Abstract
Background:
Different surgical procedures have been proposed for the treatment of Distal Radioulnar Joint (DRUJ) arthrosis and other conditions. This study aimed to introduce a new design of DRUJ prosthesis based on the Sauvé-Kapandji procedure followed by the evaluation of its short-term results. Darrach and Sauvé-Kapandji techniques are two well-known salvage procedures. Various implant designs have been proposed for DRUJ substitution to avoid the disadvantages of these procedures.
Methods:
Before and after the insertion of the intraosseous DRUJ prosthesis in five patients, indices, such as the range of motion, as well as grip and pinch strengths were measured and recorded. Moreover, the patients were asked to complete three questionnaires (i.e., Quick-Disabilities of the Arm, Shoulder and Hand; Visual Analogue Scale-Pain; and Patient-Rated Wrist Evaluation).
Results:
The patients were followed up for 27.6 months. It is worth mentioning that all patients completed the follow-up period with no complication, except for one case who came with dislocation secondary to forearm malunion and proximal forearm impingement. According to the results, there were improvements in all indices, compared to pre- operation.
Conclusion:
The intraosseous distal radioulnar prosthesis can be an alternative option for the replacement of DRUJ.
Key Words: Case series, Distal radioulnar prosthesis, Sauvé-Kapandji procedure
Introduction
The distal radioulnar joint (DRUJ) plays an important role in the axial rotation of the forearm and stability of the wrist (1, 2). Many surgical procedures have been developed to overcome the DRUJ problems, such as arthrosis, deformity, and instability. Darrach, hemiresection interposition, arthroplasty, and Sauvé-Kapandji procedure are the most well-known techniques (3-5). These procedures are effective in decreasing pain and retrieving function, especially in complex post-traumatic problems. However, the instability of proximal bony stump and its impingement on the radius bone in Darrach and Sauvé-Kapandji procedures (6-10) along with the convergence of the distal ulnar stump in resection arthroplasty techniques (11) are frequent complications of these arthroplasties.
The alternative treatment for traditional reconstructive techniques is arthroplasty implants. In short- and long-term follow-ups, the DRUJ implants decrease complications, such as articular instabilities and bone impingement (12, 13). Moreover, they provide a more normal transfer of forces in the wrist area (12, 14). Nonetheless, a more extended follow-up is needed for such prosthesis to confirm the result sustainability.
Although various designs have been proposed for DRUJ prostheses, they can be classified into two general categories. These categories include prostheses that only have the ulnar component (UHP, Martin GMBH, Germany and U-Head, Small Bone Innovation, USA) and those that, in addition to the ulnar component which replaces the sigmoid notch include the radial component (Aptis DRUJ Prostheses, Aptis Medical, USA and the prosthesis designed by Schuurman AH) (15).
Previously, our team designed an “intraosseous” DRUJ prosthesis and tested its stability and effect on the biomechanics of the wrist. The “intraosseous” DRUJ prosthesis is placed in ulna bone, and DRUJ arthrodesis is performed similarly to the Sauvé-Kapandji procedure. Moreover, forearm axial rotations are carried out through pseudoarthrosis of the ulna bone with a prosthesis instead of DRUJ.
After a cadaver study on “intraosseous” DRUJ prosthesis, as the next step, it was aimed to test the prosthesis on a limited number of patients in order to evaluate its clinical possibility and outcome.
Materials and Methods
In a case-series study, the patients with distal radioulnar joint degenerative changes or instability underwent surgery for the insertion of a newly-designed “intraosseous” prosthesis of DRUJ between 2016 and 2019. The study protocol was approved in the local institutional review board, and informed consent was obtained from all patients before enrollment in the study.
All patients were adults with severe distal radioulnar joint degenerative changes. The exclusion criteria were the patients with severe degenerative changes in carpometacarpal joint or any significant degeneration in the triangular fibrocartilage complex (TFCC).
Anteroposterior and lateral radiographs, as well as three dimensional computed tomography (CT) scans, were obtained before the operation. Moreover, demographic characteristics, range of motion in six directions (i.e., flexion, extension, ulnar deviation, radial deviation, supination, and pronation), as well as grip and pinch strengths were recorded in this study. In addition, the participants were asked to complete three functional questionnaires (i.e., visual analog scale-Pain [VAS], Quick- Disabilities of the Arm, Shoulder and Hand [DASH], and Patient-Rated Wrist Evaluation (PRWE]). The patients were followed up for at least two years after the prosthesis insertion. The range of motion, as well as grip and pinch strengths were measured, wrist and forearm radiographs (anteroposterior and lateral views) were taken, and functional questionnaires were completed at the final follow-up visit.
