Abstract
OBJECTIVES
Italy has been one of the countries most severely affected by the coronavirus disease 2019 (COVID-19). The Italian government was forced to introduce quarantine measures quickly, and all elective health services were stopped or postponed. This emergency has dramatically changed the management of paediatric and adult patients with congenital heart disease. We analysed data from 14 Italian congenital cardiac surgery centres during lockdown, focusing on the impact of the pandemic on surgical activity, patients and healthcare providers and resource allocation.
METHODS
Fourteen centres participated in this study. The period analysed was from 9 March to 4 May. We collected data on the involvement of the hospitals in the treatment of patients with COVID-19 and on limitations on regular activity and on the contagion among patients and healthcare providers.
RESULTS
Four hospitals (29%) remained COVID-19 free, whereas 10 had a 39% reduction in the number of beds for surgical patients, especially in the northern area. Two hundred sixty-three surgical procedures were performed: 20% elective, 62% urgent, 10% emergency and 3% life-saving. Hospital mortality was 0.4%. Compared to 2019, the reduction in surgical activity was 52%. No patients operated on had positive test results before surgery for severe acute respiratory syndrome coronavirus 2, the virus responsible for COVID-19. Three patients were infected during the postoperative period. Twenty-nine nurses and 12 doctors were infected. Overall, 80% of our infected healthcare providers were in northern centres.
CONCLUSIONS
Our study shows that the pandemic had a different impact on the various Italian congenital cardiac surgery centres based on the different patterns of spread of the virus across the country. During the lockdown, the system was able to satisfy all emergency clinical needs with excellent results.
Keywords: Coronavirus disease 2019, Pandemic, Congenital heart disease, Cardiac surgery
Starting from Wuhan (China) in December 2019 [1], the disease called coronavirus disease 2019 (COVID-19) has rapidly become a worldwide pandemic with currently over 12 million cases globally (15 June).
INTRODUCTION
Starting from Wuhan (China) in December 2019 [1], the disease called coronavirus disease 2019 (COVID-19) has rapidly become a worldwide pandemic with currently over 12 million cases globally (15 June). By the end of February 2020, Italy became one of the most affected countries worldwide with over 220 000 patients infected and 32 000 deaths, forcing the Italian government to quickly introduce on 9 March emergency quarantine and isolation measures [2]. The treatment and management of patients with COVID-19 became a priority. As a result, all elective health services were stopped or postponed. This emergency situation dramatically changed the treatment of children and adults with congenital heart disease (CHD) requiring surgery or interventional procedures. All planned operations were postponed to free up intensive care unit (ICU) beds for the treatment of patients with COVID-19. Many hospitals converted operating theatres and recovery areas into areas for additional ICU beds. The CHD community was forced to face a sudden and unknown challenge in terms of reorganization, relocation of resources and ways to protect healthcare providers, families and patients from infection. Some units, like the ones in Lombardy, were closed and merged using the hub-and-spoke model [3], whereas others underwent a drastic reduction in their activity. At the same time, it was necessary to guarantee adequate health services for those patients, especially newborns and infants, who required surgery within a stringent time frame.
After 8 weeks of complete lockdown, a critical reduction in the number of hospitalized patients with COVID-19 was registered in Italy, allowing the start of a new healthcare management phase (phase 2). In this context, on behalf of the congenital domain of the Italian Society of Cardiac Surgery, we analysed the data from 14 Italian cardiac surgery centres dedicated to CHD, focusing on the impact of the pandemic on surgical activity and results, on protection of patients and healthcare providers and on variations in resource allocation.
METHODS
Using a questionnaire, we conducted a descriptive and retrospective survey on the impact of the COVID-19 pandemic on the activity of all Italian cardiac surgery centres dedicated to CHD.
Through official decrees, the Ministry of Health and the local health departments indicated the ways of working to be followed for the duration of the complete lockdown:
Classification of patients/illnesses into emergency, urgent, deferrable and with prenatal diagnosis and scheduled birth and
Authorization for interventions only for emergency and urgent patients who could not be postponed beyond 60 days.
