Figure 3.
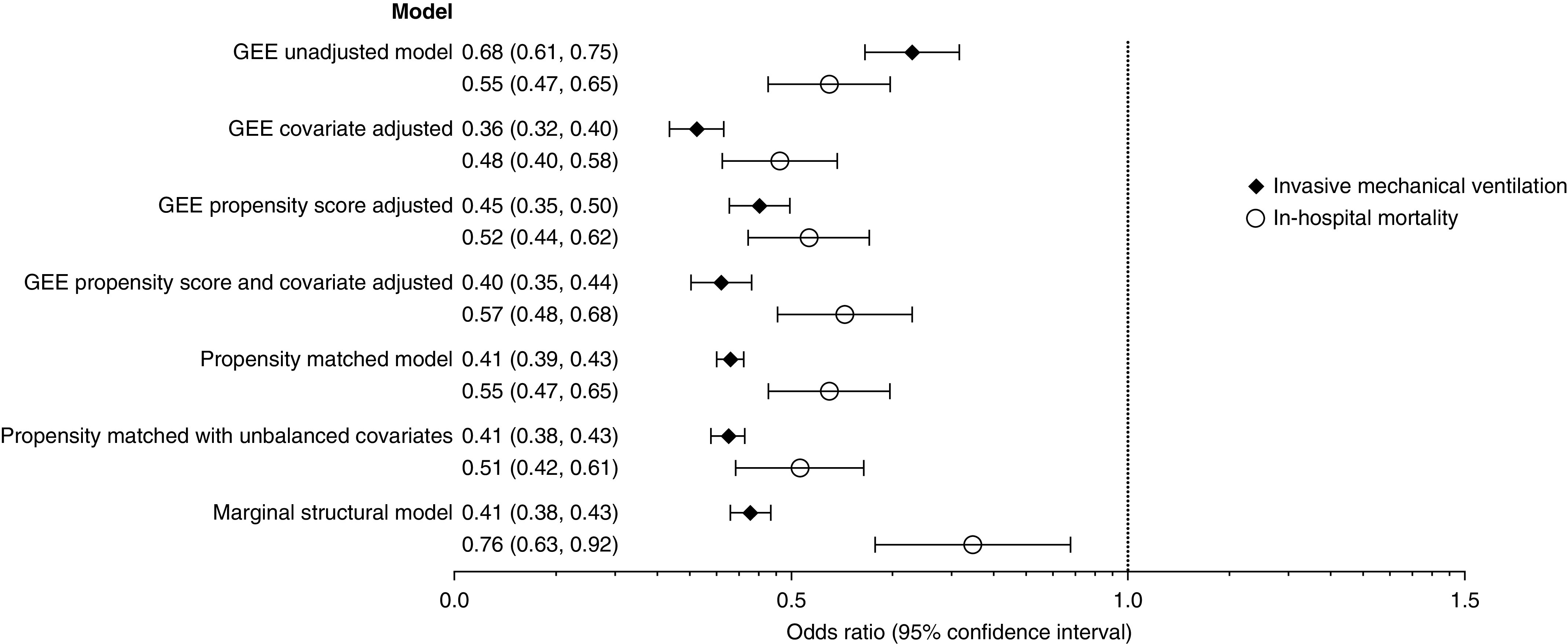
Associations between noninvasive ventilation and subsequent invasive mechanical ventilation and mortality among patients admitted with asthma exacerbation to the ICU. Generalized estimating equation (GEE) and marginal structural models N = 53,654. Propensity-matched models n = 25,450. GEE covariate adjusted included age, sex, race, marital status, primary insurance, admission year and quarter, primary admitting diagnosis of asthma, primary admitting diagnosis of respiratory failure, Elixhauser comorbidity score, hypertension, diabetes, hypothyroidism, obesity, right heart failure, valvular disease, psychoses, alcohol abuse, sleep apnea, weight loss, solid tumor, drug abuse, pulmonary circulation disease, tobacco use, pneumonia, severe sepsis, quartile of hospital beds, population served, teaching hospital, geographic region, attending specialty, and the following early treatments and tests: magnesium, inhaled corticosteroid, inhaled long-acting β-agonist, antibiotics, spirometry, and arterial blood gas. The propensity-matched model with unbalanced covariates included right heart failure, valvular disease, pulmonary circulation disease, solid tumor, psychosis, end-stage renal disease, cirrhosis, and arterial blood gas. Marginal structural model: time-varying confounder included in stabilized inverse probability of treatment weights included administration of magnesium, antibiotics, inhaled corticosteroid, spirometry or peak flow measurement, arterial blood gas, and exposure to noninvasive ventilation in the days prior in addition to baseline covariates included in the GEE covariate-adjusted model.
