact the performance of sCysC in identifying AKI in critically ill patients.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12882-020-02165-1.
Keywords: Acute kidney injury, Cystatin C, Intensive care unit, Renal biomarker
Key messages
● Glucocorticoids could induce an increase in sCysC levels. However, the relationship between the sCysC and glucocorticoids was not manifested in a dose-dependent manner.
● Glucocorticoids did not have a statistically significant effect on the performance of sCysC in detecting AKI in critically ill patients.
Background
Acute kidney injury (AKI) is an alarming burden in critically ill patients with a high incidence and independently impacts prognosis [1–4]. The therapeutic outcome of AKI is unsatisfactory as the initiation of effective treatments are started relatively late after a noticeable elevation in serum creatinine (SCr) [5, 6]. In this context, the exploration of an early biomarker could significantly improve the prognosis of AKI.
Cystatin C (CysC), a cysteine proteinase inhibitor, is freely filtered by the glomerulus and entirely reabsorbed by the proximal tubules [7–9]. Contrast to SCr, the concentrations of serum cystatin C (sCysC) show a small individual variability as nonrenal factors only slightly influenced it [8, 9].. Therefore, sCysC may be superior to SCr in detecting a minimal change in the glomerular filtration rate (GFR) [7, 10, 11]. Previous studies showed that it might be a potential biomarker for the early detection of AKI [12–16].
However, as sCysC is widely used in clinical application, many studies reported other factors that might interfere with its concentrations beyond renal function, such as glucocorticoid therapy, thyroid function, and glycemic status [17–22]. CysC is produced by all nucleated cells in the human body at a relatively constant rate [7, 8]. However, it was shown that glucocorticoids could stimulate the production of CysC in vitro [23]. Moreover, glucocorticoid medication would also increase sCysC concentrations in experimental animals, such as rats and dogs [24, 25]. Glucocorticoids have extensive applications in human medicine because of its functions of anti-inflammation and immunosuppression. Many studies already suggested that glucocorticoids could impact sCysC concentrations independently of renal function in patients [26–29]. However, it remains undefined whether glucocorticoids influence sCysC to detect AKI in critically ill patients.
Therefore, this prospective, observational, propensity-matched study was performed in a large critically ill cohort to illuminate whether glucocorticoids impacted the diagnostic and predictive accuracy of sCysC in detecting AKI.
Methods
Study design and participants
This prospective observational study was undertaken in the general intensive care unit (ICU) of Guangdong Provincial People’s Hospital from October 2014 to December 2017. Patients aged 18 years or older admitted to ICU were enrolled for the study. The exclusion criteria incorporated preexisting Cushing syndrome or adrenocortical hypofunction, end-stage renal disease (ESRD) or undergoing renal replacement therapy (RRT) before admission, renal transplantation or nephrectomy, missing clinical data or refusal of consent. The primary outcome of this study was the diagnosis of AKI within 1 week after ICU admission, and the secondary outcomes included length of ICU and hospital stay, as well as ICU and hospital mortality. The protocol was followed according to that of the Strengthening the Reporting of Observational Studies in Epidemiology [30] and Standards for Reporting Diagnostic Accuracy [31] criteria. The current study received the approval of ethics committee of the Guangdong Provincial People’s Hospital and all methods were performed in accordance with the relevant guidelines and regulations. Written informed consent was obtained from each participant or a family member at the time of enrollment.
Data collection
We prospectively collected patients’ baseline clinical data. All serum samples for determining SCr, sCysC, and serum albumin were collected concurrently within 1 h after ICU admission. SCr was measured at least once a day as a part of routine clinical care during ICU hospitalization. The following demographic and clinical characteristics were collected: age, sex, body mass index (BMI), preexisting clinical conditions, previous glucocorticoid administration within 5 days before entering ICU, admission type, baseline SCr, baseline-estimated glomerular filtration rate (eGFR), SCr at ICU admission, serum albumin and Acute Physiology and Chronic Health Evaluation II (APACHE II) score at ICU admission. The outcome variables were documented, including the occurrence of AKI within 1 week after ICU admission, length of ICU stay, length of hospital stay, ICU mortality, and in-hospital mortality. We calculated the eGFR based on the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) creatinine equation [32].
Definitions
AKI was diagnosed according to the Kidney Disease Improving Global Outcomes (KDIGO) criteria as any of the following: increase in SCr by 0.3 mg/dl (26.5 mmol/l) within 48 h, increase in SCr to 1.5 times of the baseline level within 1 week, or urine output < 0.5 mL/kg/h for 6 h [33]. Because of insufficient sensitivity of urine output in diuretics administration, we diagnosed AKI based on SCr [34]. We determined the baseline SCr according to the following rules ranked in descending order of preference [35]: (1) the most recent pre-ICU value between 30 and 365 days before ICU admission; (2) a stable pre-ICU value > 365 days for patients aged < 40 years (stable defined as within 15% of the lowest ICU measurement) before ICU admission; (3) pre-ICU value > 365 days before ICU admission and less than the initial SCr at ICU admission; (4) a pre-ICU value (between 3 and 39 days before ICU admission) less than or equal to the initial on-admission SCr to ICU and not distinctly during AKI; (5) the lowest SCr upon initial admission to ICU, the last ICU value, or the minimum value at follow-up to 365 days. Established AKI and later-onset AKI were diagnosed if patients reached the KDIGO criteria at ICU admission or within 1 week after ICU admission, respectively. Mild AKI was defined as KDIGO stage 1 and severe AKI was defined as stage 2 or stage 3 of KDIGO criteria [33, 36].
Patient groups
Thus far, previous studies showed that there was a significant correlation between sCysC levels and glucocorticoids in the first 5 days after the administration of glucocorticoids [28, 29]. Therefore, the patients were divided into four groups based on accumulated doses of glucocorticoids within 5 days before admission to ICU: Group I (non-users), Group II (0 mg < prednisone ≤50 mg), Group III (50 mg < prednisone ≤150 mg), Group IV (prednisone > 150 mg). As attested by potency and duration of action of glucocorticoids, we used this dosage calculation, 4 mg/day of methylprednisolone and 0.75 mg/day of dexamethasone was equal to a dosage of 5 mg/day of prednisone [37].
Laboratory methods
All samples were measured within 24 h after collection at the central laboratory of the Guangdong Provincial People’s Hospital. SCr, sCysC, and serum albumin were measured using a UniCel DxC 800 Synchron System (Beckman Coulter, CA, USA). sCysC was measured by immunoturbidimetry, the coefficients of inter-assay and intraassay variations for which were ≤ 5% and ≤ 10%, respectively.
Statistical analysis
To avoid potential confounders and selection biases caused by nonrandomized in this study, we used the propensity score matching. We generated the propensity score for each patient according to the probability of receiving glucocorticoids produced by multivariable logistic regression analysis model. The multivariable logistic regression analysis model (P < 0.001; Hosmer and Lemeshow goodness-of-fit test, P = 0.935) obtained the following covariates: age, sex, BMI, APACHE II score, serum albumin, baseline eGFR, diabetes mellitus (DM), hypertension, chronic kidney disease (CKD), coronary heart disease (CHD), chronic heart failure (CHF), stroke, malignancy, chronic obstructive pulmonary disease (COPD), chronic liver disease, admission type, and grade of AKI. And then, we used the propensity score to match glucocorticoid users with non-users at a ratio of 1:4 using nearest neighbor matching. Patients without a corresponding match were excluded. After all propensity score matches were completed, we evaluated the balance in baseline variates. Propensity score matching was performed using SPSS version 23.0 (SPSS, USA, IL).