Intraosseous Prosthesis of the DRUJ
The intraosseous prosthesis of the DRUJ is composed of three main segments, namely distal and proximal stems, locking system, and a globe [Figure 1].
Figure 1.
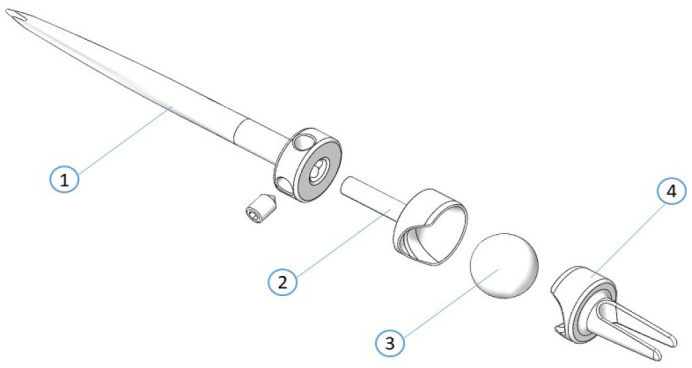
Intraosseous DRUJ prosthesis components: 1- Proximal stem, 2- Locking segment including a proximal concave unit, 3- Globe, and 4- Distal stem including a distal concave unit
Proximal stem
The proximal stem is placed inside the medulla of the proximal segment of the ulna after segmental resection of the bone and designed in two sizes (i.e., 4.5 and 6 mm in diameter) [Figure 1]. In the distal side of the proximal stem, four holes are designed to be connected to the locking system [Figure 1].
Distal stem
The distal stem is composed of two parts, namely an intraosseous section and a head that are used to connect with the globe and the locking segment [Figure 1]. The head is designed in the same way as the head of the locking segment. The intraosseous part of the distal stem has a longitudinal slit allowing the screws to pass through distal ulna to distal radius.
Locking System
The locking system consists of two concave units (head of the distal stem and locking segment). After placing the two units of the locking system together, these two hollow hemispheres form a complete hollow sphere which is the place for insertion of the globe. Each concave unit has a notch in the peripheral border allowing the globe to be inserted while both notches are against each other. After rotating the locking segment (180º), the globe will be safely stabilized.
Globe
Globe is the part of a prosthesis that is placed in the vacant space created in the locking system. In addition to distal and proximal motions, rotations are possibly around it [Figure 1].
Placement of the DRUJ prosthesis (Technique)
In a supine position and under tourniquet control, after prepping and draping, a dorsoulnar incision was made on the ulnar side of distal forearm carving over the ulnar head on the dorsal side [Figure 2A]. The extensor digiti minimi (EDM) and extensor carpi ulnaris (ECU) tendons flap ulnarward were left aside after opening the fifth extensor compartment and subperiosteally releasing of the sixth extensor compartment. It was attempted not to open the ECU compartment. After the DRUJ and ulna bone exposure, the remaining joint cartilage was decorticated and removed with a burr and narrow rongeur, and the DRUJ was prepared for arthrodesis. Similar to the cadaver study, using a specifically-designed jig, the location of the distal and proximal screws for the DRUJ arthrodesis and the distal ulna bone-cuts were determined followed by the resection of the segment [Figure 2 B].
