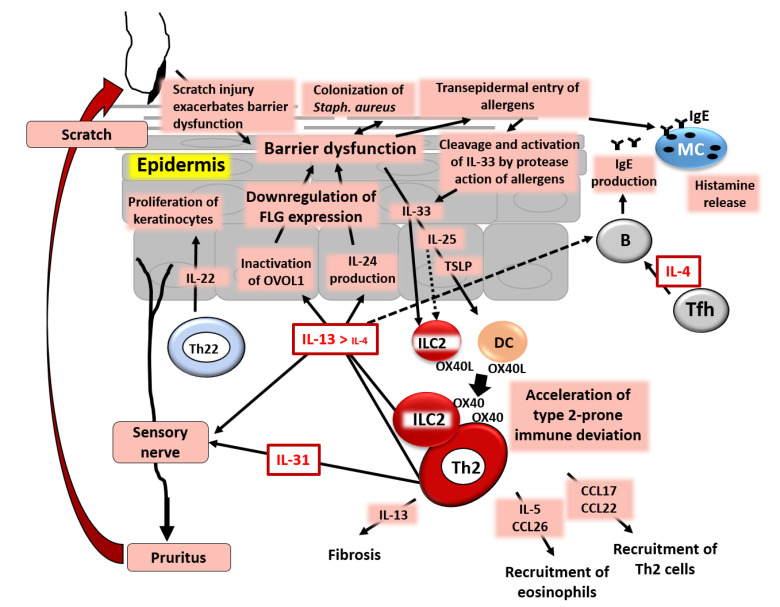
Figure 5.
Simplified pathogenesis of AD. IL-4 and especially IL-13, produced from group 2 innate lymphoid cells (ILC2s) and T helper 2 (Th2) cells, down-regulate FLG expression and induce barrier dysfunction via inactivation of OVOL1. IL-13/IL-4 stimulate keratinocytes to produce periostin and then IL-24, which also down-regulates FLG expression. Keratinocytes in the barrier-disrupted epidermis release thymic stromal lymphopoietin (TSLP), IL-25, and IL-33, which up-regulate the expression of OX40L in ILC2s and dendritic cells (DCs). OX40L-positive ILC2s and DCs accelerate the differentiation of OX40-positive ILC2s and Th2 cells. The barrier dysfunction triggers the colonization of Staphylococcus aureus and transepidermal entry of allergens. Many allergens have protease activity, which cleaves full-length IL-33 to active short-form IL-33. T follicular helper (Tfh) cells produce IL-4, which stimulates B cells to produce IgE. IgE on mast cells (MCs) is ligated by allergens and the MCs then release histamine and other chemical mediators. IL-31 and IL-13/IL-4 stimulate sensory nerves and induce pruritus with subsequent scratch behavior, which further exacerbates skin barrier dysfunction. An IL-13/IL-4-rich milieu up-regulates the production of CCL17 and CCL22, which induce the preferential recruitment of Th2 cells. An IL-13/IL-4-dominant microenvironment also up-regulates the production of IL-5 and CCL26, which attract eosinophils. IL-13 is responsible for the pro-fibrotic process and is also involved in lichenification and tissue remodeling.