A two-tailed P value< 0.05 was considered statistically significant. All continuous variables did not follow normal distribution as tested by SPSS software. Continuous variables were reported as median (interquartile range, IQR) and compared using the Wilcoxon rank-sum test. Categorical variables were reported as absolute value (percentage) and compared using the chi-square test or Fisher’s exact test. The bivariate correlation analysis was used to assess the association between two variables. Multivariable linear regression analysis with a stepwise variable selection was also used to assess the relationship between sCysC and other variables. A receiver operating characteristic (ROC) curve analysis was generated, and the area under the curve (AUC) in each group as assessed using the Hanley–McNeil method, and the optimal cutoff value for AKI detection was determined with the Youden’s index. All statistical analyses were performed using SPSS version 23.0 (SPSS, IL, USA) and MedCalc version 18.2.1 (MedCalc Software, Ostend, Belgium) software programs.
Results
Patient characteristics and outcomes
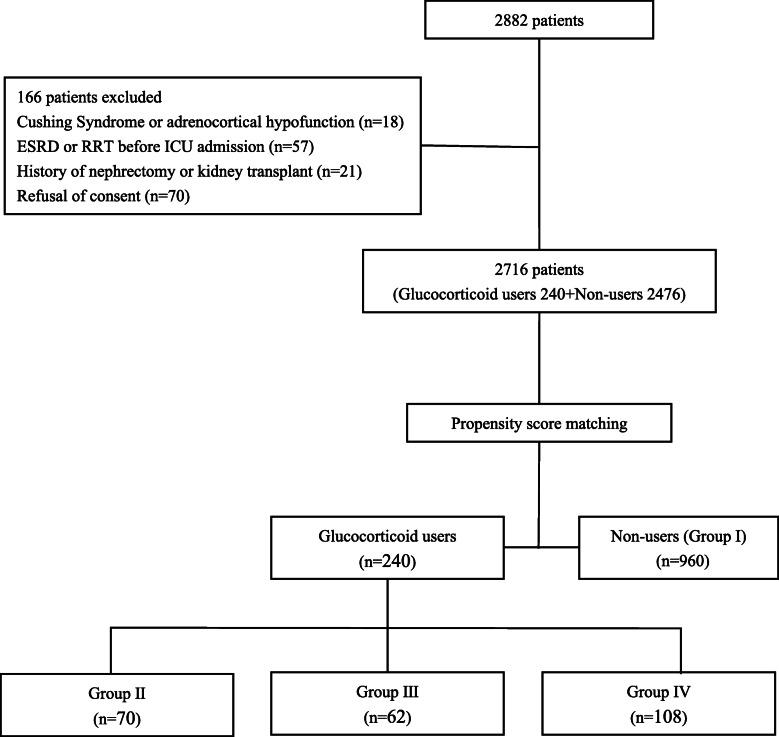
There were 2716 patients got engaged in this study (Fig. 1). A total of 166 patients were excluded. Glucocorticoids were prescribed for 8.8% (240/2716) of patients. In total, 23.3% of patients (634/2716) met the diagnostic criteria of AKI, including patients accounted for 34.9% (221/634) occurred established AKI, and patients accounted for 65.1% (413/634) developed later-onset AKI.
Fig. 1.
Recruitment of patients into the study. ESRD: End-stage renal disease; ICU: Intensive care unit; n: Sample size; RRT: Renal replacement therapy. Group I was defined as the cumulative doses of prednisone within 5 days before admission to ICU was equal to 0 mg. Group II was defined as the cumulative doses of prednisone within 5 days before admission to ICU were greater than 0 mg and less than or equal to 50 mg. Group III was defined as the cumulative doses of prednisone within 5 days before admission to ICU were greater than 50 mg and less than or equal to 150 mg. Group IV was defined as the cumulative doses of prednisone within 5 days before admission to ICUs were greater than 150 mg
Table 1 shows the characteristics of the patients. Compared with patients who were not prescribed glucocorticoids, users were more likely to have a higher APACHE II score (11 vs. 9, P < 0.001), and had a significantly higher percentage of comorbidities, including malignancy (27.9% vs. 14.7%, P < 0.001), COPD (5.4% vs. 1.8%, P < 0.001) and chronic liver disease (2.9% vs 1.0%, P = 0.017). Moreover, there was a significant difference between glucocorticoid users and non-users in admission type. Patients using glucocorticoids were more likely to suffer from more severe AKI.
Table 1.
Baseline data and outcomes
| Variables | Before matching | After matching | ||||
|---|---|---|---|---|---|---|
| Corticosteroid users (n = 240) | Non-users (n = 2476) | P value | Corticosteroid users (n = 240) | Non-users (n = 960) | P value | |
| Cumulative dose of prednisone, mg | 133.3 (50.0–300.0) | 0 | 133.3 (50.0–300.0) | 0 | ||
| Baseline characteristics | ||||||
| Age, years | 55.0 (44.0–65.0) | 55.0 (43.0–65.0) | 0.949 | 55.0 (44.0–65.0) | 54.0 (40.0–67.0) | 0.800 |
| Male sex, n (%) | 158 (65.8) | 1280 (51.7) | < 0.001 | 158 (65.8) | 615 (64.1) | 0.608 |
| BMI, kg/m2 | 22.46 (20.77–24.95) | 22.32 (20.70–24.44) | 0.506 | 22.46 (20.77–24.95) | 22.45 (20.95–24.46) | 0.986 |
| Preexisting clinical conditions | ||||||
| Hypertension, n (%) | 46 (19.2) | 476 (19.2) | 0.983 | 46 (19.2) | 177 (18.4) | 0.795 |
| DM, n (%) | 21 (8.8) | 208 (8.4) | 0.852 | 21 (8.8) | 82 (8.5) | 0.918 |
| CKD, n (%) | 12 (5.0) | 90 (3.6) | 0.288 | 12 (5.0) | 45 (4.7) | 0.839 |
| CHD, n (%) | 8 (3.3) | 94 (3.8) | 0.719 | 8 (3.3) | 29 (3.0) | 0.802 |
| Stroke, n (%) | 24 (10.0) | 326 (13.2) | 0.162 | 24 (10.0) | 106 (11.0) | 0.642 |
| CHF, n (%) | 8 (3.3) | 62 (2.5) | 0.439 | 8 (3.3) | 27 (2.8) | 0.668 |
| Malignancy, n (%) | 67 (27.9) | 364 (14.7) | < 0.001 | 67 (27.9) | 256 (26.7) | 0.696 |
| COPD, n (%) | 13 (5.4) | 45 (1.8) | < 0.001 | 13 (5.4) | 35 (3.6) | 0.211 |
| Chronic liver disease, n (%) | 7 (2.9) | 24 (1.0) | 0.017 | 7 (2.9) | 19 (2.0) | 0.372 |
| Admission type | < 0.001 | 0.258 | ||||
| Elective surgical, n (%) | 155 (64.6) | 1887 (76.2) | 155 (64.6) | 650 (67.7) | ||
| Emergency surgical, n (%) | 17 (7.1) | 205 (8.3) | 17 (7.1) | 84 (8.8) | ||
| Medical, n (%) | 68 (28.3) | 384 (15.5) | 68 (28.3) | 226 (23.5) | ||
