Abstract
PURPOSE
The COVID-19 pandemic has severely affected clinical practice in oncology, leading to organizational, ethical, and medical issues. In particular, it has raised challenges in the context of competing care priorities between COVID-19 and cancer treatment. Residents on the front line face difficulties related to increasing care needs and urgent reorganization of health care systems while managing psychological stress and uncertainty. We aimed to evaluate the impact of the COVID-19 pandemic on oncology residents.
METHODS AND MATERIALS
We conducted a national survey (39 questions) in France among oncology and radiation therapy residents to determine the psychological impact and professional difficulties (eg, reassignment, training/research time, supervision, teleworking, management of patients) associated with the first peak of the COVID-19 pandemic.
RESULTS
Overall, 222 residents (medical oncologists, 61%; radiation therapists, 39%) participated in our survey, representing approximately one third of all residents and fellows in France. One third of respondents had been reassigned to a COVID-19 ward. Training and research activity decreased for 89% and 41% of respondents, respectively. Two thirds (70%) of respondents declared that they had faced ethical issues, 35% felt worried about their own health, and 23% experienced psychological distress. According to the Hospital Anxiety and Depression Scale, 32% were anxious and 17% depressed. Consumption of tobacco, psychostimulants, and alcohol increased in 31%, 24%, and 29% of respondents, respectively.
CONCLUSION
French oncology residents were highly affected by the first peak of the COVID-19 pandemic in terms of professional activity and psychological impact. This national survey can be used as a basis for improved management, medical reorganization, and training of residents during the ongoing COVID-19 pandemic.
INTRODUCTION
First detected in China as a respiratory disease in December 2019, SARS-CoV-2 has spread around the world and become a global public health emergency.1 Coronavirus disease 2019 (COVID-19) was declared the first pandemic of the 21st century on March 11, 2020. As of June 15, 2020, 8,020,087 cases had been officially diagnosed worldwide, and 436,167 deaths had occurred,2 including 29,407 in France. With rapid human-to-human transmission, COVID-19 induces a broad range of symptoms of variable severity, from asymptomatic to acute respiratory distress syndrome,1 myocarditis,3 and even neurologic and digestive symptoms.4 Since the first patient was diagnosed in France on January 24, 2020, COVID-19 has spread rapidly, challenging health care systems worldwide.5
CONTEXT
Key Objective
What were the professional difficulties and psychological effects for medical and radiation oncology residents during the first peak of the COVID-19 pandemic?
Knowledge Generated
Seventy-two percent of residents felt uncomfortable with patient management, and 70% had faced ethical issues. Thirty-two percent of residents were classified as anxious and 17% as depressed according to the Hospital Anxiety and Depression Scale.
Relevance
Improved management, medical reorganization, and training of residents are mandatory to minimize the effects of the ongoing COVID-19 pandemic.
In this regard, patients with cancer are a specific population6 with vulnerability to SARS-CoV-2 (both infection and death), but they are also at risk in the context of rationing normal care.7 For these patients, continuing the management of their cancer as a chronic disease is as important as facing the COVID-19 pandemic. Moreover, a shortage of beds and resources resulting from a huge influx of patients with COVID-19 requiring hospitalization and intensive care, along with the perception of cancer as a disease with a poor life expectancy, may lead to limited therapeutic procedures in these patients.
In France, during the first peak of the COVID-19 pandemic, hospitals were rapidly reorganized in terms of oncology and surgery provision, and new intensive care units were created, with reassignment of human and material resources.8,9 Residents and fellows in medical and radiation oncology were then first in line for the management and care of patients with cancer in general hospitals and cancer centers. Although coping with death and end-of-life care is part of the daily practice of young oncologists,10,11 great adaptability and flexibility were asked of them, with potential psychological and physical impacts, as well as an impact on their training. Because residents are at the beginning of their medical careers, they may not have the resources to deal with the potential negative effects of this pandemic. This may negatively affect their careers and their education or even change their career perceptions.12 Therefore, studying how the pandemic is affecting residents is important for every specialty; it has been done for orthopedic,13 urology,14 and dermatology15 residents in different countries.
We conducted a national survey in France to determine the psychological impact on and professional difficulties encountered by medical and radiation oncology residents (eg, reassignment, training/research time, supervision, teleworking, management of patients) during the first peak of the COVID-19 pandemic.
