The COVID-19 pandemic has broadly impacted biomedical research and clinical practice. The effect on early career researchers has been particularly significant, likely resulting in long-lasting consequences. During the lockdown, we conducted a series of initiatives to listen and understand the effect the pandemic had on laboratory and clinical research. Here we present the main conclusions of our surveys. We aim to stimulate discussion and to empower early career researchers to take actions that might help in boosting their research, career and well-being during and after the pandemic.
The COVID-19 pandemic has dramatically changed our everyday routine. Starting early 2020, several countries worldwide locked research centers down and temporarily halted clinical trials for several weeks. This not only resulted in significant disruption of biomedical activities and clinical research but also of routine medical care delivery, with dramatic consequences on health economics. As many young researchers worldwide, we suddenly found ourselves isolated at home, having to manage work-life balance through a very fragile equilibrium and with high doses of uncertainty for the near future. Furthermore, many schools were closed and that had a major impact on those having to take care of young children.1
Going through the difficult situation of the lockdown, we decided to launch an initiative to listen to the needs and worries of other researchers, particularly to assess the impact on early career scientists like us. We aimed to start a conversation among clinical and basic researchers, to get a picture of the consequences of the pandemic on their personal and professional life, and to explore ways to alleviate the negative impact of COVID-19 safety measures both short and long term. Given the intrinsic differences between clinical and basic research, we created 2 independent online surveys specifically designed for these 2 categories. Since the European Hematology Association (EHA) is a comprehensive association including both clinical and basic researchers, we were able to gather this information and compare the differential impact and needs in both profiles. An invitation was sent to EHA members, and it was also shared through social media. The information collected on each survey fed the discussion in two consecutive webinars organized by the EHA and the YoungEHA committee that are available online for free (Table 1).
Table 1.
Call to Action. Useful Suggestions to Action that have Arisen Through our Surveys.
| Topic | More information |
|---|---|
| Peer-mentoring groups at individual institutions | https://ehaweb.org/youngeha/blog/mentoring-peer-peer-networks-a-recipe-for-success |
| Resetting research/clinical laboratories | EHA basic and clinical research webinars: https://www.youtube.com/watch?v=AV-1Lyfm6Zo&feature=youtu.be; https://www.youtube.com/watch?v=vUB6BBSUg4M&feature=youtu.be |
| Early career researchers / gender equity | https://www.universityaffairs.ca/opinion/the-black-hole/; www.pnas.org/cgi/doi/10.1073/pnas.2010636117; |
| Sharing research ideas | https://european-hematology-association.tribe.so/login?redirect=/ |
| Reducing bureaucracy | https://journals.lww.com/hemasphere/Fulltext/2020/04000/Reducing_Bureaucracy_in_Clinical_Research__A_Call.5.aspx |
| Guidance for research | https://ec.europa.eu/health/sites/health/files/human-use/docs/guidance_regulatory_covid19_en.pdf |
Our 2 surveys collected data from 276 researchers, 70% of whom were based in Europe (mostly Spain, United Kingdom, Italy, Germany and Greece), and 30% were participants from overseas (mostly the US, India, Mexico and Egypt) (Fig. 1A). We had a good representation of both academic and clinical researchers, with overall almost 60% being clinicians/physician scientists (hereinafter referred as clinical researchers, CRs) and 40% basic/translational researchers (hereinafter referred as basic researchers, BRs). Among BRs, most participants of the survey had management responsibilities, corresponding largely to postdoctoral researchers who already supervise personnel and principal investigators who manage a full laboratory. Of them, only 22% were able to continue doing wet lab research. On the other hand, approximately half of the CRs that participated in our clinical survey were medical specialists (MD or equivalent), while 39% identified themselves as physician scientists. Most of the CRs that participated were involved in the recruitment, design or running of clinical trials, and the majority were in charge of managing personnel and projects. According to our survey, 66% of CRs were still able to do research. Additionally, as much as 40% said that they were assigned to take care of hematology patients with COVID-19 or COVID-19 patients in general.
Figure 1.