| Baseline eGFR, ml/min/1.73 m2 | 103.70 (89.81–115.39) | 100.23 (85.83–112.60) | 0.036 | 103.70 (89.81–115.39) | 103.19 (88.62–116.34) | 0.875 |
| Baseline SCr, umol/L | 63.85 (54.00–76.53) | 65.00 (53.36–79.69) | 0.639 | 63.85 (54.00–76.53) | 64.00 (51.60–79.50) | 0.742 |
| SCr at ICU admission umol/L | 76.17 (64.00–92.15) | 73.00 (59.40–91.80) | 0.056 | 76.17 (64.00–92.15) | 76.00 (60.03–96.00) | 0.708 |
| Serum albumin, g/L | 30.45 (26.60–33.80) | 31.60 (27.50–35.00) | 0.001 | 30.45 (26.60–33.80) | 30.30 (26.36–34.00) | 0.999 |
| APACHE II score | 11 (7.0–18.0) | 9 (6.0–14.0) | < 0.001 | 11.0 (7.0–18.0) | 11 (7.0–16.0) | 0.537 |
| Primary outcomes | ||||||
| Total AKI, n (%) | 88 (36.7) | 546 (22.1) | < 0.001 | 88 (36.7) | 334 (34.8) | 0.586 |
| Established AKI, n (%) | 29 (12.1) | 192 (7.8) | 0.019 | 29 (12.1) | 128 (13.3) | 0.608 |
| Later-onset AKI, n (%) | 59 (24.6) | 354 (14.3) | < 0.001 | 59 (24.6) | 206 (21.5) | 0.297 |
| Grade of AKI, | < 0.001 | 0.486 | ||||
| Non-AKI, n (%) | 152 (63.3) | 1930 (77.9) | 152 (63.3) | 626 (65.2) | ||
| Mild AKI, n (%) | 50 (20.8) | 351 (14.2) | 50 (20.8) | 205 (21.4) | ||
| Severe AKI, n (%) | 38 (15.8) | 195 (7.9) | 38 (15.8) | 129 (13.4) | ||
The non-normally distributed continuous variables are expressed as median (25th percentile to 75th percentile [interquartile range]). Categorical variables are expressed as n (%)
APACHE II score Acute Physiology and Chronic Health Evaluation II score; AKI Acute kidney injury; BMI Body mass index; CKD Chronic kidney disease; CHD Coronary heart disease; CHF Chronic heart failure; COPD Chronic obstructive pulmonary disease; DM Diabetes mellitus; eGFR Estimated glomerular filtration rate; ICU Intensive care unit; KDIGO Kidney Disease: Improving Global Outcomes; n Sample size; SCr Serum creatinine; Established AKI, defined as diagnosis of AKI at ICU admission; Later-onset AKI, indicated no AKI diagnosis at ICU admission but reaching the KDIGO criteria within 1 week after admission; Mild-AKI: defined as reaching KDIGO stage 1 diagnostic criteria of AKI; Severe-AKI, defined as reaching KDIGO stage 2 or stage 3 diagnostic criteria of AKI
P value for global comparisons among groups by rank sum test and chi-square test for continuous and categorical variables, respectively
Factors associated with sCysC
The results of bivariate correlations analysis indicated a significant, but weak, correlation between sCysC and previous use of glucocorticoids (correlation coefficient = 0.074, P < 0.001) (Table 2). In multivariable linear regression analysis (Table 3), we found the same association between sCysC and previous use of glucocorticoids (standardized β = 0.092, P = 0.003). There was also an association between the cumulative dose of steroids and cystatin C in the above two types of correlation analysis. Besides, the correlation and regression analyses demonstrated that other factors also were associated with sCysC. Therefore, we used the propensity score matching to eliminate their impacts.
Table 2.
Factors associated with sCysC using bivariate correlation analysis
| Variables | Correlation coefficient | P |
|---|---|---|
| Spearman method | ||
| Age, years | 0.391 | < 0.001 |
| BMI, kg/m2 | 0.029 | 0.134 |
| Baseline eGFR, ml/minute/1.73 m2 | − 0.477 | < 0.001 |
| Baseline SCr, umol/L | 0.438 | < 0.001 |
| SCr at ICU admission, umol/L | 0.569 | < 0.001 |
| Cumulative dose of prednisone, mg | 0.152 | < 0.001 |
| Serum albumin, g/L | −0.118 | < 0.001 |
| APACHE II score | 0.397 | < 0.001 |
| Grade of AKI, n (%) | 0.414 | < 0.001 |
| Point-biserial method | ||
| Male sex, n (%) | 0.164 | < 0.001 |
| Previous use of glucocorticoids, n (%) | 0.074 | < 0.001 |
| Hypertension, n (%) | 0.255 | < 0.001 |
| DM, n (%) | 0.182 | < 0.001 |
| CKD, n (%) | 0.473 | < 0.001 |
| CHD, n (%) | 0.160 | < 0.001 |
| Stroke, n (%) | 0.108 | < 0.001 |
| CHF, n (%) | 0.207 | < 0.001 |
| Malignancy, n (%) | −0.003 | 0.889 |
| COPD, n (%) | 0.111 | < 0.001 |
| Chronic Liver disease, n (%) | 0.043 | 0.026 |
APACHE II score Acute Physiology and Chronic Health Evaluation II score; AKI Acute kidney injury; BMI Body mass index; CKD Chronic kidney disease; CHD Coronary heart disease; CHF Chronic heart failure; COPD Chronic obstructive pulmonary disease; DM Diabetes mellitus; eGFR Estimated glomerular filtration rate; ICU Intensive care unit; KDIGO Kidney Disease: Improving Global Outcomes; n Sample size; SCr Serum creatinine; Mild-AKI: defined as reaching KDIGO stage 1 diagnostic criteria of AKI; Severe-AKI, defined as reaching KDIGO stage 2 or stage 3 diagnostic criteria of AKI
Table 3.