In Lombardy, the regional health department introduced from 9 March the hub-and-spoke model, suggesting:
Extensive collaboration between the teams, including working together in the operating theatre and catheterization laboratory,
Daily official communication about the number of ICU beds available in the respective centres and
Frequent telemeetings among surgical centres and paediatric cardiology and neonatology units to discuss patient management strategy, transfer timing and scheduled births.
The extracorporeal membrane oxygenation (ECMO), transplant, ventricular assist device and heart failure programmes were not reorganized. Currently, there is no national database for cardiac surgery activity in Italy. Therefore, data were collected through a survey search realized by written inquiry to each congenital cardiac surgery unit (Supplementary Material, Appendix S1). We analysed data during the lockdown from 9 March 2020 to 4 May 2020 and compared the data to data from the same period in the year 2019.
The survey was divided into 4 sections: general data of the participating centres, reorganization of the centres and possible relocation of resources during the lockdown, surgical activity and data about healthcare providers.
RESULTS
Italy, with over 60 million inhabitants and a birth rate of 1.29, has 15 cardiac surgery units dedicated to CHD (Fig. 1). Among these, 4 units (27%) operate in a children’s hospital, whereas 11 units (73%) operate in institutions offering both adult acquired and congenital cardiac surgery services. Ten units are within general hospitals, 3 are in university centres and 2 are in private hospitals accredited with the National Health System. The geographical distribution includes 7 centres in northern, 4 in central and 4 in southern Italy (Fig. 1). An average of 3500 patients with CHD are operated on in these units each year (unpublished official data from Italian Society of Cardiac Surgery—Congenital Domain, presented at the XXIX National Meeting of Societa’ Italiana di Chirurgia Cardiaca-SICCH, Rome 2018).
Figure 1:
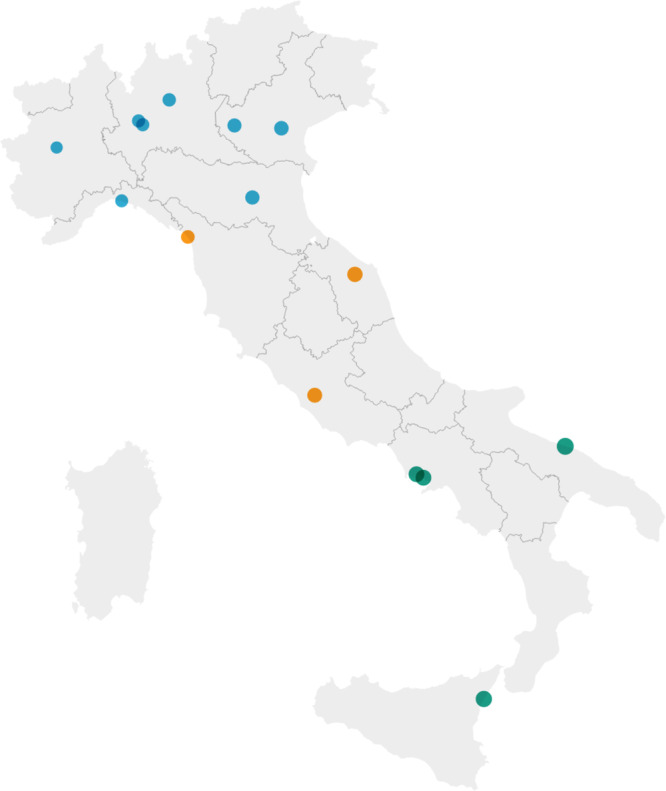
Congenital cardiac surgery units in Italy. Blue: centres in the northern area; orange: centres in the central area; green: centres in the southern area.
Fourteen centres (14/15 = 93%) agreed to participate in the survey and contributed to the data collection. In terms of structural organization, 7 units (50%) have ICUs fully dedicated to patients with CHD, whereas 7 have mixed ICUs with congenital and acquired patients. In 11 centres (79%), the ICU is managed by intensivists, whereas in 3 (21%), by congenital cardiac surgeons. The number of ICU and ward beds and the number of cardiac surgery and anaesthesiology staff dedicated to CHD for each centre are summarized in Table 1.
