Abstract
Osteochondral fractures of the knee represent a challenging entity to manage since there are many different surgical techniques for cartilage repair or other salvage procedures. In terms of cartilage repair, several hardware devices can be used, and many of them could imply a second-stage surgery for hardware removal. The purpose of this article is to describe in detail a one-stage osteochondral fracture repair technique with knotless anchors and interconnected crossing suture sliding loops for the knee. This technique is a one-stage open or arthroscopic procedure with an unlimited number of loops configurations with no particular need for a second surgery for hardware removal, no knot damage, and without the use of bone tunnels. It can be used in different cartilage anatomic locations, such as femoral condyles, trochlea, patella, or other joints.
Osteochondral fracture (OCF) is an injury of the lateral femoral condyle/trochlea or patella that usually occurs in adolescents or young adults after trauma or patellar dislocation.1, 2, 3, 4 This entity is not always easy to differentiate from osteochondritis dissecans, a disorder of one or more ossification centers, usually in the lateral aspect of the medial femoral condyle.5 The patient with an acute OCF has a trauma/dislocation history either by a direct blow to the patella or by a twisting mechanism. Clinical presentation is usually pain, swelling, and functional limitation. Imaging usually includes radiography (X-ray), computer tomography scan, and/or magnetic resonance imaging to identify the osteochondral defect and the fragment or loose body.2,3
To avoid the early degenerative phenomena, high-grade of suspicion and early diagnosis are required, so that the surgical treatment can take place as soon as possible.
Classically, the treatment of OCFs include osteosynthesis of the fragment with different devices described in the literature, such as standard compression screws, headless compression screws, Herbert screws, bioabsorbable screws and pins, meniscus arrows, or sutures passed through complete bone tunnels.6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18
Occasionally, when the subchondral bone or the fragment is too small for fixation or chronic, it has to be removed and managed with cartilage restorative techniques, such as debridement and/or micro/nanofractures, autologous chondrocyte implantation/matrix-induced chondrocyte implantation, mosaicplasty, bone grafts and scaffolds, biomaterials or fresh osteochondral allograft, depending on the size and depth of injury.19, 20, 21, 22, 23
The purpose of this Technical Note is to describe the one-stage osteochondral fracture repair technique with knotless anchors and interconnected crossing suture sliding loops, with no complete bone tunnels, no need for a second-stage surgery hardware removal, and suitable in certain cases (Table 1) and for different anatomic locations, such as patella, condyle, or trochlea defects.
Table 1.
Indications and Contraindications for One-Stage Osteochondral Fracture Repair Technique With Knotless Anchors and Interconnected Crossing Suture Sliding Loops for the Knee
Indications
|
Contraindications
|
Surgical Technique
The patient is positioned supine with a tourniquet applied. After skin preparation and draping, diagnostic arthroscopy is usually performed to assess the cartilage injury. The skin is then marked with a marking pen for the following anatomical landmarks and skin incision. A longitudinal lateral or medial parapatellar incision is made as needed for injury exposure (Video 1). Subcutaneous tissue is dissected, and a lateral or medial parapatellar arthrotomy is then performed.
The chondral or osteochondral fragment is then located, removed, prepared, and cleaned at the back table (Fig 1). Close attention should be taken to regularize the edges of the fragment, avoiding excessive bone or cartilage debridement. The defect is also cleaned and deepened with a curette, creating a bleeding bed, and irregular and unstable cartilage edges are removed. The fragment and the defect are then evaluated and sized to avoid size mismatches. Later on, the fragment is placed in the correct position. Other pearls and pitfalls should be taken into account in the surgical osteochondral fracture repair with knotless anchors and interconnected crossing suture sliding loops for obtaining an optimal result (Table 2).
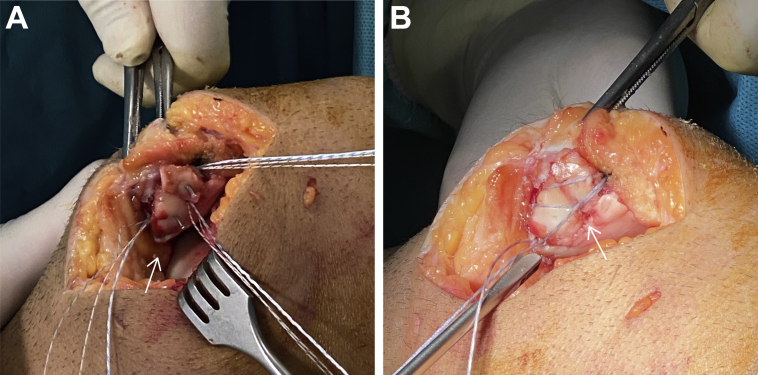
Fig 1.