Factors associated with sCysC using multivariate linear regression analysis
| Independent variables | sCysC at ICU admission, mg/L | |
|---|---|---|
| Standardized β | P | |
| Baseline SCr, umol/L | 0.002 | < 0.001 |
| SCr at ICU admission, umol/L | 0.004 | < 0.001 |
| Grade of AKI | 0.183 | < 0.001 |
| APACHE II score | 0.009 | < 0.001 |
| Baseline eGFR, ml/min/1.73 m2 | − 0.003 | < 0.001 |
| Admission type | −0.105 | < 0.001 |
| CKD, n (%) | 0.227 | < 0.001 |
| Previous use of glucocorticoids, n (%) | 0.092 | 0.003 |
| Cumulative dose of prednisone, mg | 0.0002 | 0.028 |
| Serum albumin, g/L | −0.004 | 0.001 |
| CHD, n (%) | 0.118 | 0.001 |
| Age | 0.001 | 0.049 |
| Constant | 0.702 (Unstandardized) | < 0.001 |
APACHE II score Acute Physiology and Chronic Health Evaluation II score; AKI Acute kidney injury; BMI Body mass index; CKD Chronic kidney disease; CHD Coronary heart disease; CHF Chronic heart failure; COPD Chronic obstructive pulmonary disease; DM Diabetes mellitus; eGFR Estimated glomerular filtration rate; ICU Intensive care unit; KDIGO Kidney Disease: Improving Global Outcomes; n Sample size; SCr Serum creatinine; Mild-AKI: defined as reaching KDIGO stage 1 diagnostic criteria of AKI; Severe-AKI, defined as reaching KDIGO stage 2 or stage 3 diagnostic criteria of AKI
Independent variables included: baseline SCr, SCr at ICU admission, previous use of glucocorticoids, cumulative dose of prednisone, APACHE II score, grade of AKI, admission type, malignancy, stoke, hypertension, DM, CHD, CHF, COPD, chronic Liver disease, CKD, Albumin at admission, BMI, eGFR, sex, age. Variables not listed in the table were removed from the stepwise analysis. Adjusted R square 0.776
Propensity score match
Based on the propensity score of each patient, 240 glucocorticoid users were successfully matched to 960 non-users (Table 1). There were no significant differences in the baseline characteristics between the matched glucocorticoid users and non-users.
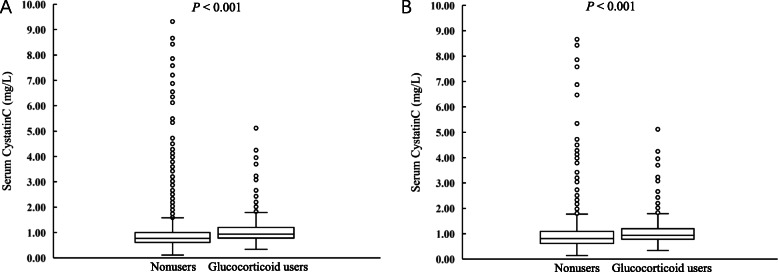
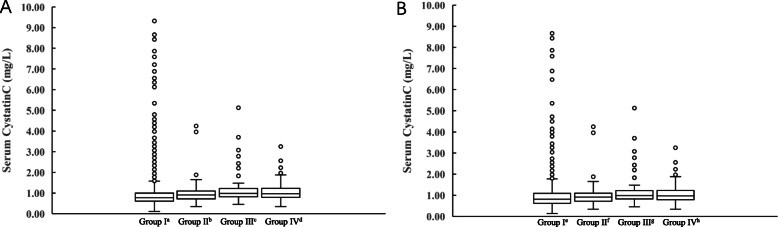
The concentrations of sCysC in different groups
We found a significant difference in sCysC levels between glucocorticoid users and non-users (0.940 mg/L vs 0.810 mg/L; P < 0.001), although sCysC levels were elevated moderately (Fig. 2). Before matching, sCysC levels were statistically significantly lower in group I than the other three groups (P < 0.05), and the sCysC levels of different glucocorticoids recipient groups were not different (P > 0.05). After matching, there were the same results in the different glucocorticoids recipient groups (P > 0.05), but the sCysC levels of group I were significantly lower than the sCysC levels in group III or group IV (P < 0.05) (Fig. 3).
Fig. 2.
The median of sCysC levels in patients with and without glucocorticoid treatment. a Glucocorticoid users had higher levels of sCysC before matching (0.940 mg/L vs 0.770 mg/L; P < 0.001). b Glucocorticoid users had higher levels of sCysC after matching (0.940 mg/L vs 0.810 mg/L; P < 0.001)
Fig. 3.
The concentration of sCysC in different groups. Grouping of standards was according to cumulative doses of glucocorticoids within 5 days before admission to ICU: Group I: non-users; Group II: 0 mg < prednisone ≤50 mg; Group III: 50 mg < prednisone ≤150 mg; Group IV: prednisone > 150 mg; a Before matching: a: group I vs. group II P < 0.05, vs. group III P < 0.05, and vs. group IV P < 0.05; b: group II vs. group I P < 0.05, vs. group III P > 0.05, and vs. group IV P > 0.05; c: group III vs. group I P < 0.05, vs. group II P > 0.05, and vs. group IV P > 0.05; d: group IV vs. group I P < 0.05, vs. group II P > 0.05, and vs. group III P > 0.05. b After matching: e: group I vs. group II P > 0.05, vs. group III P < 0.05, and vs. group IV P < 0.05; f: group II vs. group I P > 0.05, vs. group III P > 0.05, and vs. group IV P > 0.05; g: group III vs. group I P < 0.05, vs. group II P > 0.05, and vs. group IV P > 0.05; h: group IV vs. group I P < 0.05, vs. group II P > 0.05, and vs. group III P > 0.05
Detection of AKI by sCysC concerning different glucocorticoids doses
Table 4 shows the AUC-ROC analysis for the performance of sCysC to detect AKI in different groups. Before matching, the AUC calculated by sCysC for the entire cohort was 0.769, 0.810, and 0.748 for total AKI, established AKI, and later-onset AKI respectively (Additional file 1: Fig. S1). After matching, the AUC calculated by sCysC for the entire cohort was 0.758, 0.802, and 0.732 for detecting total AKI, established AKI, and later-onset AKI respectively (Additional file 1: Fig. S1).
Table 4.