Table 1:
Characteristics of Italian congenital cardiac surgery centres
| Hospital | Type | 2019 cases | ICU beds | Ward beds | Surgeons | Anaesthetists |
|---|---|---|---|---|---|---|
| 1 | M | 446 | 8 | 40 | 4 | 5 |
| 2 | M | 192 | 4 | 7 | 2 | 4 |
| 3 | M | 186 | 10 | 10 | 3 | 7 |
| 4 | M | 208 | 3 | 8 | 2 | 3 |
| 5 | M | 302 | 3 | 6 | 3 | 6 |
| 6 | P | 200 | 5 | 10 | 5 | 8 |
| 7 | M | 334 | 5 | 24 | 5 | 4 |
| 8 | M | 221 | 7 | 26 | 4 | 9 |
| 9 | M | 260 | 4 | 19 | 5 | 6 |
| 10 | P | 600 | 16 | 32 | 9 | 18 |
| 11 | M | 67 | 1 | 2 | 2 | 0 |
| 12 | M | 300 | 7 | 12 | 5 | 9 |
| 13 | M | 46 | 4 | 10 | 4 | 0 |
| 14 | P | 164 | 4 | 12 | 3 | 6 |
| TOT | 3526 | 81 | 218 | 56 | 85 |
ICU: intensive care unit; M: mixed (adult and paediatric); P: paediatric.
Coronavirus disease 2019 reorganization
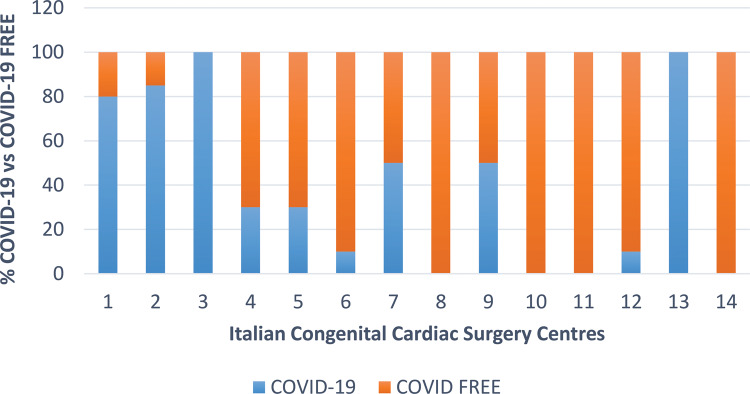
Emergency quarantine measures had different applications across northern, central and southern Italy. Four hospitals remained completely COVID-19 free (none in the north), whereas in the other ten, 39% of all hospital beds were converted to beds for patients with COVID-19 (mean number of beds reallocated in the north was 55%; centre, 17%; and south, 27%) (Fig. 2).
Figure 2:
Hospital reconfiguration after coronavirus disease 2019 emergency.
A reduction in the number of ICU beds was observed in 8 hospitals (57%); a reduction in the number of operating theatres, in 6 (42%); and a reduction in the number of ward beds in 5 hospitals (35%).
Because the Lombardy region was the one most profoundly affected in terms of infections and deaths, it also experienced the most radical transformation with the adoption of the hub- and-spoke model. Two of 3 units were closed, and urgent surgical activity, including reassignment of the cardiac surgeons, was concentrated in a third unit [4, 5].
Ten units (71%) comprised protected separated areas in the ICU and in the wards for possible patients with CHD who had positive test results for COVID-19. Seven centres (50%) dedicated an operating theatre only for treatment of eventual CHD patients infected with severe acute respiratory syndrome coronavirus 2. All data relative to the redistribution enacted to deal with the COVID-19 emergency are reported in Table 2.