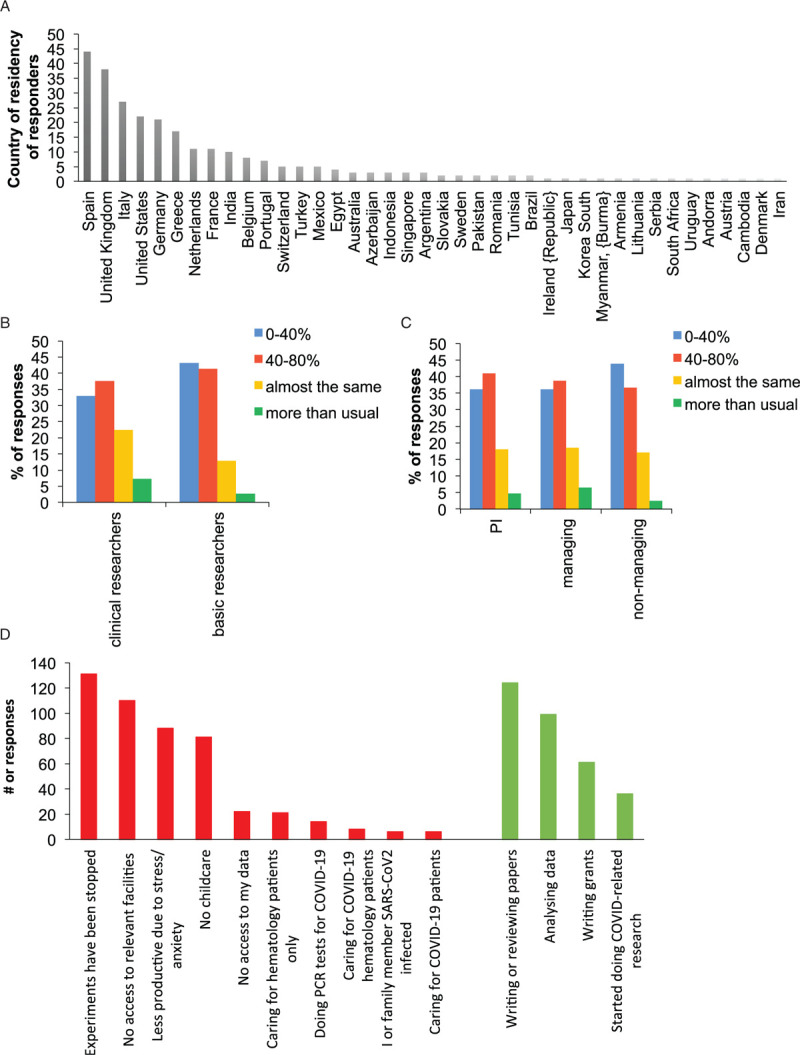
Summary of main results derived from the two surveys launched by YoungEHA committee. (A) Country of residence of the participants. (B) Comparison of percentage of responses between clinical researchers and basic researchers on the effect the lockdown had on their productivity. (C) Comparison of responses between researchers at different career stages on the effect the lockdown had on their productivity. PI = principal investigator, person responsible of managing a lab; Managing = person responsible of managing people, postdoc researcher or equivalent; Non-managing = person without managing responsibilities, PhD student or equivalent. (D) Bar graph summarizes the number of participants that have selected a given statement as one of the main causes of their change in productivity during the lockdown. In red (left) are statements that may cause a hinder in productivity and in green (right) those that may enhance it.
Our first priority with these 2 surveys was to determine the impact of the lockdown on productivity and work-life balance. As expected, the lockdown had a major impact on the productivity of both groups with 33% of CRs and 43% of BRs stating that they were below 40% of their normal productivity. Interestingly, 22% of CRs and 13% of BRs claimed to be as productive as before the lockdown. Furthermore, 7% of the CRs reported to be “more productive than usual” while only 3% of BRs chose that answer (Fig. 1B). Although both types of researchers were affected, productivity of BRs suffered more from the isolating conditions secondary to the pandemic. Unfortunately, due to the heterogeneity of our sample, it was not possible to assess differences between countries. When comparing the answers related to career stage, regardless of being CRs or BRs, we found that the youngest participants (i.e. those that do not have any management responsibilities, such as PhD students) were more impacted, with 44% of them having very poor productivity. However, we did not find remarkable differences in the answers from principal investigators and postdoctoral researchers, with 40% having very poor productivity, 40% medium-low productivity, 20% “equal than usual” and around 10% declaring to be “more productive than usual” (Fig. 1C).
In order to understand changes in productivity, we invited the participants to select three statements from a given list of possible causes (Fig. 1D). As expected, strict lockdown conditions caused major disruption that forced the majority of scientist to stop experiments. This was also due to the lack of access to many critical facilities. Being a natural consequence of the pandemic, stress and anxiety were also recognized as relevant causes for reduced productivity and disruption of childcare services resulted in more time dedicated to childcare. Other causes for changes in productivity reported in the survey were lack of access to own research data, clinical care of COVID-19 patients and lab duties for SARS-CoV2 PCR tests. On the positive side, those not primarily involved in COVID-19 research/care, took advantage of the lockdown to write or review papers, analyze data and write grants. Also, a minor but significant fraction of participants started to do COVID-19 related research during this pandemic (Figure 1D).