Detection of AKI using sCysC by different groups
| Total AKI | Established AKI | Later-on AKI | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AUC ROC | 95%CI | Cutoff | P | AUC ROC | 95%CI | Cutoff | P | AUC ROC | 95%CI | Cutoff | P | |
| Before matching | ||||||||||||
| Total | 0.769 ± 0.011 | 0.753–0.785 | 1.00 | < 0.001 | 0.810 ± 0.017 | 0.793–0.826 | 0.93 | < 0.001 | 0.748 ± 0.014 | 0.730–0.765 | 1.02 | < 0.001 |
| Group I | 0.769 ± 0.012 | 0.752–0.786 | 1.00 | < 0.001 | 0.810 ± 0.018 | 0.793–0.827 | 0.93 | < 0.001 | 0.747 ± 0.015 | 0.729–0.765 | 1.02 | < 0.001 |
| Group II | 0.733 ± 0.060 | 0.613–0.831 | 1.00 | < 0.001 | 0.760 ± 0.086 | 0.622–0.868 | 1.04 | 0.003 | 0.714 ± 0.072 | 0.580–0.825 | 1.00 | 0.003 |
| Group III | 0.736 ± 0.064 | 0.609–0.840 | 1.21 | < 0.001 | 0.781 ± 0.085 | 0.631–0.891 | 1.48 | 0.001 | 0.712 ± 0.078 | 0.569–0.829 | 1.09 | 0.007 |
| Group IV | 0.724 ± 0.061 | 0.629–0.805 | 1.36 | < 0.001 | 0.779 ± 0.077 | 0.676–0.862 | 0.99 | < 0.001 | 0.707 ± 0.074 | 0.608–0.793 | 1.64 | 0.005 |
| After matching | ||||||||||||
| Total | 0.758 ± 0.015 | 0.733–0.782 | 1.09 | < 0.001 | 0.802 ± 0.021 | 0.775–0.827 | 0.98 | < 0.001 | 0.732 ± 0.019 | 0.704–0.759 | 1.09 | < 0.001 |
| Group I | 0.768 ± 0.017 | 0.740–0.794 | 0.95 | < 0.001 | 0.812 ± 0.023 | 0.782–0.839 | 0.98 | < 0.001 | 0.740 ± 0.021 | 0.709–0.770 | 0.95 | < 0.001 |
| Group II | 0.733 ± 0.060 | 0.613–0.831 | 1.00 | < 0.001 | 0.760 ± 0.086 | 0.622–0.868 | 1.04 | 0.003 | 0.714 ± 0.072 | 0.580–0.825 | 1.00 | 0.003 |
| Group III | 0.736 ± 0.064 | 0.609–0.840 | 1.21 | < 0.001 | 0.781 ± 0.085 | 0.631–0.891 | 1.48 | 0.001 | 0.712 ± 0.078 | 0.569–0.829 | 1.09 | 0.007 |
| Group IV | 0.724 ± 0.061 | 0.629–0.805 | 1.36 | < 0.001 | 0.779 ± 0.077 | 0.676–0.862 | 0.99 | < 0.001 | 0.707 ± 0.074 | 0.608–0.793 | 1.64 | 0.005 |
95% CI 95% Confidence interval; AKI Acute kidney injury; AUC-ROC Area under the receiver operating characteristic curve; ICU Intensive care unit; KDIGO Kidney Disease: Improving Global Outcomes; Established AKI, defined as diagnosis of AKI at ICU admission; Later-onset AKI, indicated no AKI diagnosis at ICU admission but reaching the KDIGO criteria within 1 week after admission;
Grouping of standards was according to cumulative doses of glucocorticoids within 5 days before admission to ICU: Group I: non-users; Group II: 0 mg < prednisone ≤50 mg; Group III: 50 mg < prednisone ≤150 mg; Group IV: prednisone > 150 mg;
Before matching: Total AKI: AUC of Group I vs. AUC of Group II, Z = 0.588, P = 0.556. AUC of Group I vs. AUC of Group III, Z = 0.507, P = 0.612. AUC of Group I vs. AUC of Group IV, Z = 0.724, P = 0.469. AUC of Group II vs. AUC of Group III, Z = −0.034, P = 0.973. AUC of Group II vs. AUC of Group IV, Z = 0.105, P = 0.916. AUC of Group III vs. AUC of Group IV, Z = 0.136, P = 0.892. Established AKI: AUC of Group I vs. AUC of Group II, Z = 0.569, P = 0.569. AUC of Group I vs. AUC of Group III, Z = 0.334, P = 0.739. AUC of Group I vs. AUC of Group IV, Z = 0.392, P = 0.695. AUC of Group II vs. AUC of Group III, Z = − 0.174, P = 0.862. AUC of Group II vs. AUC of Group IV, Z = − 0.165, P = 0.869. AUC of Group III vs. AUC of Group IV, Z = 0.017, P = 0.986. Later-on AKI: AUC of Group I vs. AUC of Group II, Z = 0.449, P = 0.654. AUC of Group I vs. AUC of Group III, Z = 0.441, P = 0.660. AUC of Group I vs. AUC of Group IV, Z = 0.530, P = 0.596. AUC of Group II vs. AUC of Group III, Z = 0.019, P = 0.985. AUC of Group II vs. AUC of Group IV, Z = 0.068, P = 0.946. AUC of Group III vs. AUC of Group IV, Z = 0.047, P = 0.963
After matching: Total AKI: AUC of Group I vs. AUC of Group II, Z = 0.561, P = 0.575. AUC of Group I vs. AUC of Group III, Z = 0.483, P = 0.629. AUC of Group I vs. AUC of Group IV, Z = 0.695, P = 0.487. AUC of Group II vs. AUC of Group III, Z = − 0.034, P = 0.973. AUC of Group II vs. AUC of Group IV, Z = 0.105, P = 0.916. AUC of Group III vs. AUC of Group IV, Z = 0.136, P = 0.892. Established AKI: AUC of Group I vs. AUC of Group II, Z = 0.584, P = 0.559. AUC of Group I vs. AUC of Group III, Z = 0.352, P = 0.725. AUC of Group I vs. AUC of Group IV, Z = 0.411, P = 0.681. AUC of Group II vs. AUC of Group III, Z = − 0.174, P = 0.862. AUC of Group II vs. AUC of Group IV, Z = − 0.165, P = 0.869. AUC of Group III vs. AUC of Group IV, Z = 0.017, P = 0.986. Later-on AKI: AUC of Group I vs. AUC of Group II, Z = 0.347, P = 0.729. AUC of Group I vs. AUC of Group III, Z = 0.347, P = 0.729. AUC of Group I vs. AUC of Group IV, Z = 0.429, P = 0.668. AUC of Group II vs. AUC of Group III, Z = 0.019, P = 0.985. AUC of Group II vs. AUC of Group IV, Z = 0.068, P = 0.946. AUC of Group III vs. AUC of Group IV, Z = 0.047, P = 0.963
The patients were split into four groups based on whether they received glucocorticoid therapy and the accumulated doses of glucocorticoids within 5 days before ICU admission. Before matching, the AUC for sCysC in detecting total AKI was 0.769, 0.733, 0.736 and 0.724 in group I, group II, group III, and group IV respectively. The AUC for sCysC in diagnosing established AKI was 0.810, 0.760, 0.781, and 0.779 in group I, group II, group III, and group IV respectively. The AUC for sCysC in predicting later-onset AKI was 0.747, 0.714, 0.712, 0.707 in group I, group II, group III, and group IV respectively. After matching, the AUC for sCysC in detecting total AKI, established AKI, and later-onset AKI was 0.768, 0.812, and 0.740 respectively in group I; 0.733, 0.760, and 0.714 respectively in group II; 0.736, 0.781, and 0.712 respectively in group III; 0.724, 0.779, and 0.707 respectively in group IV. In summary, we did not observe a significant difference between AUC in any two groups for total AKI, established AKI, and later-onset AKI before and after the matching. Before and after matching, the cutoff values of sCysC in detecting AKI were different in diverse glucocorticoids recipient groups, but the change of cutoff values of sCysC were irregular.
Discussion
In this prospective, propensity-matched cohort study, we evaluated whether glucocorticoids affect the ability of sCysC to detect AKI in critically ill patients. We adopted a propensity score matching to eliminate the influences of potential confounding factors. Before and after matching, we found that the abilities of sCysC in detecting AKI were not different among patients with or without glucocorticoid therapy.
sCysC has an advantage that it might be less influenced by nonrenal factors than SCr [8, 9]. However, many studies have shown conflicting results. These studies suggested that the relationship between GFR and sCysC might have a potential variability due to some nonrenal factors, including age, sex, thyroid hormones, glycemic status, hepatic impairment, as well as glucocorticoids [17–22, 26–29, 38–43]. Bjarnadottir et al. demonstrated in vitro that dexamethasone could lead to CysC level increase by the dose-dependent manner [23]. Recent studies confirmed this in animals [24, 25], and we found similar results in our current study. We found that sCysC level in glucocorticoid users was higher than that in non-users, no matter with or without matching. This phenomenon might be caused by glucocorticoids increasing the transcription of the CysC by induction of the promoter [23]. Alternatively, glucocorticoids have a nephrotoxic effect as its ability of causing metabolic alkalosis and hypertension [44]. This may be another reason why glucocorticoids could lead to an increase in the sCysC level.