Osteochondral defect on the lateral trochlea of a right knee in a patient with decubitus supine position (A) and a chondral fragment (B). The defect (A) and the fragment (B) should be sized for proper fit between them.
Table 2.
Pearls and Pitfalls of the One-Stage Osteochondral Fracture Repair Technique with Knotless Anchors and Interconnected Crossing Suture Sliding Loops for the Knee
Pearls
|
Pitfalls
|
Next, the drill guide for the first anchor should be positioned correctly in the desired position, such that the drilling takes place in the edges of the defect, in the vicinity of healthy cartilage. The knotless sliding anchors (Knotless BioComposite SutureTak 3 mm; Arthrex, Naples, FL) should then be placed after each drilling. Once all the anchors are in place, the main suture of each anchor should be interconnected with a different opposite anchor. These knotless anchors are provided with a primary high-strength suture and a shuttling thread, so that a loop is created in between the primary suture from one suture and the shuttling thread from a distant anchor. Multiple crossing loops configurations are possible with this technique (Fig 2). For tightening, the free ends of different compression sutures already shuttled into the anchors should be pulled, so that the sliding mechanism and the loop generate compression over the fragment. The ends of the sutures are cut with a blade at the edges of the fragment.
Fig 2.
Crossing sutures loops configuration. (A) Three knotless anchors are equally distanced between each other; each repair suture is interconnected to a distant anchor using the shuttling mechanism, so that the loops stay and generate compression forces over the fragment. (B) Three loops connect to each other in the knotless sliding anchors without the need for bone tunneling.
At the end of the procedure (Fig 3), the knee should be cycled to check the stability of the fragment and the quality of the repair. The retinaculum is sutured to close the arthrotomy, the following layers are then closed, and proper dressing is applied.
Fig 3.
Final crossing sutures knotless loop configuration for osteochondral fracture repair on the lateral trochlea. White arrow marks the lesion.
Postoperative Rehabilitation
Postoperatively, the patient is placed in a straight knee brace in extension for 1 month with non–weight-bearing for 3 to 4 weeks, and then progressive partial weight-bearing is allowed with crutches. Isometric exercises should begin in the first week. After 1 week, the brace should be taken once per day for 0 to 90° passive flexion exercises.
Discussion
There are different techniques described in the literature for the repair of osteochondral fractures and to avoid future chondral damage and subsequent osteoarthrosis.6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 The more classic techniques use metallic devices, such as screws and pins, and more recently, there is new available materials and biomaterials with new mechanisms of fixation. Some of these materials are resorbable, which are thought to be less harmful to the cartilage and the surrounding soft tissues. They can protrude, move, and fail to fix the fragment due to the degree and capacity of fixation and compression, remaining in situ while healing and before the possible enzymatic reabsorption or hardware biochemical reactions. Hardware protrusion, movement, migration, and failure can lead to collateral damage to healthy soft tissues, such as cartilage, bone, or meniscus (Table 3).24 Hardware biochemical reactions can lead to foreign body reactions, osteolysis, inflammation, infection, nonunion, malunion, pseudotumor, and clinical symptoms such as stiffness, pain, and functional limitations. These complications can justify a second surgery for hardware removal, which has an impact on the patient's recovery, satisfaction, and economic implications. Moreover, implant hardware removal does not guarantee avoidance of hardware complications, relief, or improvement and may be associated with further complications.25 The real impact and prevalence of these complications, as well as the rate of a second hardware removal surgery, are not found explicitly in the literature for cartilage surgery repair. There are no general guidelines for hardware removal, although some surgeons prefer to remove some of these devices and avoid future complications.
Table 3.
Advantages and Disadvantages of One-Stage Osteochondral Fracture Repair Technique With Knotless Anchors and Interconnected Crossing Suture Sliding Loops for the Knee
Advantages
|
Disadvantages
|
OCD, osteochondritis dissecans.
There are different indications and contraindications for one-stage osteochondral fracture repair technique with knotless anchors and interconnected crossing suture sliding loops for the knee that should be respected to maximize surgical outcomes (Table 1).
One of the advantages of this technique is that this implant uses high-strength braided non-absorbable sutures (No. 2 FiberWire; Arthrex), which has shown resistance to bending abrasion compared with other sutures.26 Unlike other types of devices, this type of suture is not known to cause complications that would require a second surgery for its removal.