MATERIALS AND METHODS
Our questionnaire was developed and validated by a working group comprising resident and senior clinicians (medical and radiation oncologists) and psychologists. The 39-question survey comprised three sections: demographics of the respondents (11 questions), professional impact (15 questions), and psychological impact (13 questions; Data Supplement).
The target population was composed of French medical and radiation oncology residents who are following a 5-year training schedule. After 6 years of studying medicine, French students pass a national resident ranking examination, which allows them to choose their specialty according to their rank and become residents. At this point, they are mostly between 25 and 30 years of age and begin full-time rotations of 6 months, mainly in their field, under the responsibility of attending physicians.
Anxiety and depression symptoms were assessed using the Hospital Anxiety and Depression Scale (HADS), with significance defined by a score of ≥ 8.16 Subjective quantitative variables were assessed using a virtual visual analog scale (VAS) rated from 0 to 100.
The questionnaire was available for 10 days, from May 4 to 14, 2020. The residents (medical oncologists and radiation therapists) were invited via e-mail, Web site, and social networks through the National Association of Medical Oncology Residents and the Radiation Therapist Residents to participate in this nationwide prospective survey. Three reminder e-mails to complete the survey were sent after the initial mailing to increase the number of responses. Participants were invited to complete the survey using SondageOnline (Zurich, Switzerland), accessible from a computer, tablet, or smartphone; they could log on to the survey through a specific link provided to each group.
Statistical Analyses
Continuous and categorical variables are described as means (ranges [minimum to maximum]/interquartile ranges [IQRs]) and frequencies (percentages), respectively. Subgroup analyses were carried out according to sex, year of residency (first 3 years v last 2 years), medical specialty (medical v radiation oncology), type of hospital (cancer center v public university hospital), and COVID-19 incidence area (high-incidence area v other area). The χ2 test was used for large samples (> 60), and Fisher’s exact test was used for small samples (< 60). For each test, statistical significance was set at a two-sided P value of < .05.
RESULTS
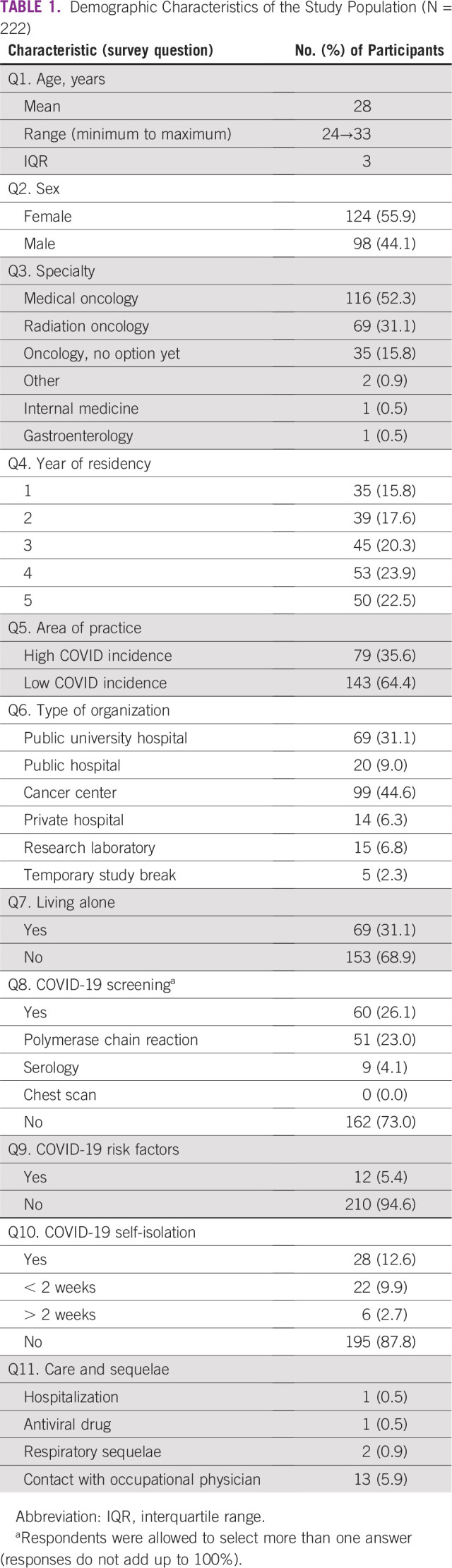
A total of 222 residents participated in this survey; 206 (92.8%) completed the entire questionnaire. Medical oncologists represented 52% of the respondents (n = 111), and 56% of the respondents were women (n = 124). Distribution according to year of residency was well balanced (Table 1). All areas of the country were represented, with 36% of residents working in the three most affected regions (n = 79). The most represented hospitals were public university hospitals (31%; n = 69) and cancer centers (45%; n = 99). Overall, 26% of respondents had been tested for COVID-19 (n = 60), and 13% were socially isolated (n = 28; Table 1).