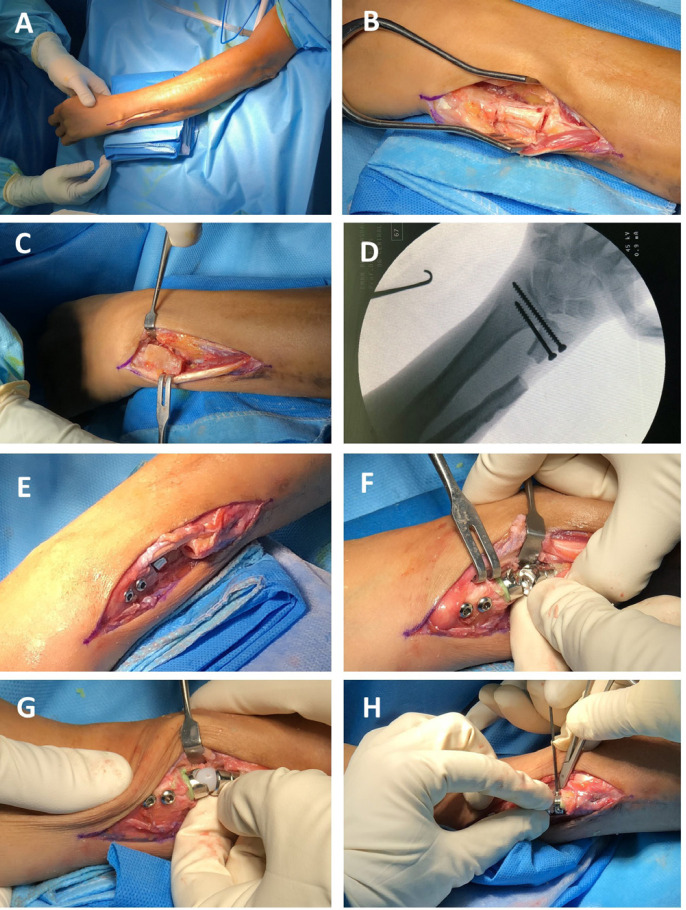
Figure 2A-H.
Intraosseous DRUJ prosthesis insertion technique
(A) A curvilinear incision was made on the ulnar side of the distal forearm extending over DRUJ on dorsal side.
(B) A length of approximately 24 mm was cut from the distal ulna surface, and 20 mm was cut from the distal ulna.
(C) The osteophytes were removed and the remaining joint cartilage was destroyed.
(D) Arthrodesis of the DRUJ is performed using a fully-threaded cancellous screw in the distal and a partially-threaded cancellous screw in the proximal side.
(E) Distal stem is inserted.
(F) The proximal stem and the locking part are inserted.
(G) The globe is placed between the two pieces of the locking system.
(H) These two pieces were rotated 180-degree relative to each other for the final locking of the prosthesis, and the locking part was fixed to the proximal stem using the screws designed in the prosthesis.
If there existed any mismatch between the articular surface of the distal radius and ulna, it would have been leveled out at the time, and arthrodesis of the joint was performed similarly to the cadaver study [Figure 2C; 2D].
Afterward, the medullary canals were reamed, and an appropriate stem size was selected based on the internal diameter (4.5 or 6 mm). After testing the prosthesis stability with trails, the distal and proximal stems were inserted and fixed using cement [Figure 2E; 2F]. Subsequently, the locking part was connected to the proximal stem. The insertion punch was used for the insertion of the globe between the two pieces of the locking system [Figure 2G]. As for the final locking of the prosthesis, the locking part was rotated 180 degrees relative to the distal stem, and the it was fixed to the proximal stem with screws [Figure 2H].
Once the prosthesis insertion process was completed, its stability was checked clinically and under fluoroscopic imaging. By mercerizing the resected ulnar segment around DRUJ, the defects were filled, thereby promoting the DRUJ union. The EDM compartment was closed and the ECU tendon was placed on its anatomic position. The skin and subcutaneous tissues were closed in layers, and after dressing, arm and forearm were secured; moreover, wrist and elbow were put into a long arm splint in a neutral position.
Dressings were changed once a week, and the skin sutures were removed 14 days after surgery. The splint would be removed in week four. Protected active wrist and elbow range of motions started closely after the splint removal. In week 8 and after confirmation of DRUJ union in radiographs, the patient could start an unprotected range of motion.
Tools and Variables
Quick DASH questionnaire
Quick-DASH is a short form of the DASH questionnaire consisting of 11 physical and mental items that measure the upper extremity disability. The scoring is based on a five-point Likert type scale ranging from no difficulty (0) to inability to do the task (100) (16). It should be noted that this questionnaire is validated in Persian (17).
Patient-rated wrist evaluation questionnaire
The PRWE is one of the most common clinical instruments used as an outcome measurement tool for distal radius fractures and other upper extremity conditions. The PRWE questionnaire consists of 15 items to evaluate pain (n=5), as well as hand and wrist functions (n=15) (18). The PRWE score ranges from 0 to 100, and a higher score implies a higher degree of pain and disability. The validity of the Persian version of the questionnaire is confirmed in this study (19).
Visual Analogue Scale
The VAS is a single-item questionnaire ranging from 0 (no pain) to 10 (the highest amount of pain a patient can experience) at the time of visit, which demonstrates pain severity (20).
Grip strength
It evaluates the upper extremities strength using a specific measuring tool (21). The hydraulic grip dynamometer (Lafayette Instrument Company, Indiana, USA) was utilized to measure the hand force in this study. A maximum of three attempts was employed, and the result was reported as the proportion of the affected hand force to the unaffected one.