Numerous previous clinical studies verified the relationship between sCysC level and glucocorticoids in patients. Cimerman et al. found that sCysC levels were elevated in steroid-independent patients with asthma after 1 week of methylprednisolone treatment [18]. Several studies in renal transplant recipients have also shown that sCysC levels are correlated with glucocorticoids [26–29, 39]. Risch et al. showed that the level of sCysC are positively correlated with the doses of glucocorticoids [26]. However, their study suggested that glucocorticoids did not affect the detection of impaired renal function by sCysC, as their obtained data indicated that sCysC was still more accurate than SCr to assess the renal function in renal transplant patients. Similarly, Pöge et al. found that the highest sCysC levels occurred on day 2 with high-doses of glucocorticoids in renal transplant patients, which suggested changes in sCysC levels develop fast [27]. Furthermore, Mendiluce et al. noticed that the increase of sCysC levels coincides with high-doses glucocorticoid treatment in the first 5 days after renal transplantation and then decreased [28]. Such studies suggested that the change of sCysC levels might be reversible. Some studies further demonstrated that sCysC could underestimate GFR resulted from this association [26, 39, 45]. Le Bricon et al. suggested that sCysC underestimated GFR in 14% in 3 months after renal transplantation [45]. Therefore, sCysC may be of limited value in assessing renal function in the case of using glucocorticoids due to underestimating of GFR. However, a recent study by Silva et al. did not observe such interference in lupus nephritis patients undergoing glucocorticoid therapy [46]. They speculated that the gene that codifies CysC was already activated by the induction because lupus nephritis patients used glucocorticoid medication for a long time. Another study had a discrepant conclusion from a study performed by Cimerman et al. in patients with asthma. However, the glucocorticoids treatment is provided by inhalation, but not systemic use [47]. Previous studies also supported that glucocorticoids not only could raise sCysC levels but also are associated in a dose-dependent manner with increased sCysC [26, 39]. In the present study, a multiple linear regression analysis showed that glucocorticoid uses were independently correlated with sCysC. After using the statistical approach of propensity score matching, we demonstrated that the elevation of sCysC levels was related to higher doses of glucocorticoids. However, we did not observe a dose-dependent relationship between the doses of glucocorticoids and sCysC levels. Accumulating evidences suggest that glucocorticoids may have a role in interfering with sCysC concentrations. Therefore, we can not exclude the possibility that using glucocorticoids may impact the value of sCysC as a marker of AKI.
As previous and present studies suggested, glucocorticoids induce an elevation of sCysC levels. So, we designed this study to solve the problem of whether the glucocorticoids could impact the performance of sCysC in detecting AKI. The results suggested that glucocorticoids had no statistically significant effect on sCysC in diagnosing and predicting AKI. We suspect that this phenomenon might be a result of the increased sCysC caused by glucocorticoids is only temporary and finite.
This study was not without limitations. First, we used propensity score matching to minimize the effects of potential confounders and selection bias caused by the nonrandom allocation to either the glucocorticoid users or non-users group. Nevertheless, this approach might still have limitations in balancing these factors between the two groups. Second, because our study was not an interventional trial, and we measured sCysC only once at ICU admission, we could not evaluate how long after withholding glucocorticoid therapy sCysC levels are affected. Third, this study did not reveal the rule of change of sCysC cutoff value for AKI detection when patients received glucocorticoid medication. We thought a larger sample size of glucocorticoid users was needed to reveal this rule.
Conclusion
Glucocorticoids did not impact the performance of sCysC in identifying AKI in critically ill patients, although the levels of sCysC might be slightly affected by glucocorticoid treatment.
Supplementary Information
Additional file 1:Fig. S1 Performance of sCysC for AKI detection before and after matching. A Performance of sCysC for total AKI detection before and after matching; B Performance of sCysC for established AKI detection before and after matching; C Performance of sCysC for later-onset AKI detection before and after matching; Established AKI, defined as diagnosis of AKI at ICU admission; Later-onset AKI, indicated no AKI diagnosis at ICU admission but reaching the KDIGO criteria within 1 week after admission; AKI: Acute kidney injury; ICU: Intensive care unit; KDIGO: Kidney Disease: Improving Global Outcomes;
Acknowledgements
The authors thank all the doctors, nurses, technicians, and patients at the Guangdong Provincial People’s Hospital for their dedication in the study.
Abbreviations
- 95% CI
95% Confidence interval
- AKI
Acute kidney injury
- APACHE II
Acute physiology and chronic health evaluation II score
- AUC
Area under the receiver operating characteristic curve
- BMI
Body mass index
- CHD
Coronary heart disease
- CHF
Chronic heart failure
- CKD
Chronic kidney disease
- COPD
Chronic obstructive pulmonary disease
- CysC
Cystatin C
- DM
Diabetes mellitus
- eGFR
Estimated glomerular filtration rate
- EPI
Epidemiology collaboration
- ESRD
End-stage renal disease
- GFR
Glomerular filtration rate
- ICU
Intensive care unit
- KDIGO
Kidney disease: improving global outcomes
- n
Sample size
- ROC
Receiver operating characteristic curve
- RRT
Renal replacement therapy
- SCr
Serum creatinine
- sCysC
Serum cystatin C
Authors’ contributions
CBC, SLL MS, and YPB equally contributed to the design of the research. SLL and YPB equally contributed to analyze and interpret the data. CBC and MS contributed to the conception of the research and critically revised the manuscript. SLL, MS, YPB, YJD, MXF, JXL, YJW, WYP, YTH, HF, and HDZ performed the research and collected data. All authors contributed to the acquisition and analysis of the data, drafted the manuscript, and agree to be fully accountable for ensuring the integrity and accuracy of the work. All authors read and approved the final manuscript.
Funding
The study was supported by Chunbo Chen’s research grants from the National Natural Science Foundation of China [81671963], the Science and Technology Planning Project of Guangdong Province (Key Program) [2014B020212023], the Guangzhou Livelihood Science and Technology Program [201803010058], and Yujun Deng’s research grant from the Science and Technology Planning Project of Guangdong Province [2016A020215129].
Availability of data and materials
The datasets generated and/or analyzed during this study are not publicly available, owing to currently ongoing research studies, but the data are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The current study received the approval of ethics committee of the Guangdong Provincial People’s Hospital. The ethics committee of the Guangdong Provincial People’s Hospital supervised the study, including the study design, protocol, ethical issue, and data and sample collection. Written informed consent was obtained from each patient or from the appropriate guardian.
Consent for publication
Not applicable. No individual personal data are included in the study. All patients provided necessary consent to participate in the present study.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Silin Liang, Mai Shi and Yunpeng Bai contributed equally to this study, Co-first author.
Contributor Information
Silin Liang, Email: 923700746@qq.com.
Mai Shi, Email: shimai910703@163.com.