TABLE 1.
Demographic Characteristics of the Study Population (N = 222)
Since the start of the COVID-19 pandemic, 32% of French residents had been reassigned to a new hospital department (n = 67), mostly voluntarily (82%; n = 55), and 65% managed patients with COVID-19 (n = 138), mainly during night shifts (68%; n = 94). At the time of mid May, 85% of residents (n = 179) had returned to management of patients without COVID-19, and 78% had returned to their previous professional activity (n = 167). Most residents had access to personal protective equipment (94%; n = 201), but this was deemed inadequate in 31% of cases (n = 65), and 53% did not receive proper hygiene training regarding the equipment (n = 112; Table 2).
TABLE 2.
Professional Impact of the COVID-19 Pandemic (N = 222)
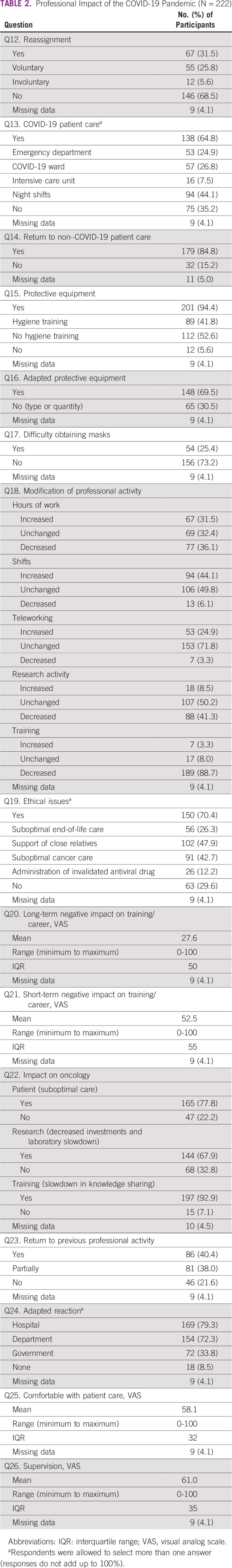
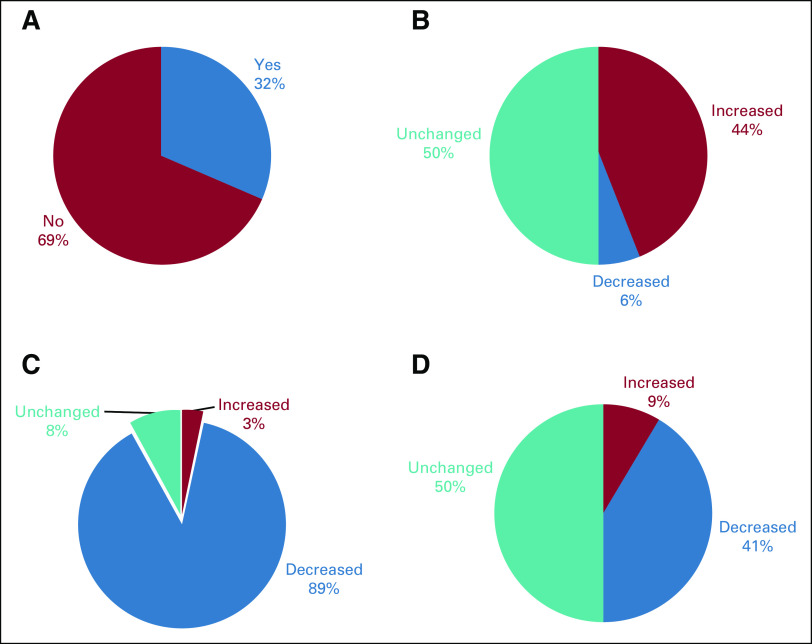
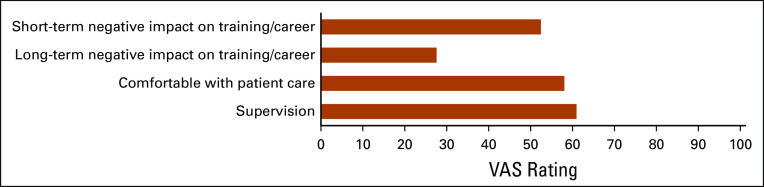
Training and research activities had decreased for 89% (n = 189) and 41% of residents (n = 88), respectively, whereas working hours and night shifts had increased for 31% (n = 67) and 44% of residents (n = 94), respectively (Fig 1). Seventy percent of residents had faced ethical issues (n = 150), mainly related to their ability to provide less support to patients’ relatives (48%; n = 102) and suboptimal cancer treatment (43%; n = 91). Respondents had the feeling that the COVID-19 pandemic might have a negative impact on their training/career in the short term (mean VAS, 52.5; IQR, 55) rather than in the long term (mean VAS, 27.6; IQR, 50) and may negatively affect oncology patients, research, and training in 78%, 68%, and 93% of cases, respectively. In addition, they believed their hospital or department had adapted to respond to COVID-19 in 79% and 72% of cases, respectively, although they felt uncomfortable with patient care (mean VAS, 58.1; IQR, 32) and received less supervision (mean VAS, 61.0; IQR, 35; Table 2; Fig 2). Residents’ opinions about the impact of the COVID-19 pandemic on the future of oncology are shown in Figure 3.
FIG 1.
Professional impact of the COVID-19 pandemic on French oncology residents during the first peak regarding (A) reassignment, (B) shifts, (C) training, and (D) research activities.
FIG 2.
Residents’ opinions about quality of care, supervision, and impact on their career during the first peak of the COVID-19 pandemic. A virtual visual analog scale (VAS) was rated from 0 to 100.
FIG 3.
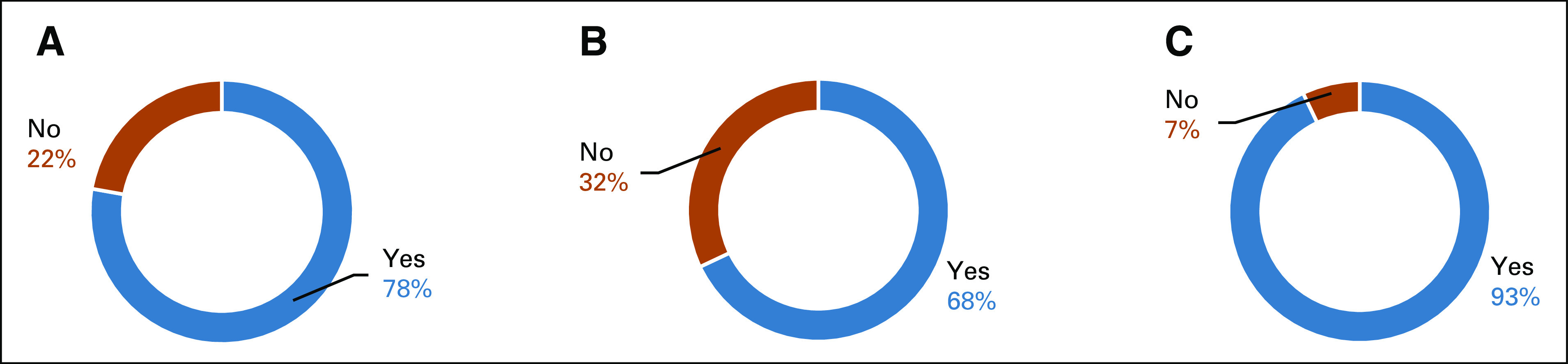
Residents’ opinions about the impact of the COVID-19 pandemic on the future of oncology as regards (A) suboptimal care, (B) cancer research slowdown, and (C) knowledge sharing slowdown.