Wrist range of motion
Regarding the range of motion, the wrist flexion-extension, ulnar-radial deviations, and forearm pronation-supination were measured with an orthopedics ruler in degrees for both sides (22).
Results
In total, five patients (four males and one female) with the mean age of 48.8 years and a mean follow-up of 27.6 months underwent surgery for intraosseous DRUJ replacement [Table 1]. Table 1 tabulates the data before and after DRUJ replacement.
Table 1.
Demographic characteristics of the patients who underwent Intra-Osseous Distal Radioulnar Joint replacement
| Variable | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Mean (SD) |
|---|---|---|---|---|---|---|
| Gender | Male | Male | Male | Female | Male | |
| Age | 32 | 26 | 75 | 65 | 46 | 48.8 (20.9) |
| Duration of symptoms (years) | 10 | 15 | 12 | 2 | 7 | 9.2 (4.9) |
| Follow-up duration (months) | 31 | 29 | 29 | 26 | 23 | 27.6 (3.1) |
| Affected hand | Left | Right | Left | Right | Right | |
| Grip Strength (affected side/unaffected side) | ||||||
| Before surgery | 15.5/34 | 20/42 | 5/20 | 13/29 | 14.5/36 | 40.6 (09.1) |
| After Surgery | 19.5/31 | 36/45 | 13/21 | 18/29 | 19.3/31 | 65.8 (07.9) |
| Pinch Strength (affected side/unaffected side) | ||||||
| Before surgery | 2.4/4.5 | 3.5/9 | 2.5/5 | 2.8/4.2 | 3.1/6 | 52.6 (09.9) |
| After Surgery | 3.2/4.1 | 5.4/8.8 | 3.4/5 | 3.1/4.1 | 4.6/7.1 | 69.6 (07.0) |
| Flexion (affected side/unaffected side) | ||||||
| Before surgery | 40/90 | 70/85 | 50/65 | 50/65 | 70/80 | 73.6 (16.8) |
| After Surgery | 45/90 | 70/85 | 53/65 | 45/65 | 70/80 | 74.1 (15.1) |
| Extesion (affected side/unaffected side) | ||||||
| Before surgery | 60/70 | 80/80 | 60/75 | 60/60 | 75/75 | 93.1 (9.6) |
| After Surgery | 65/70 | 65/80 | 60/75 | 60/60 | 65/75 | 88.1 (8.3) |
| Supination (affected side/unaffected side) | ||||||
| Before surgery | 40/80 | 70/85 | 50/90 | 10/80 | 60/90 | 53.6 (25.9) |
| After Surgery | 65/80 | 70/85 | 65/90 | 45/80 | 60/90 | 71.7 (10.8) |
| Pronation (affected side/unaffected side) | ||||||
| Before surgery | 60/90 | 35/90 | 80/90 | 60/90 | 65/90 | 66.7 (18.0) |
| After Surgery | 80/90 | 65/90 | 80/90 | 70/90 | 70/90 | 81.1 (7.5) |
| Radial Deviation (affected side/unaffected side) | ||||||
| Before surgery | 20/20 | 30/30 | 10/35 | 20/20 | 20/35 | 81.7 (30.9) |
| After Surgery | 20/20 | 20/30 | 12/35 | 20/20 | 18/25 | 74.6 (27.3) |
| Ulnar Deviation (affected side/unaffected side) | ||||||
| Before surgery | 15/40 | 45/40 | 15/35 | 10/25 | 30/35 | 63.7 (33.7) |
| After Surgery | 30/40 | 35/40 | 25/35 | 20/25 | 30/35 | 79.9 (6.8) |
| Range of Motion (affected side/unaffected side) | ||||||
| Before surgery | 60.26 | 80.49 | 67.95 | 61.76 | 81.01 | 70.3 (9.9) |
| After Surgery | 78.21 | 79.27 | 75.64 | 76.47 | 79.24 | 77.8 (1.6) |
| Visual Analogue Scale-Pain | ||||||
| Before surgery | 9 | 6 | 5 | 4.5 | 6 | 6.1 (1.7) |
| After Surgery | 5 | 2 | 1 | 1 | 3 | 2.4 (1.7) |
| Quick-Disabilities of the Arm, Shoulder and Hand | ||||||
| Before surgery | 90.9 | 36.36 | 68.1 | 43.13 | 52.2 | 58.1 (21.8) |
| After Surgery | 52.3 | 11.4 | 18.2 | 4.6 | 18.2 | 52.3 (20.9) |
| Patient-Rated Wrist Evaluation | ||||||
| Before surgery | 51.3 | 62.9 | 86.2 | 53.6 | 65.3 | 63.8 (13.8) |
| After Surgery | 37.3 | 27 | 32.7 | 6.9 | 23.3 | 37.3 (25.4) |
Out of five patients, four cases completed the follow-up period with no complications [Figure 3]. However, patient number one faced prosthesis dislocation two weeks after the operation. Moreover, this patient had a malunion of both bones before undergoing DRUJ arthrodesis. Therefore, the intraosseous space was narrow, and the bones were impinging on each other. Accordingly, it had been ignored by the last surgeon. After the insertion of the prosthesis, his forearm had a small range of rotation secondary to mid-shaft bony impingement. To overcome the problem, the arthrodesis alignment had to be diverged which probably led to prosthesis instability. The prosthesis had to be removed so that it could function as a classic Sauvé-Kapandji procedure [Figure 4].