Table 2:
Congenital cardiac surgery units undergoing reduction in resources during lockdown
| Hospital | ICU beds, n (%) | Ward beds, n (%) | Operating theatre, n (%) |
|---|---|---|---|
| 1 | 0 (0) | 20 (50) | 1 (50) |
| 2 | 4 (100) | 4 (57) | 3 (80) |
| 3 | 6 (60) | 10 (100) | 2 (100) |
| 4 | 1 (33) | 4 (50) | 0 (0) |
| 5 | 2 (66) | 0 (0) | 3 (60) |
| 6 | 1 (20) | 0 (0) | 0 (0) |
| 7 | 4 (80) | 0 (0) | 1 (20) |
| 8 | 0 (0) | 0 (0) | 0 (0) |
| 9 | 2 (50) | 4 (21) | 0 (0) |
| 10 | 0 (0) | 0 (0) | 0 (0) |
| 11 | 0 (0) | 0 (0) | 0 (0) |
| 12 | 0 (0) | 0 (0) | 0 (0) |
| 13 | 4 (100) | 10 (100) | 1 (100) |
| 14 | 0 (0) | 0 (0) | 0 (0) |
ICU: intensive care unit.
Patients
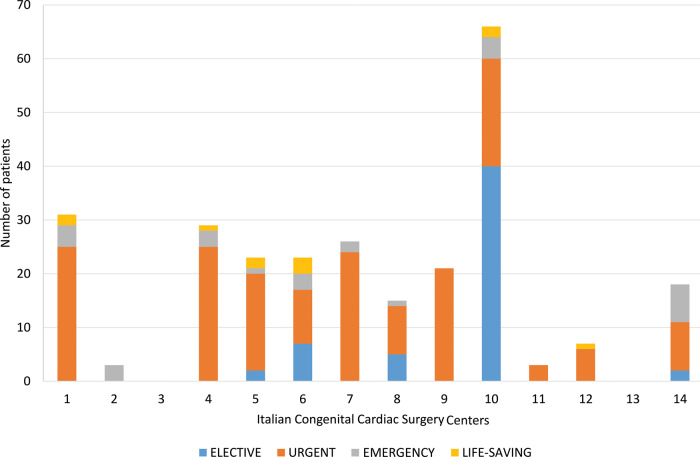
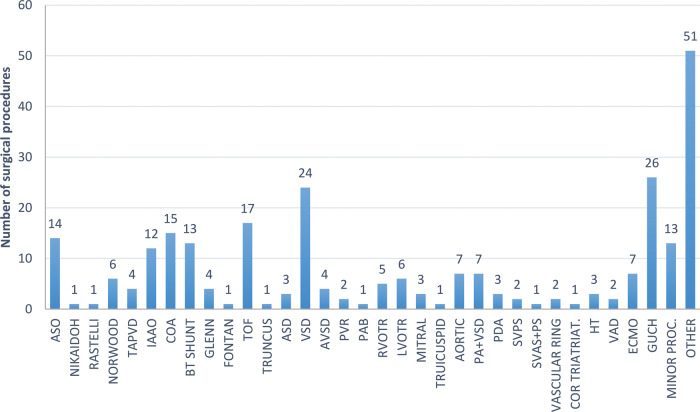
All centres had strictly enforced restricted access to patients. Two centres (14%) completely prevented parents from visiting. In 7 centres, all patients and the accompanying parent were tested for the virus preoperatively. In 3 centres and in 4 hospitals that were COVID-19 free, the test was done only in the presence of symptoms and/or fever. The test used in all centres was the real time-polymerase chain reaction, commonly called the nasopharyngeal swab. In terms of patient selection, 9 centres (64%) strictly followed the rules suggested by the Ministry of Health and the local health departments. For the patients already hospitalized at the beginning of lockdown, 8 centres (57%) discharged all elective cases, whereas the other 6 (43%) operated on the patients. From 9 March to 4 May, 263 surgical procedures were performed: 56 (20%) elective, 170 (62%) urgent, 28 (10%) emergency and 9 (3%) life-saving (Fig. 3). Sixty-six (25%) were neonates; 83 (32%) were infants; 88 (33%) were paediatric patients; and 26 (10%) were adults with CHD (ACHD). Compared to the same period of time in 2019, there was a reduction of 52% in the surgical procedures performed (51% in the north, 43% in the central region and 66% in the south). The more frequent surgical procedures were performed in ACHD, followed by the arterial switch operation. All types of procedures performed are reported in Fig. 4. Despite the difficult period, 4 heart transplants and 7 non-virus-related ECMO procedures were also performed with good results. In 80% of cases, the patients operated on were from the same area of the hospital. There was an 85% decrease in patients operated on from abroad.