The peculiarity of knotless anchors minimizes the risk of iatrogenic surrounding cartilage or tissue damage.27 Suture fixation can give a uniform compression of the fragment(s) without penetrating to the cartilage tissue, and an unlimited number of loops configurations can be used. This characteristic potentially allows for earlier rehabilitation and return-to-play, as we have seen clinically in the presented cases.
This technique can be performed with open or mini-open surgery or by arthroscopy, depending on the injury and surgeon's preference and skills. In cases of comminuted or irregular non-contained fragments, provisional fixation with K-wires could be used to allow the osteochondral fracture fixation with crossing sutures knotless (Fig 4).
Fig 4.
(A) Provisional K-wire fixation in a comminuted medial facet patellar osteochondral fracture. White arrow marks the lesion. (B) Final crossing sutures knotless fixation.
Comparing our technique with other suture techniques for cartilage repair, such as the one described by Ng et al.8 for patella or by Bowers and Huffman11 for femoral condyle defects, our technique does not use bone tunnels, which simplifies the technique and reduces the risk of fractures. Another advantage is that it can be used in different anatomic locations, such as patella, femoral condyles, trochlea, or in other joints, unlike mentioned techniques described in the literature.
However, some potential disadvantages and risks of this technique could be less potential fixation strength (no complete fragment passage of the sutures); potential loosening of the sliding loop mechanism and failure; and potentially inflammatory responses, synovitis,24 and cartilage abrasion (load-bearing surfaces) (Table 2).
Acknowledgments
We thank Maria Sava, College of Osteopathic Medicine of the Pacific Western University of Health Sciences, for the English correction of this manuscript.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.C. and García Cugat Foundation receive research support from Smith and Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Description of the one-stage osteochondral fracture repair technique with knotless anchors and interconnected crossing suture sliding loops for the knee.
References
- 1.Chotel F., Knorr G., Simian E., Dubrana F., Versier G. Knee osteochondral fractures in skeletally immature patients: French multicenter study. Orthop Traumatol. 2011;97:154–159. doi: 10.1016/j.otsr.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 2.Lee B.J., Christino M.A., Daniels A.H., Hulstyn M.J., Eberson C.P. Adolescent patellar osteochondral fracture following patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2013;21:1856–1861. doi: 10.1007/s00167-012-2179-z. [DOI] [PubMed] [Google Scholar]
- 3.Seeley M.A., Knesek M., Vanderhave K.L. Osteochondral injury after acute patellar dislocation in children and adolescents. J Pediatr Orthop. 2013;33:511–518. doi: 10.1097/BPO.0b013e318288b7a0. [DOI] [PubMed] [Google Scholar]
- 4.Liu J.N., Steinhaus M.E., Kalbian I.L. Patellar instability management: a survey of the international patellofemoral study group. Am J Sports Med. 2018;46:3299–3306. doi: 10.1177/0363546517732045. [DOI] [PubMed] [Google Scholar]
- 5.Kan J.H. Osteochondral abnormalities: Pitfalls, injuries, and osteochondritis dissecans. ARRS Categorical Course. 2011:149–152. [Google Scholar]
- 6.Dhawan A., Hospodar P.P. Suture fixation as a treatment for acute traumatic osteochondral lesions. Arthroscopy. 1999;15:307–311. doi: 10.1016/s0749-8063(99)70040-x. [DOI] [PubMed] [Google Scholar]
- 7.Gkiokas A., Morassi L.G., Kohl S., Zampakides C., Megremis P., Evangelopoulos D.S. Bioabsorbable pins for treatment of osteochondral fractures of the knee after acute patella dislocation in children and young adolescents. Adv Orthop. 2012;2012:1–4. doi: 10.1155/2012/249687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ng W.M., Al-Fayyadh M.Z.M., Kho J., Seow Hui T., Mohamed Ali M.R.B. Crossing suture technique for the osteochondral fractures repair of patella. Arthrosc Tech. 2017;6:e1035–e1039. doi: 10.1016/j.eats.2017.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hammerle C.-P., Jacob R.P. Chondral and osteochondral fractures after luxation of the patella and their treatment. Arch Orthop Trauma Surg. 1980;97:207–211. doi: 10.1007/BF00389728. [DOI] [PubMed] [Google Scholar]
- 10.Tonin M., Said A.M., Veselko M. Arthroscopic reduction and fixation of osteochondral fracture of the patellar ridge. Arthroscopy. 2001;17:1–4. doi: 10.1053/jars.2001.21255. [DOI] [PubMed] [Google Scholar]
