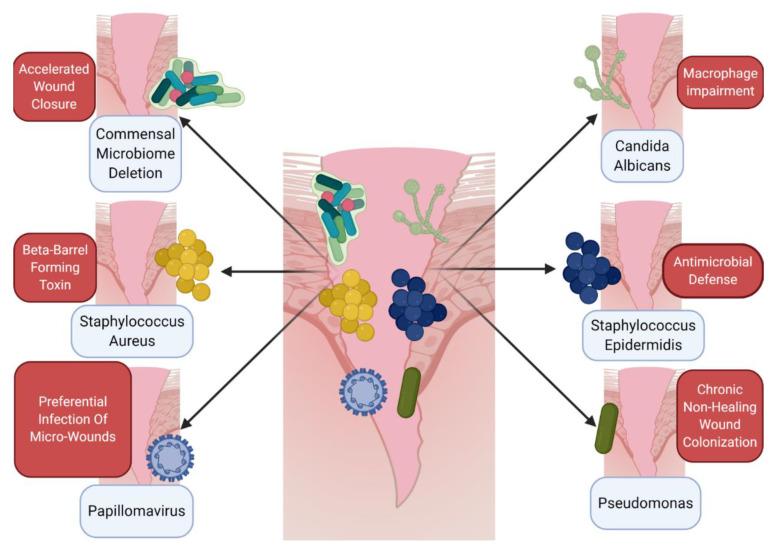
Figure 1.
Host–microbe cross talk informs the immune microenvironment of wounds. A number of different microbes, including various bacteria, viruses, and fungi, can directly impact wound healing and alter the immune microenvironment. Upon wounding, whether by trauma, arthropod bite, or chronic barrier disruption, skin-resident bacteria, viruses, and fungi all can impact the microenvironment of the healing tissue. Several general and specific examples of this microenvironment interaction have been elucidated recently. Paradoxically, germ-free mice exhibit accelerated wound closure when compared to conventionally raised mice [54]. Other specific microbes have distinct effects on immune cells, including Staphylococcus aureus, which creates beta-barrel forming toxins to impair macrophage function in the wound [58], or Candida albicans, which also disrupts normal macrophage action [59]. While not a direct immune cell effect, other pathogens can impact the microenvironment, hijacking or colonizing wounds directly, including papillomavirus [60] and Pseudomonas species [61]. Skin commensal microbes such as Staphylococcus epidermidis can promote immune defenses in the wound [57] via phenol-soluble modulins. This provides a snapshot of the various roles of microbes in the wound microenvironment but is not exhaustive. Further study is needed to fully understand the skin microbiome–wound microenvironment interaction. Figure created using BioRender.