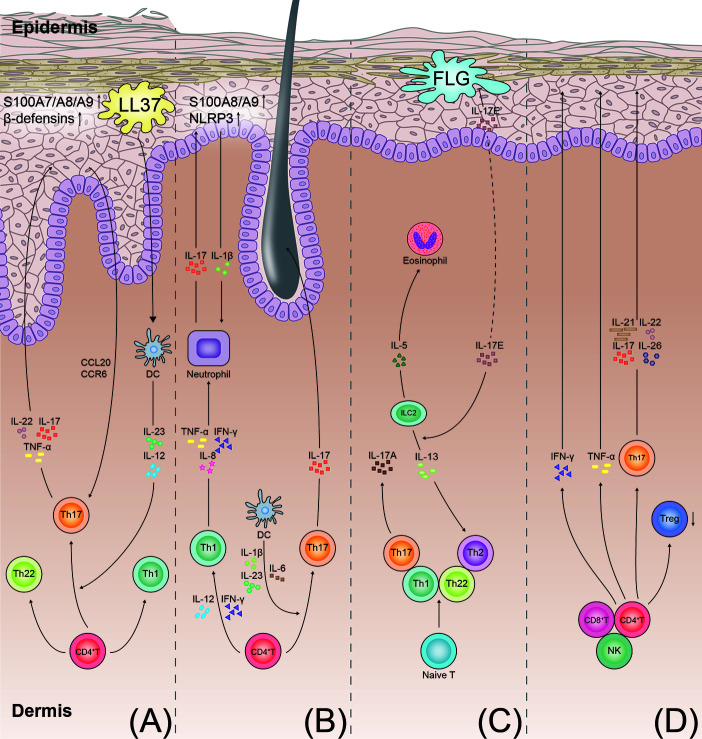
Figure 2.
T-cell immune axis and associated cytokines in the pathogenesis of psoriasis, hidradenitis suppurativa, atopic dermatitis, and alopecia areata. (A) Psoriasis develops through the aberrant activation of the dendritic cells producing IL-12 and IL-23. The dendritic cells induce the differentiation of the Th 17 cells and Th1 cells. IL-23 promotes the Th17 cells to secrete IL-17, IL-22, and TNF-α. In keratinocytes, IL-17 also stimulates production of antimicrobial peptides (S100A7/A8/A9 proteins and beta defensins). These cytokines promote keratinocyte proliferation and neutrophil recruitment, resulting in the formation of psoriatic plaques. (B) In hidradenitis suppurativa, the T cells involved in the pathogenesis of hidradenitis suppurativa include the Th1 and Th17 cells. IL-23 induces the differentiation of the Th17 cells and overexpression of IL-17. IL-17 induces the expression of the proinflammatory proteins (S100A8/A9) and NLRP3 in the keratinocytes. More inflammatory cytokines are recruited to the follicular unit and perilesional skin. (C) In atopic dermatitis, with impairment of the skin barrier in patients with atopic dermatitis, the damaged keratinocytes produce inflammatory cytokines (IL-17E). The cytokines stimulate the ILC2s to secrete type 2 cytokines (IL-5 and IL-13). IL-17E also inhibits the synthesis of FLG. IL-4, IL-13, and IL-31 directly stimulate the sensory nerves to promote pruritus. (D) In alopecia areata, the elevated IFN-γ levels in the perifollicular area activate the differentiation of the CD4+ T cells into various types of T cells, as shown. Th17 cells act on the hair follicle by producing proinflammatory mediators (IL-17, IL-21, IL-22, and IL-26), ultimately leading to the disruption of hair growth. TNF, tumor necrosis factor; NLRP3, NACHT, LRR, and NACHT, LRR, and PYD domains-containing protein 3; FLG, filaggrin; ILC2s, type 2 innate lymphoid cells; DC, dendritic cell.