- 11.Bowers A.L., Huffman G.R. Suture bridge fixation of a femoral condyle traumatic osteochondral defect. Clin Orthop Rel Res. 2008;466:2276–2281. doi: 10.1007/s11999-008-0357-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wouters D.B., Burgerhof J.G.M., de Hosson J.T.M., Bos R.R.M. Fixation of osteochondral fragments in the human knee using Meniscus Arrows®. Knee Surg Sports Traumatol Arthrosc. 2011;19:183–188. doi: 10.1007/s00167-010-1158-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aydoğmuş S., Duymuş T.M., Keçeci T. An unexpected complication after headless compression screw fixation of an osteochondral fracture of patella. Case Rep Orthop. 2016;2016:1–4. doi: 10.1155/2016/7290104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cavalheiro C.M., Gobbi R.G., Hinckel B.B., Demange M.K., Pécora J.R., Camanho G.L. Femoral condyle osteochondral fracture treated with bone suture after acute patellar dislocation: A case report. Rev Bras Ortop. 2018;53:636–642. doi: 10.1016/j.rboe.2017.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schlechter J.A., Nguyen S.V., Fletcher K.L. Utility of bioabsorbable fixation of osteochondral lesions in the adolescent knee: Outcomes analysis with minimum 2-year follow-up. Orthop J Sports Med. 2019;7:12–14. doi: 10.1177/2325967119876896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Z.-X., Song H.-H., Wang Q., Guo D.-M. Clinical outcomes after absorbable suture fixation of patellar osteochondral fracture following patellar dislocation. Ann Transl Med. 2019;7 doi: 10.21037/atm.2019.03.52. 173-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Megremis P., Megremis O., Margariti R. Late repair, one year after a knee twisting injury, of a missed femoral trochlea osteochondral fragment, with bioabsorbable nails, in a 14-year-old boy. J Am Acad Orthop Surg Glob Res Rev. 2019;3 doi: 10.5435/JAAOSGlobal-D-18-00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsu T.-L., Lin S.-M., Chang C.-H., Lan T.-Y. Neglected pediatric osteochondral fracture dislocation of the patella. Case Rep Orthop. 2019;2019:1–5. doi: 10.1155/2019/2904782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cole B.J., Pascual-Garrido C., Grumet R.C. Surgical management of articular cartilage defects in the knee. J Bone Joint Surg Am. 2009;91:1778–1790. [PubMed] [Google Scholar]
- 20.Hinzpeter J., Zamorano A., Barahona M., Campos P. Treatment of osteochondritis dissecans of the knee with autologous iliac bone graft and hyaluronic acid scaffold. Knee Surg Rel Res. 2019;31:143–146. doi: 10.5792/ksrr.18.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kon E., Robinson D., Shani J. Reconstruction of large osteochondral defects using a hemicondylar aragonite-based implant in a caprine model. Arthroscopy. 2020;36:1884–1894. doi: 10.1016/j.arthro.2020.02.026. [DOI] [PubMed] [Google Scholar]
- 22.Gelber P.E., Perelli S., Ibañez M. Fresh osteochondral patellar allograft resurfacing. Arthrosc Tech. 2018;7:e617–e622. doi: 10.1016/j.eats.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Woodmass J.M., Melugin H.P., Wu I.T., Saris D.B.F., Stuart M.J., Krych A.J. Viable osteochondral allograft for the treatment of a full-thickness cartilage defect of the patella. Arthrosc Tech. 2017;6:e1661–e1665. doi: 10.1016/j.eats.2017.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Acklin Y.P., Bircher A., Morgenstern M., Richards R.G., Sommer C. Benefits of hardware removal after plating. Injury. 2018;49:S91–S95. doi: 10.1016/S0020-1383(18)30311-5. [DOI] [PubMed] [Google Scholar]
- 25.Savage E., Hurren C.J., Slader S., Khan L.A.K., Sutti A., Page R.S. Bending and abrasion fatigue of common suture materials used in arthroscopic and open orthopedic surgery. J Orthop Res. 2013;31:132–138. doi: 10.1002/jor.22185. [DOI] [PubMed] [Google Scholar]
- 26.Visscher L.E., Jeffery C., Gilmour T., Anderson L., Couzens G. The history of suture anchors in orthopaedic surgery. Clin Biomech. 2019;61:70–78. doi: 10.1016/j.clinbiomech.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 27.Lovric V., Goldberg M.J., Heuberer P.R. Suture wear particles cause a significant inflammatory response in a murine synovial airpouch model. J Orthop Surg Res. 2018;13:1–8. doi: 10.1186/s13018-018-1026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of the one-stage osteochondral fracture repair technique with knotless anchors and interconnected crossing suture sliding loops for the knee.