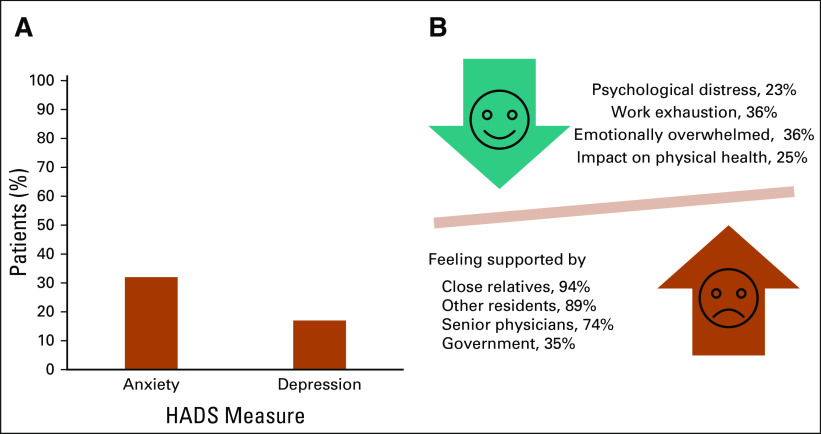
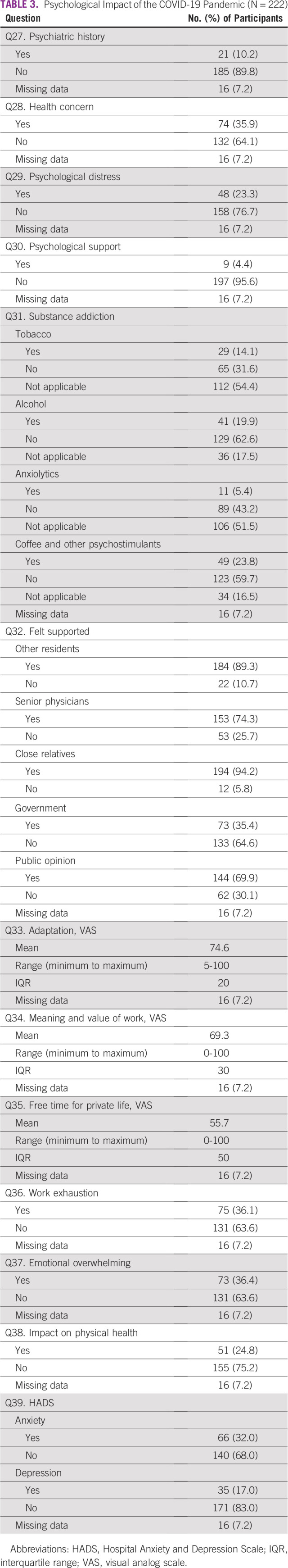
Although residents felt they had adapted (mean VAS, 74.6; IQR, 20) and were supported by colleagues and close relatives (89% and 94%, respectively), the COVID-19 pandemic affected their psychological health. One third (36%) of residents felt exhausted and emotionally overwhelmed, with limited time for their private life (mean VAS, 55.7; IQR, 50), and 25% said their work had been affected by their physical health. As a result, 32% of residents were classified as anxious (n = 66) and 17% as depressed (n = 35) according to HADS (Fig 4). Furthermore, among tobacco, alcohol, and psychostimulant users, 31%, 24%, and 29% increased their consumption during the COVID-19 pandemic. However, only nine residents (4%) received psychological support from a professional (Table 3).
FIG 4.
Psychological impact of the first peak of the COVID-19 pandemic on oncology residents. (A) Prevalence of anxiety and depression symptoms among residents using the Hospital Anxiety and Depression Scale (HADS), and (B) representation of the support and consequences of the first peak of the COVID-19 pandemic.
TABLE 3.
Psychological Impact of the COVID-19 Pandemic (N = 222)
Subgroup Analyses
Subgroup analysis by specialty revealed that medical oncologists were more frequently reassigned (42% v 20% for radiation oncologists; P = .003) and consequently had longer working hours (63% v 23%; P = .04) and night shifts (53% v 36%; P < .001). In addition to this inflated workload, their research activity was affected (6% v 21%; P = .02), they felt more comfortable managing patients with COVID-19 (mean VAS, 63 v 52 of 100; P = .003), and they had less free time for their private life (mean VAS, 52 v 64 of 100; P = .01) compared with radiation oncologists. Men felt more closely supervised than women (mean VAS, 66 v 57 of 100; P = .002). Older residents were more frequently reassigned (52% v 14% for younger residents; P < .0001), more frequently had adapted personal protective equipment (80% v 61%; P = .0001), practiced more teleworking (33% v 18%; P = .01), felt more comfortable managing patients with COVID-19 (mean VAS, 54 v 63 of 100; P = .01), felt they had better adapted (mean VAS, 73 v 78 of 100; P = .03), and had more free time for their private life (mean VAS, 54 v 62 of 100; P = .03) than younger residents.