We were also concerned about consequences of the pandemic on research funding, which could have particularly impacted early career researchers that are transitioning to independence. This was difficult to assess in an international survey as each country, even within Europe, has very different funding strategies. However, from our survey it was clear that charity-based funding agencies, for example in the United Kingdom, experienced major funding restrictions leading to multiple requests of cuts in project budgets and causing denial of any project extension, despite researchers losing several months of employment. Instead, in many other European countries, agencies and institutions were more supportive and flexible, securing salaries, granting no-cost extensions and postponing deadlines for current and future grants.
Another important topic that was covered in the clinical survey was the impact on patient follow-up and clinical trials during the lockdown. The answer was pretty homogeneous from all participants, with 94% of them highlighting that patients had major concerns with their health status, and around 80% declaring issues with scheduled visits, initiation of new studies and patient recruitment. The majority also reported disruption of investigator-driven studies and contract research organizations site-visits (data not shown).
Overall, our survey has confirmed that the lockdown has been particularly detrimental for younger researchers, including PhD students, postdoctoral researchers, clinical fellows and junior group leaders. This has been previously discussed2–4 and needs to be addressed adequately, with specific attention to minimize the impact on gender equity.1,6 This initiative driven by the YoungEHA committee has highlighted that there is an unmet need for the research community to share experiences, ideas and resources. We believe this is a role that scientific societies should take over more proactively, and this initiative together with those of a few other societies5 is a good starting point. Through surveys and webinars we also collected some inspiring actions that individuals, institutes or societies had launched that we believe could be useful if implemented elsewhere. We have summarized them in Table 1, along with examples for resources.
In conclusion, we believe the unique and dramatic situation we have been facing has amplified some issues basic and clinical research already had, but has also added new challenges. The pause in laboratory and clinical research, that lasted more than two months in most European countries, is only slowly resuming with an uncertain pace and future. Indeed, we are still going through a very difficult situation that is still putting a lot of pressure on the research system and the researchers. Thus, the open exchange of ideas and suggestions among researchers is now more relevant than ever to find strategies to minimize the impact. Particularly, we as early career researchers should empower ourselves and raise our voice to be heard, as we are essential pieces in reshaping the research culture, driving the changes needed. Under the auspices of EHA, we were able to contribute to this effort and will continue to do so. Future feedback from additional surveys or other initiatives, along with actions from organizations, institutions and societies are warranted to face the continuous challenges of this pandemic.
Acknowledgements
We would like to thank everyone that shared their experiences in the surveys and all the speakers who participated in the webinars; all members of the YoungEHA committee for their input before and during this initiative; and the EHA staff, particularly Francesco Cerisoli, Deepa Maas-Sundararaman and Esther Sifuma, for their support and contribution.
Footnotes
The authors have indicated they have no potential conflicts of interest to disclose.
AK, LB and AM-D are members of the Young European Hematology Association committee, @young_eha, The Hague, The Netherlands.
References
- 1.Minello A. The pandemic and the female academic. Nature. 2020;April 17. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 2.Ahmed MA, Behbahani AH, Brückner A, et al. The precarious position of postdocs during COVID-19. Science. 2020;368:957–958. [DOI] [PubMed] [Google Scholar]
- 3.Levine RL, Rathmell WK. COVID-19 impact on early career investigators: a call for action. Nature Rev Cancer. 2020;20:357–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gibson EM, Bennett FC, Gillespie SM, et al. How support of Early Career researchers can reset science in the post-COVID19 world. Cell. 2020;181:1445–1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Waterhouse DM, Harvey RD, Hurley SM, et al. Early impact of COVID-19 on the conduct of oncology clinical trials and long-term opportunities for transformation: findings from an American Society of Clinical Oncology survey. JCO Oncol Pract. 2020;16:417–421. [DOI] [PubMed] [Google Scholar]
- 6.Malisch JL, Harris BH, Sherrer BH, et al. Opinion: In the wake of COVID-19, academia needs new solutions to ensure gender equity. PNAS. 2020;117:15378–15381. [DOI] [PMC free article] [PubMed] [Google Scholar]


