Fig. 5.
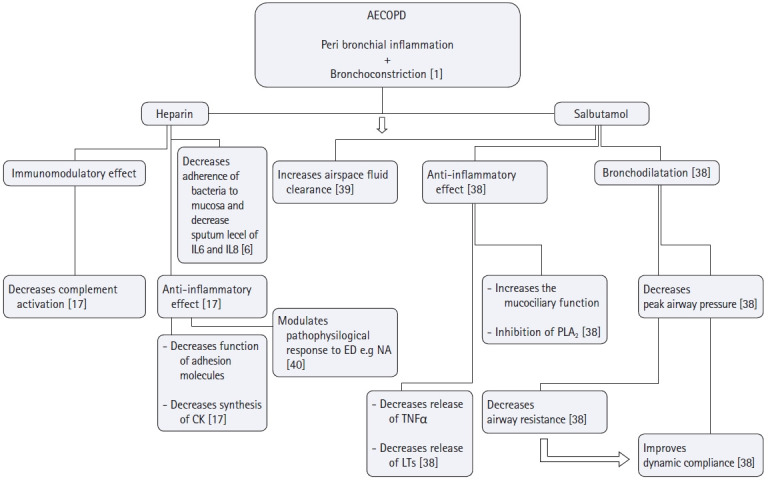
Possible roles of heparin and salbutamol nebulization in targeting the pathophysiology of AECOPD. Main targets of heparin and salbutamol in the management of AECOPD are to hit its two pathological components; peribronchial inflammation and bronchoconstriction. As for heparin, it prevents the adhesion of Pseudomonas aeruginosa, Burkholderia cepacia, Burkholderia pseudomalleior Legionella pneumophilato bronchial mucosa and decrease sputum levels of IL-6 and IL-8 confirming its anti-inflammatory action. Heparin's anti-inflammatory effect is exerted also by other mechanisms; i) Heparin preparations have been shown to inhibit chemokine synthesis, as well as chemokine function (a cytokine that regulates the extravasations of cells from blood stream to tissues), ii) Heparin inhibits adhesion molecules (which with cytokines are essential for the extravasations of neutrophils to tissues), iii) Animal studies highlighted the effect of low molecular weight heparin on the modulation of pathophysiologic response to endotoxins by decreasing neutrophils adhesion, solubilization of TNF-α receptors and regulation of thromoboxane A2 biosynthesis. Salbutamol on the other hand through its bronchodilator effect improves dynamic compliance secondary to the decrease of peak airway pressure, it also possesses a unique anti-inflammatory effect by inhibiting the mast cell release to histamine and its inhibitory effect on phospholipase A2 subsequently decreasing the microvascular permeability and enhancing the air space fluid clearance. AECOPD: acute exacerbation chronic obstructive pulmonary disease, IL-6: Interleukin 6, IL-8: Interleukin 8, CK: cytokines, ED: endotoxins, NA: neutrophil aggregation, TNFα: tissue necrosis factor α, LTs: Leukotrienes, PLA2: Phospholipase A2.