Residents working in cancer centers were more often reassigned (33% v 16% in public university hospitals; P = .02), had fewer night shifts (34% v 55%; P = .006), more frequently increased their alcohol consumption (41% v 10%; P = .01), felt they had better adapted (mean VAS, 75 v 70 of 100; P = .05), and had more free time for their private life (mean VAS, 60 v 51 of 100; P = .067) compared with residents in public university hospitals. French residents working in the top three high-incidence COVID-19 areas were more frequently reassigned (44% v 25% in other areas; P = .004), had more extended working hours (48% v 23%; P = .0001) and a higher number of night shifts (55% v 38%; P = .02); were more likely to have increased their consumption of psychostimulants (32% v 20%; P = .04), were more closely supervised (mean VAS, 65 v 59 of 100; P = .07), and had less free time for their private life (mean VAS, 49 v 60 of 100; P = .014) compared with those working in other areas.
DISCUSSION
Our survey highlights how deeply the first peak of the COVID-19 pandemic affected French medical oncology and radiation oncology residents. National and international practice guidelines were rapidly published and helped clinicians to adapt their management of patients with cancer.8,17 However, many aspects of the aftermath were underestimated, especially concerning the adaptation of residents to the COVID-19 pandemic.
During the first peak, oncology residents had to adapt and change their practice with an increased workload, either being on the front line to manage patients with COVID-19 or managing patients with cancer, whose treatments and complications had not gone away. Importantly, more than one third of oncology residents had been asked to help outside their field of competence, in an intensive care unit or dedicated COVID-19 unit. Reorganization of work in an emergency put residents under pressure, especially those less experienced, with 72% feeling uncomfortable with patient management and lacking educational support. Nevertheless, 85% of residents had returned to their original ward by May 2020.
Mental health issues were among the most striking results. Despite the high rate of psychological problems, only 4% sought psychological support from a professional during the pandemic. It is particularly noteworthy that no psychological support units are dedicated to young oncologists, despite the uniqueness of the profession regarding mental health. Results presented at the European Society for Medical Oncology (ESMO) 2014 Congress showed that 45% of European oncologists age < 40 years had emotional exhaustion, and 74% reported no access to adequate support.18 According to the WHO, in addition to SARS-CoV-2, viral diseases in general threaten public health, with a consistent risk of new viruses emerging. In their meta-analysis, Kisely et al19 found that emergent viruses caused psychological distress among medical staff. Risk factors for this distress included young age, being more junior, extended quarantine, and lack of practical support. The National French Residents Union presented data during the pandemic, with surprising results: 72% of French residents across all disciplines felt anxious and 37% depressed compared with the 32% and 17% of oncology residents, respectively, in our survey.20 This difference may be a result of the specific training of oncology residents, with an already developed level of compassion, that may be protective from psychological distress. In a study by Lai et al21 conducted in China, 45% of health workers showed anxiety and 50% were depressed. These results were worse in the most affected regions and among workers directly exposed to the virus, which is consistent with our data, although the incidence of anxiety and depression was lower in our population. However, these investigators surveyed health care workers in February, whereas we launched our questionnaire in May, after the peak of the epidemic had been reached. French public health services conducted a survey among the general population, with HADS scores decreasing dramatically at the end of quarantine, in early May.22 This suggests that specific psychological support from a professional should be provided during the pandemic and indeed throughout residency.
In addition, it is striking to note the physical health risks encountered by oncology residents. During the first peak of the pandemic, as with other health workers in France, they lacked supplies of personal protective equipment against SARS-CoV-2 (eg, masks) and had to self-learn how to protect themselves. Insufficient equipment and education might have contributed to the proportion of residents (13%) who had to self-isolate with COVID-19 symptoms. In addition, from the long-term perspective, the increased consumption of addictive and toxic substances during the COVID-19 pandemic is a particular concern for young oncologists.