Figure 3:
Number and type (priority) of surgical procedures performed during the lockdown.
Figure 4:
Surgical procedures performed during the lockdown. ASD: atrial septal defect; ASO: arterial switch operation; AVSD: atrioventricular septal defect; BT: Blalock–Taussig; COA: coarctation; ECMO: extracorporeal membrane oxygenation; GUCH: grown-up congenital heart disease; HT: heart transplant; IAAO: interrupted aortic arch; LVOTR: left ventricular outflow tract repair; PA + VSD: pulmonary atresia and ventricular septal defect; PAB: pulmonary artery banding; PDA: patent ductus arteriosus; proc.: procedure; PVR: pulmonary valve replacement; RVOTR: right ventricular outflow tract repair; SVAS + PS: supravalvular aortic stenosis and pulmonary stenosis; SVPS: supravalvular pulmonary stenosis; triatriat: triatriatum; TAPVD: total anomalous pulmonary vein drainage; TOF: tetralogy of Fallot; VAD: ventricular assist device; VSD: ventricular septal defect.
The overall hospital mortality was 0.4% (1/263). A 4-month-old patient with Williams syndrome and severe biventricular dysfunction underwent ascending aorta and pulmonary artery enlargement and died on postoperative day 15 of refractory low cardiac output syndrome.
No patients operated on had positive test results for COVID-19 preoperatively. Three patients turned positive during the postoperative period. In 1 case, a 19-year-old patient who had a heart transplant for failing Fontan required ECMO support for 8 days. The patient, with no signs of pneumonia, had a favourable postoperative course. The other 2 patients were ACHD who became positive during the postoperative period without any impact on the clinical course. Two neonates had parents who tested positive at the time of admission. Both newborns had negative test results before surgery and remained negative until discharge.
Healthcare providers
During the period analysed, body temperatures were monitored daily in 9 centres (64%), whereas nasopharyngeal swabs were obtained only in case of contact with infected patients in 86% of the units (12/14). Only 1 unit repeated the swabs every 7 days for all healthcare providers.
Although the use of personal protective equipment was mandatory in 11 centres (79%), its availability, especially during the first 2 weeks of lockdown, was sufficient in only 9 hospitals (64%), especially in the northern units (43%). Seventy-eight percentage of the respondents believed that their hospital provided sufficient information to allow them to avoid infection, but only 64% believed they received sufficient personal protective equipment. Only 57% (8/14) of the centres received adequate and timely guidelines to avoid contagion, and 29% (4/14) received information only after the first patients with COVID-19 were hospitalized.
All centres adopted regional protocols, but in 70% (8/14) of the units, these protocols were adjusted according to the respective local hospital healthcare departments. One centre adopted specific protocols developed by cardiac surgery and cardiology department staff.
The pandemic often caused staff relocation to deal with the emergency. In all units, cardiologists remained committed entirely to the care of congenital cardiac patients, whereas 57% of the anaesthesiologists, 50% of the nurses and 28% of the perfusionists were moved to COVID-19 patient care. Only 7% of congenital cardiac surgeons were relocated to COVID-19 units.
In the 14 centres, during the lockdown period, 29 nurses and 12 physicians dedicated to CHD care become infected (25 nurses and 9 doctors in north, 4 nurses and 3 doctors in the rest of Italy). Two anaesthesiologists from the northern area required hospitalization and non-invasive ventilation whereas all the other healthcare providers were treated at home. All the contagion occurred in the first 2 weeks of the emergency.