Yunpeng Bai, Email: bypnenu@126.com.
Yujun Deng, Email: icudeng@163.com.
Miaoxian Fang, Email: 23633910@qq.com.
Jiaxin Li, Email: lijiaxin@gdph.org.cn.
Yijin Wu, Email: wuyijin_ggh@163.com.
Wenying Peng, Email: pp19790908@163.com.
Yating Hou, Email: stuythou@163.com.
Heng Fang, Email: 1330928062@qq.com.
Huidan Zhang, Email: 529245452@qq.com.
Chunbo Chen, Email: gghccm@163.com.
References
- 1.RPd S, ARS C, LAB P, Ronco C, Macedo E. An epidemiologic overview of acute kidney injury in intensive care units. Rev Assoc Méd Bras. 2019;65:1094–1101. doi: 10.1590/1806-9282.65.8.1094. [DOI] [PubMed] [Google Scholar]
- 2.Negi S, Koreeda D, Kobayashi S, Yano T, Tatsuta K, Mima T, et al. Acute kidney injury: epidemiology, outcomes, complications, and therapeutic strategies. Semin Dial. 2018;31(5):519–527. doi: 10.1111/sdi.12705. [DOI] [PubMed] [Google Scholar]
- 3.Hoste EAJ, Bagshaw SM, Bellomo R, Cely CM, Colman R, Cruz DN, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41(8):1411–1423. doi: 10.1007/s00134-015-3934-7. [DOI] [PubMed] [Google Scholar]
- 4.Folkestad T, Brurberg KG, Nordhuus KM, Tveiten CK, Guttormsen AB, Os I, et al. Acute kidney injury in burn patients admitted to the intensive care unit: a systematic review and meta-analysis. Crit Care. 2020;24(1):2. doi: 10.1186/s13054-019-2710-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jo SK, Rosner MH, Okusa MD. Pharmacologic treatment of acute kidney injury: why drugs haven’t worked and what is on the horizon. Clin J Am Soc Nephrol. 2007;2(2):356–365. doi: 10.2215/CJN.03280906. [DOI] [PubMed] [Google Scholar]
- 6.Pakula AM, Skinner RA. Acute kidney injury in the critically ill patient:a current review of the literature. J Intensive Care Med. 2016;31(5):319–324. doi: 10.1177/0885066615575699. [DOI] [PubMed] [Google Scholar]
- 7.Randers E, Erlandsen EJ. Serum cystatin C as an endogenous marker of the renal function--a review. Clin Chem Lab Med. 1999;37(4):389–395. doi: 10.1515/CCLM.1999.064. [DOI] [PubMed] [Google Scholar]
- 8.Ostermann M, Joannidis M. Acute kidney injury 2016: diagnosis and diagnostic workup. Crit Care. 2016;20(1):299. doi: 10.1186/s13054-016-1478-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teo SH, Endre ZH. Biomarkers in acute kidney injury (AKI) Best Pract Res Clin Anaesthesiol. 2017;31(3):331–344. doi: 10.1016/j.bpa.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 10.Dharnidharka VR, Kwon C, Stevens G. Serum cystatin C is superior to serum creatinine as a marker of kidney function: a meta-analysis. Am J Kidney Dis. 2002;40(2):221–226. doi: 10.1053/ajkd.2002.34487. [DOI] [PubMed] [Google Scholar]
- 11.Laterza OF. Price CP, Scott MG. Cystatin C: an improved estimator of glomerular filtration rate? Clin Chem. 2002;48(5):699–707. doi: 10.1093/clinchem/48.5.699. [DOI] [PubMed] [Google Scholar]
- 12.Herget-Rosenthal S, Marggraf G, Husing J, Goring F, Pietruck F, Janssen O, et al. Early detection of acute renal failure by serum cystatin C. Kidney Int. 2004;66(3):1115–1122. doi: 10.1111/j.1523-1755.2004.00861.x. [DOI] [PubMed] [Google Scholar]
- 13.Charlton JR, Portilla D, Okusa MD. A basic science view of acute kidney injury biomarkers. Nephrol Dial Transplant. 2014;29(7):1301–1311. doi: 10.1093/ndt/gft510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deng Y, Chi R, Chen S, Ye H, Yuan J, Wang L, et al. Evaluation of clinically available renal biomarkers in critically ill adults: a prospective multicenter observational study. Crit Care. 2017;21(1):46. doi: 10.1186/s13054-017-1626-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deng Y, Yuan J, Chi R, Ye H, Zhou D, Wang S, et al. The incidence, risk factors and outcomes of postoperative acute kidney injury in neurosurgical critically ill patients. Sci Rep. 2017;7(1):4245. doi: 10.1038/s41598-017-04627-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deng Y, Ma J, Hou Y, Zhou D, Hou T, Li J, et al. Combining serum Cystatin C and urinary N-acetyl-Beta-D-Glucosaminidase improves the precision foracute kidney injury diagnosis after resection of intracranial space-occupying lesions. Kidney Blood Press Res. 2020;45(1):142-56. [DOI] [PubMed]
- 17.Manetti L, Genovesi M, Pardini E, Grasso L, Lupi I, Linda Morselli L, et al. Early effects of methylprednisolone infusion on serum cystatin C in patients with severe Graves' ophthalmopathy. Clin Chim Acta. 2005;356(1):227–228. doi: 10.1016/j.cccn.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 18.Cimerman N, Brguljan PM, Krašovec M, Šuškovič S, Kos J. Serum cystatin C, a potent inhibitor of cysteine proteinases, is elevated in asthmatic patients. Clin Chim Acta. 2000;300(1):83–95. doi: 10.1016/S0009-8981(00)00298-9. [DOI] [PubMed] [Google Scholar]
- 19.Zhang D, Gao L, Ye H, Chi R, Wang L, Hu L, et al. Impact of thyroid function on cystatin C in detecting acute kidney injury: a prospective, observational study. BMC Nephrol. 2019;20(1):41. doi: 10.1186/s12882-019-1201-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deng Y, Wang L, Hou Y, Ma J, Chi R, Ye H, et al. The influence of glycemic status on the performance of cystatin C for acute kidney injury detection in the critically ill. Ren Fail. 2019;41(1):139–149. doi: 10.1080/0886022X.2019.1586722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stevens LA, Schmid CH, Greene T, Li L, Beck GJ, Joffe MM, et al. Factors other than glomerular filtration rate affect serum cystatin C levels. Kidney Int. 2009;75(6):652–660. doi: 10.1038/ki.2008.638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Royakkers AA, Korevaar JC, van Suijlen JD, Hofstra LS, Kuiper MA, Spronk PE, et al. Serum and urine cystatin C are poor biomarkers for acute kidney injury and renal replacement therapy. Intensive Care Med. 2011;37(3):493–501. doi: 10.1007/s00134-010-2087-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bjarnadottir M, Grubb A, Olafsson I. Promoter-mediated, dexamethasone-induced increase in cystatin C production by HeLa cells. Scand J Clin Lab Invest. 1995;55(7):617–623. doi: 10.3109/00365519509110261. [DOI] [PubMed] [Google Scholar]