Besides the health issues, young oncologists are currently worried about the future of their specialty and their training. Nearly a whole semester of theoretic and practical training was missed, and research laboratories were closed for those preparing for MSc or PhD degrees. Uncertainty over future clinical and working conditions and careers, changes to legislation with regard to social distancing, and disruption of education and postgraduate training has led to anxiety and apprehension among junior physicians.23 However, young oncologists also acquired new skills, such as teleworking and treatment prioritorization,24 and a lot of new questions are pending about cancer and COVID-19. As lockdown and protective measures are removed entirely, oncology residents will need the support of senior clinicians to catch up with their training and research schedules.25 A shift toward online medical training is ongoing,26 and a balance will have to be found between in-person and online courses. Moreover, during the pandemic, major cancer meetings were replaced by virtual meetings (eg, American Association for Cancer Research 2020, ASCO 2020, ESM0 2020); if these digital congresses persist, they may in the longer term have positive results for residents’ educational training, because attendance at these major international congresses was historically limited for residents.
Our study has several limitations. First, the timeframe for completing the questionnaire may have had an influence, and the results would probably have been different if the questionnaire had been completed between March 15 and 30, 2020, before the epidemic peak in France. Timing of a questionnaire is crucial against a fast-moving landscape such as a pandemic that requires great adaptability, and our results might have been more significant because the survey was conducted during the epidemic peak. Nevertheless, it allows us to appreciate the feeling of residents during the period with the highest COVID-19 activity. Second, because it was an online questionnaire, a nonresponse bias is inevitable. There were few missing data, and the questionnaire was designed to be filled in quickly. Third, we lack longitudinal follow-up, even though it was not a goal of our study, but depending on the evolution of the COVID-19 pandemic in France, other surveys will be performed. Finally, not all French oncology residents responded to the survey, but the 222 respondents, from all over France, represented more than one third of all French oncology and radiation therapy residents, making our survey highly representative of this population.
In conclusion, this national survey raises concerning questions with regard to the professional difficulties and mental and physical issues faced by oncology and radiation therapy residents. Young oncologists show strong resilience, and they must be mentored by senior clinicians to overcome the missed training and research, thereby minimizing the impact of the pandemic on their future practice. This survey can be used as the basis for improved management, medical reorganization, and training of residents during the ongoing COVID-19 pandemic.
ACKNOWLEDGMENT
We thank all the French residents in oncology who answered the questionnaire, the National French Residents Union for providing analyses of their survey, and Newmed Publishing Services for language editing.
EQUAL CONTRIBUTION
M.H. and A.B. contributed equally to this work.
PRIOR PRESENTATION
Presented at the American Association for Cancer Research Virtual Meeting: COVID-19 and Cancer, July 20-22, 2020.
AUTHOR CONTRIBUTIONS
Conception and design: Marc Hilmi, Alice Boilève, Anabelle Ducousso, Cindy Neuzillet, Natacha Naoun
Collection and assembly of data: Marc Hilmi, Alice Boilève, Natacha Naoun
Data analysis and interpretation: Marc Hilmi, Alice Boilève, Morgan Michalet, Anthony Turpin, Cindy Neuzillet, Natacha Naoun
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/site/misc/authors.html.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Anthony Turpin
Honoraria: Amgen, Merck Serono, Servier
Consulting or Advisory Role: Amgen
Travel, Accommodations, Expenses: AstraZeneca, Pfizer, Sanofi, Merck
Cindy Neuzillet
Honoraria: Servier, Roche, AstraZeneca, Bristol Myers Squibb, Amgen, Merck, MSD Oncology, Novartis, Pierre Fabre, Incyte, Mylan, Baxter, Fresenius Kabi, Nutricia
Research Funding: Roche (Inst), AstraZeneca (Inst), OSE Immunotherapeutics (Inst)
Travel, Accommodations, Expenses: OSE Immunotherapeutics, MSD Oncology, Merck, Amgen, Mylan
No other potential conflicts of interest were reported.