DISCUSSION
The COVID-19 pandemic, with its rapid worldwide spread, has had a tremendous impact on all of society, the economy and the healthcare systems [4]. By the end of February 2020, Italy became one of the most affected countries, forcing the Italian government to introduce emergency quarantine measures on 9 March [2]. The system’s ability to respond to the unprecedented circumstances has been under enormous pressure, especially in the most affected areas such as northern Italy. This emergency situation has profoundly changed the treatment of paediatric and adult patients with CHD, and our community has been forced to face an unexpected and unknown challenge in terms of the reorganization, relocation of resources and protection from infection for healthcare providers, families and patients. Some programmes, like that in Lombardy, were closed and merged using the hub-and-spoke model [3], whereas others underwent a drastic reduction in activity. At the same time, it was necessary to guarantee adequate health services for those patients, especially newborns and infants, who often require surgery within a narrow time frame [6–8]. In this regard, the priority was to optimize the care of patients with CHD (from foetal to adult age), together with the safety of healthcare providers and our communities. Despite the emotional pressure, tiredness, anxiety and moral distress, the community of Italian congenital cardiac surgeons responded cohesively with innovative and collaborative strategies, which allowed excellent clinical results, thus representing a virtuous model worthy of being implemented in the future.
The pandemic had a heterogeneous spread in Italy, and most of the infections and deaths occurred in the north [9]. This observation is relevant, because the present analysis showed how the pandemic had a differential impact on various Italian paediatric cardiac surgery units in relation to the differential geographical spread of the virus. Our data clearly show that the pandemic represented an emergency mainly in the north of Italy, even though the spread of the disease also differed within different northern regions. Therefore, the most severely affected region, Lombardy, enacted a hub-and-spoke system, shutting down 2 of 3 units, whereas other regions, such as Veneto, Piemonte and Emilia-Romagna, kept all units active, devising dedicated pathways for COVID-free patients. Not surprisingly, the 4 hospitals that remained completely COVID-19 free were in the central and southern regions. Eight centres (57%) had a structural reduction in terms of ICU beds and anaesthesiology/intensive care staff dedicated to CHD, but also in terms of the nursing and the perfusion staff. On the other hand, only 7% of the staff of the paediatric cardiac surgeons were allocated to care of patients with COVID-19.
The patients operated on during the lockdown period (64% urgent and 15% emergency procedures) were mainly neonates or infants who required surgical treatment in the first days or few months of life.
The majority of elective procedures were performed in patients already hospitalized at the beginning of the complete lockdown, in foreign patients who could not be sent home or in patients hospitalized in completely COVID-19 free hospitals. The mortality rate was low (0.5%), demonstrating that the system was able to cope with emergency needs. The activity decreased by 52% compared to the same period of 2019 (51% in the northern, 43% in the central and 66% in the southern regions). The reduction was evident in the northern centres, but it is curious to note how the most drastic reduction in activity occurred in the south where the pandemic had the least effect. We can hypothesize that this phenomenon is due to a greater ‘emotional’ response to the pandemic in relation to lower availability of ICU beds and a lower organization of healthcare in the south compared to the central and northern regions.
There was no COVID-19 congenital cardiac patient operated on in line with the low incidence of coronavirus infection in the paediatric population. Three ACHD patients became infected in the postoperative period. These patients became symptomatic and were transferred to the COVID-19 area where they were treated with medical therapy and recovered completely.
The final section of the questionnaire was dedicated to healthcare providers. The majority of infections among healthcare providers was observed in nurses and to a lesser degree in the anaesthesiology/intensive care physicians. Almost all of the infected staff came from the centres of northern Italy. The contagions occurred in the first 2 weeks of lockdown, and we can only speculate that this could be related to delayed information on prevention and initial inexperience. However, one must be mindful that we had to face an unprecedented challenge that hit us all of a sudden while we were still unprepared.
What could we do better? That is not an easy task to solve even after the experience. Diffuse and systematic swab tests in the entire population should be generalized to all regions to individuate and quickly isolate all viral bursts. One improvement would have been to centralize patients with CHD in just a few CHD centres in order to have COVID-19-free full-time CHD centres, where all surgeons could rotate to take care of patients so that overall activity could have been normal.