- 24.Munoz J, Soblechero P, Duque FJ, Macias-Garcia B, Ruiz P, Zaragoza C, et al. Effects of Oral prednisone administration on serum Cystatin C in dogs. J Vet Intern Med. 2017;31(6):1765–1770. doi: 10.1111/jvim.14820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhu X-R, Ge N, Wang Y, Zhai J-L, Liu C. Corticosteroids significantly increase cystatin C levels in the plasma by promoting cystatin C production in rats. Ren Fail. 2019;41(1):698–703. doi: 10.1080/0886022X.2019.1638798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Risch L, Herklotz R, Blumberg A, Huber AR. Effects of glucocorticoid immunosuppression on serum Cystatin C concentrations in renal transplant patients. Clin Chem. 2001;47(11):2055–2059. doi: 10.1093/clinchem/47.11.2055. [DOI] [PubMed] [Google Scholar]
- 27.Poge U, Gerhardt T, Bokenkamp A, Stoffel-Wagner B, Klehr HU, Sauerbruch T, et al. Time course of low molecular weight proteins in the early kidney transplantation period--influence of corticosteroids. Nephrol Dial Transplant. 2004;19(11):2858–2863. doi: 10.1093/ndt/gfh341. [DOI] [PubMed] [Google Scholar]
- 28.Mendiluce A, Bustamante J, Martin D, Santos M, Bustamante R, Pascual P, et al. Cystatin C as a marker of renal function in kidney transplant patients. Transplant Proc. 2005;37(9):3844–3847. doi: 10.1016/j.transproceed.2005.09.203. [DOI] [PubMed] [Google Scholar]
- 29.Geramizadeh B, Azarpira N, Ayatollahi M, Rais-Jalali G-A, Aghdai M, Yaghoobi R, et al. Value of serum cystatin C as a marker of renal function in the early post kidney transplant period. Saudi J Kidney Dis Transplant. 2009;20(6):1015–1017. [PubMed] [Google Scholar]
- 30.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296. doi: 10.1371/journal.pmed.0040296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, et al. Toward complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. Acad Radiol. 2003;10(6):664–669. doi: 10.1016/S1076-6332(03)80086-7. [DOI] [PubMed] [Google Scholar]
- 32.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179–c184. doi: 10.1159/000339789. [DOI] [PubMed] [Google Scholar]
- 34.McCullough PA, Shaw AD, Haase M, Bouchard J, Waikar SS, Siew ED, et al. Diagnosis of acute kidney injury using functional and injury biomarkers: workgroup statements from the tenth acute Dialysis quality initiative consensus conference. Contrib Nephrol. 2013;182:13–29. doi: 10.1159/000349963. [DOI] [PubMed] [Google Scholar]
- 35.Endre ZH, Walker RJ, Pickering JW, Shaw GM, Frampton CM, Henderson SJ, et al. Early intervention with erythropoietin does not affect the outcome of acute kidney injury (the EARLYARF trial) Kidney Int. 2010;77(11):1020–1030. doi: 10.1038/ki.2010.25. [DOI] [PubMed] [Google Scholar]
- 36.Basu RK, Wang Y, Wong HR, Chawla LS, Wheeler DS, Goldstein SL. Incorporation of biomarkers with the renal angina index for prediction of severe AKI in critically ill children. Clin J Am Soc Nephrol. 2014;9(4):654–662. doi: 10.2215/CJN.09720913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meikle AW, Tyler FH. Potency and duration of action of glucocorticoids: effects of hydrocortisone, prednisone and dexamethasone on human pituitary-adrenal function. Am J Med. 1977;63(2):200–207. doi: 10.1016/0002-9343(77)90233-9. [DOI] [PubMed] [Google Scholar]
- 38.Ragab SM, Helwa MA, Khalaf AA. Serum cystatin C and microalbuminuria in children with immune thrombocytopenia under short course of corticosteroids. Egypt Pediatr Assoc Gaz. 2015;63(2):39–45. doi: 10.1016/j.epag.2015.05.001. [DOI] [Google Scholar]
- 39.Gruev T, Chakalarovski K, Stojceva-Taneva O, Grueva A, Trenceva K. Effects of glucocorticoid immunosuppression on serum cystatin C levels. J Med Biochem. 2009;28(3):191–196. doi: 10.2478/v10011-009-0014-y. [DOI] [Google Scholar]
- 40.Abbink FCH, Laarman CARC, Braam KI, van Wijk JAE, Kors WA, Bouman AA, et al. Beta-trace protein is not superior to cystatin C for the estimation of GFR in patients receiving corticosteroids. Clin Biochem. 2008;41(4):299–305. doi: 10.1016/j.clinbiochem.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 41.Borges RL, Hirota AH, Quinto BMR, Ribeiro AB, Zanella MT, Batista MC. Is Cystatin C a useful marker in the detection of diabetic kidney disease? Nephron Clin Pract. 2010;114(2):c127–c134. doi: 10.1159/000254385. [DOI] [PubMed] [Google Scholar]
- 42.Fricker M, Wiesli P, Brändle M, Schwegler B, Schmid C. Impact of thyroid dysfunction on serum cystatin C. Kidney Int. 2003;63(5):1944–1947. doi: 10.1046/j.1523-1755.2003.00925.x. [DOI] [PubMed] [Google Scholar]
- 43.Song T, Jia Z, Guo X, Zhao H, Bao W, Han D, et al. Does hepatic impairment influence renal function parameters in liver cirrhosis? J Transl Int Med. 2018;6(2):90–92. doi: 10.2478/jtim-2018-0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ghane Shahrbaf F, Assadi F. Drug-induced renal disorders. J Renal Inj Prev. 2015;4(3):57–60. doi: 10.12861/jrip.2015.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Le Bricon T, Thervet E, Froissart M, Benlakehal M, Bousquet B, Legendre C, et al. Plasma Cystatin C is superior to 24-h Creatinine clearance and plasma Creatinine for estimation of glomerular filtration rate 3 months after kidney transplantation. Clin Chem. 2000;46:1206–1207. doi: 10.1093/clinchem/46.8.1206. [DOI] [PubMed] [Google Scholar]
- 46.Silva MV, Moscoso Solorzano G, Nishida SK, Kirsztajn GM. Are serum cystatin C levels infl uenced by steroid doses in lupus nephritis patients? J Bras Nefrol. 2011;33.. [DOI] [PubMed]
- 47.El-Esawy NM, Morad MA, Abdin AA. Urinary Creatinine and serum Cystatin C in asthmatic children treated with inhaled corticosteroid and Beta 2 agonist. Alex J Pediatr. 2005;19(2):231. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1:Fig. S1 Performance of sCysC for AKI detection before and after matching. A Performance of sCysC for total AKI detection before and after matching; B Performance of sCysC for established AKI detection before and after matching; C Performance of sCysC for later-onset AKI detection before and after matching; Established AKI, defined as diagnosis of AKI at ICU admission; Later-onset AKI, indicated no AKI diagnosis at ICU admission but reaching the KDIGO criteria within 1 week after admission; AKI: Acute kidney injury; ICU: Intensive care unit; KDIGO: Kidney Disease: Improving Global Outcomes;
Data Availability Statement
The datasets generated and/or analyzed during this study are not publicly available, owing to currently ongoing research studies, but the data are available from the corresponding author on reasonable request.