REFERENCES
- 1.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Worldometer: COVID-19 coronavirus pandemic. https://www.worldometers.info/coronavirus/
- 3.Chen C, Zhou Y, Wang DW. SARS-CoV-2: A potential novel etiology of fulminant myocarditis. Herz. 2020;45:230–232. doi: 10.1007/s00059-020-04909-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong SH, Lui RN, Sung JJ. Covid-19 and the digestive system. J Gastroenterol Hepatol. 2020;35:744–748. doi: 10.1111/jgh.15047. [DOI] [PubMed] [Google Scholar]
- 5.Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 6.Wang H, Zhang L. Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020;21:e181. doi: 10.1016/S1470-2045(20)30149-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. doi: 10.1016/j.annonc.2020.03.296. Zhang L, Zhu F, Xie L, et al: Clinical characteristics of COVID-19-infected cancer patients: A retrospective case study in three hospitals within Wuhan, China. Ann Oncol 31:894-901, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.You B, Ravaud A, Canivet A, et al. The official French guidelines to protect patients with cancer against SARS-CoV-2 infection. Lancet Oncol. 2020;21:619–621. doi: 10.1016/S1470-2045(20)30204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.El Amrani M, Truant S, Turpin A. COVID 19 and cancer: What are the consequences of the cancer care reorganization? [in French] Bull Cancer. 2020;107:538–540. doi: 10.1016/j.bulcan.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zambrano SC, Chur-Hansen A, Crawford GB. On the emotional connection of medical specialists dealing with death and dying: A qualitative study of oncologists, surgeons, intensive care specialists and palliative medicine specialists. BMJ Support Palliat Care. 2012;2:270–275. doi: 10.1136/bmjspcare-2012-000208. [DOI] [PubMed] [Google Scholar]
- 11.Jackson VA, Mack J, Matsuyama R, et al. A qualitative study of oncologists’ approaches to end-of-life care. J Palliat Med. 2008;11:893–906. doi: 10.1089/jpm.2007.2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Byrnes YM, Civantos AM, Go BC, et al. Effect of the COVID-19 pandemic on medical student career perceptions: A national survey study. Med Educ Online. 2020;25:1798088. doi: 10.1080/10872981.2020.1798088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kogan M, Klein SE, Hannon CP, et al. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28:e456–e464. doi: 10.5435/JAAOS-D-20-00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Porpiglia F, Checcucci E, Amparore D, et al. Slowdown of urology residents’ learning curve during the COVID-19 emergency. BJU Int. 2020;125:E15–E17. doi: 10.1111/bju.15076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. doi: 10.1111/ced.14365. [epub ahead of print on July 3, 2020] [DOI] [Google Scholar]
- 16.Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 17. European Society for Medical Oncology: Cancer patient management during the COVID-19 pandemic. https://www.esmo.org/guidelines/cancer-patient-management-during-the-covid-19-pandemic?hit=ehp.
- 18.Banerjee S, Califano R, Corral J, et al. Professional burnout in European young oncologists: Results of the European Society for Medical Oncology (ESMO) Young Oncologists Committee Burnout Survey. Ann Oncol. 2017;28:1590–1596. doi: 10.1093/annonc/mdx196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. doi: 10.1136/bmj.m1642. [epub ahead of print on May 5, 2020] [DOI] [Google Scholar]
- 20. InterSyndicale Nationale des Internes: Vécu psychologique de l’épidémie COVID-19. https://isni.fr/vecu-psychologique-de-lepidemie-covid/
- 21.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Santé Publique France: Contenu du questionnaire. https://www.santepubliquefrance.fr/etudes-et-enquetes/covid-19-une-enquete-pour-suivre-l-evolution-des-comportements-et-de-la-sante-mentale-pendant-l-epidemie#block-242829.
- 23.Ding A, Zhang Y. Impact of cancelling foundation year rotations due to the COVID-19 outbreak in the UK. Postgrad Med J. 2020;96:434–435. doi: 10.1136/postgradmedj-2020-137775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cherny NI, Dafni U, Bogaerts J, et al. ESMO–Magnitude of Clinical Benefit Scale version 1.1. Ann Oncol. 2017;28:2340–2366. doi: 10.1093/annonc/mdx310. [DOI] [PubMed] [Google Scholar]
- 25.Representatives of the STARSurg Collaborative, EuroSurg Collaborative, and TASMAN Collaborative Medical student involvement in the COVID-19 response. Lancet. 2020;395:1254. doi: 10.1016/S0140-6736(20)30795-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sandhu N, Frank J, von Eyben R, et al. Virtual radiation oncology clerkship during the COVID-19 pandemic and beyond. Int J Radiat Oncol Biol Phys. 2020;108:444–451. doi: 10.1016/j.ijrobp.2020.06.050. [DOI] [PMC free article] [PubMed] [Google Scholar]