Figure 2.
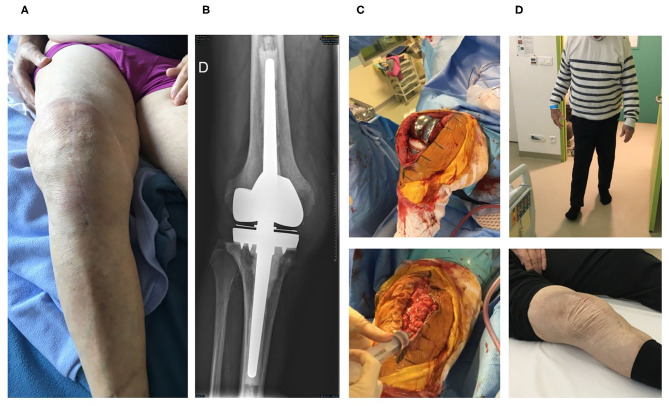
The second patient is an 84-year-old man with past history of dyslipidemia and right prosthetic-knee arthroplasty in 2006. A two-stage exchange was performed in 2007 for a S. epidermidis PKI. As the patient kept a painful knee, a one-stage exchange was performed in 2016, with implantation of a hinged cemented knee prosthesis with long stem. Cultures remained sterile. In 2019, the patient developed clinical signs of acute septic arthritis with fever. A DAIR without polyethylene exchange was performed and methicillin-susceptible S. aureus grew in perioperative samples and blood cultures. Endocarditis was excluded. The patient was treated using intravenous cefazolin and rifampin orally. Cefazolin was switched to ofloxacin 3 weeks after the DAIR and was combined with rifampin. Under this treatment, new signs of septic arthritis occurred 6 weeks after the DAIR, with local erythema, pain, and large joint effusion (A). A joint puncture was performed, but no pathogen was isolated in cultures, and the failure was attributed to S. aureus. X-ray showed no loosening of the prosthesis (B). Open DAIR was performed showing significant local inflammation and pus into the joint. The personalized cocktail of phages was administered after joint closure (C). The patient improved quickly, doxycycline was then prescribed as suppressive therapy, and the outcome was favorable at 7 months with no signs of infection, a negative C-reactive protein and pain-free walking [(D), Supplementary Video 2].