The question is now how best to serve our patient community in the second phase (phase 2) of the pandemic and in the future [6, 7]. We should immediately start a return to normality, but we should also start to consider our profession differently and more collaboratively. All great historical revolutions are characterized by profound crises that have pushed those involved to start again with greater strength, achieving even greater results. During the crisis of 1300, which was characterized by the black plague and famine, Italy saw its population halve in a few years. The nation recovered with difficulty and with a profoundly transformed society, which ultimately led to a rebirth, also known as the Renaissance.
CONCLUSIONS
On 11 March 2020, the WHO declared COVID-19 a pandemic. This infectious disease rapidly spread all over the world, impacting dramatically the entire society, the economy and the healthcare systems. In Italy, one of the most severely affected countries, the CHD community has been forced to face a sudden, previously unknown challenge. The pandemic impacted various Italian cardiac surgery units differently, depending on the differential geographical spread of the virus. Two months after the introduction of the complete lockdown, we can estimate that the system was able to satisfy all emergency needs with good results.
SUPPLEMENTARY MATERIAL
Supplementary material is available at EJCTS online.
Conflict of interest: none declared.
Author contributions
Alessandro Giamberti: Conceptualization; Data curation; Formal analysis; Methodology; Project administration; Supervision; Validation; Writing—original draft. Alessandro Varrica: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Validation; Writing—original draft. Salvatore Agati: Data curation; Resources; Validation. Gaetano Gargiulo: Data curation; Resources; Validation. Giovanni Battista Luciani: Conceptualization; Data curation; Resources; Validation; Writing—original draft. Stefano Maria Marianeschi: Data curation; Resources; Validation. Carlo Pace Napoleone: Data curation; Resources; Validation. Guido Oppido: Data curation; Resources; Validation. Massimo Padalino: Data curation; Resources; Validation. Gaetano Palma: Data curation; Resources; Validation. Vitali Pak: Data curation; Resources; Validation. Luigi Arcieri: Data curation; Resources; Validation. Gabriele Scalzo: Data curation; Resources; Validation. Federico Brunelli: Data curation; Resources; Validation. Lorenzo Galletti: Conceptualization; Data curation; Resources; Validation; Writing—original draft.
Reviewer information
European Journal of Cardio-Thoracic Surgery thanks Emre Belli, Mark Hazekamp and the other, anonymous reviewer(s) for their contribution to the peer review process of this article.
Supplementary Material
Abbreviations
- ACHD
Adults with CHD
- CHD
Congenital heart disease
- COVID-19
Coronavirus disease 2019
- ECMO
Extracorporeal membrane oxygenation
- ICU
Intensive care unit
REFERENCES
- 1. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Decree of the Italian PM of March 8, 2020.
- 3.Lombardy Regional Council Ordinance (DRG) n°XI/2906. Seduta del 08/03/2020.
- 4. Elrod JK, Fortenberry JL. The Hub-and-spoke organization design revisited: a lifeline for rural hospitals. BMC Health Serv Res 2017;17:795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Elrod JK, Fortenberry JL. The Hub-and-spoke organization design: an avenue for serving patients well. BMC Health Serv Res 2017;17:475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brida M, Chessa M, Gu H, Gatzoulis MA. The globe on the spotlight: coronavirus disease 2019 (COVID-19). Int J Cardiol 2020;310:170–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Morray BH, Gordon BM, Crystal MA, Goldstein BH, Qureshi AM, Torres AJ et al. Resource allocation and decision making for pediatric and congenital cardiac catheterization during the novel coronavirus SARS-CoV-2 (COVID-19) pandemic: a US multi-institutional perspective. J Invasive Cardiol 2020;32:E103–9. [PubMed] [Google Scholar]
- 8. Stephens EH, Dearani JA, Guleserian KJ, Overman DM, Tweddell JS, Backer CL et al. COVID-19: crisis management in congenital heart surgery. Ann Thorac Surg 2020;110:701–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Civil Protection Department. Coronavirus Emergency: the National response. http://www.protezionecivile.gov.it/risk-activities/health-risk/emergencies/coronavirus (April 2020, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.