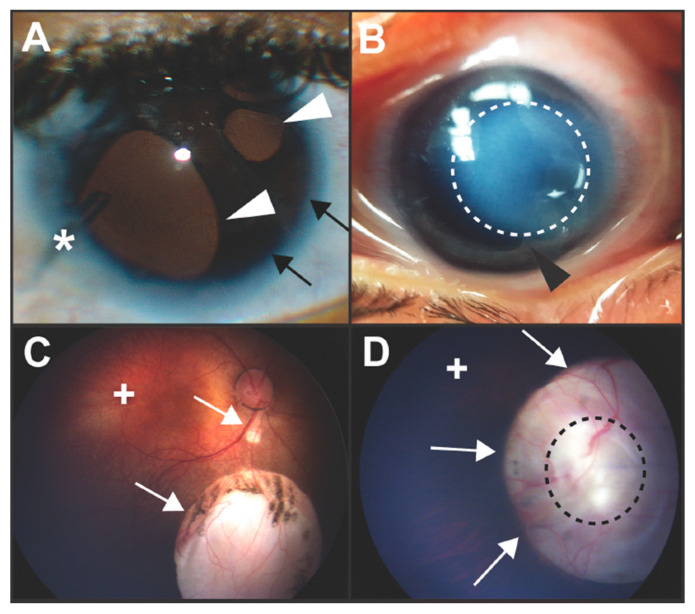
Figure 1.
Clinical images of congenital ocular anomalies. (A) Axenfeld–Rieger syndrome is characterized by Rieger Anomaly (iris hypoplasia resulting in pseudopolycoria and corectopia (white arrowheads)) and Axenfeld Anomaly (anteriorization of Schwalbe’s line of the cornea (posterior embryotoxon, black arrows) with iris adhesions). These defects are due to abnormal migration and differentiation of neural crest cells into the anterior segment of the eye. Over 50% of individuals with Axenfeld–Rieger syndrome develop glaucoma which often requires surgery such as placement of a glaucoma drainage device (asterisk). (B) In Peters anomaly, there is a circumscribed central corneal opacification (outlined by dotted white line) with iris-corneal adhesions (black arrowhead). These anomalies are due to abnormal separation of the lens vesicle from the surface ectoderm resulting in absence of Descemet’s membrane and disruption of neural crest cell migration into the anterior segment. (C,D) Colobomas are due to incomplete closure of the ocular fissure and can affect the iris, zonules, retina, choroid, and optic nerve. Chorioretinal colobomas are inferior to the optic nerve and are characterized by an area that is devoid of retina and choroid (C, white arrows). In these types of coloboma, the macula (+) which accounts for central vision, is typically not affected. Optic nerve colobomas (D, white arrows) can cause severe vision loss especially if the entire optic nerve (outlined by black dotted line) is involved. Although the macula (+) may not be affected, the loss of the ganglion cell axons that comprise the optic nerve limits vision.