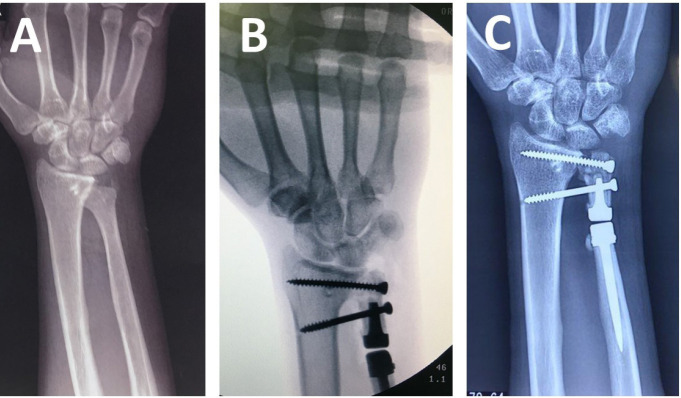
Figure 3A-C.
Radiographs of patient number two
(A) Before the operation, the patient had DRUJ instability (the reconstruction operation had failed 15 years ago).
(B) Fluoroscopic imaging during operation.
(C) Radiograph of the wrist 29 months later.
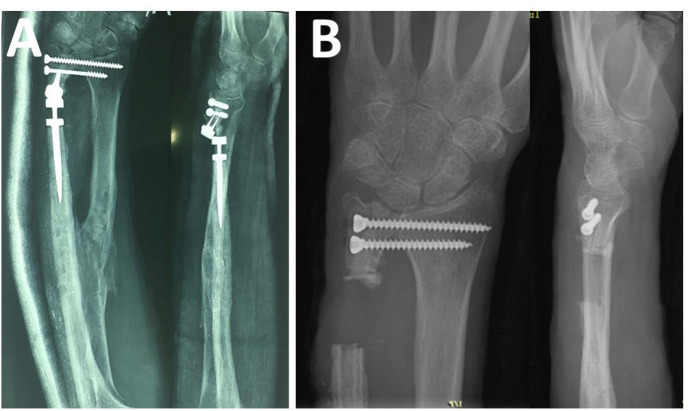
Figure 4A-B.
Patient number one
(A) The prosthesis was dislocated two weeks after its insertion
(B) The prosthesis is removed so that it became a classic Sauvé-Kapandji procedure.
Discussion
The first solution for DRUJ arthrosis was resection arthroplasties. Although these procedures are effective in decreasing pain and retrieving function, especially in complex post-traumatic problems, frequent complications, such as wrist and forearm instability, pain, and functional impairment persuaded surgeons to opt for newer solutions (2, 7, 10). Therefore, various implant arthroplasty techniques for DRUJ arthrosis were developed, and many studies supported the good results with prosthesis arthroplasties (12, 23, 24). In the present study, a newly-designed DRUJ prosthesis was introduced with its insertion technique that was named “intraosseous” DRUJ prosthesis.
Theoretically, this kind of prosthesis has three advantages. First, unlike other types, TFCC is reserved in our prosthesis and the anatomy of the lunocarpal joint remains intact. Second, due to the variety of sigmoid notch anatomy in different individuals, sigmoid notch erosion and instability of DRUJ are common problems in implant prostheses (25); however, in “intraosseous” DRUJ prosthesis, the DRUJ undergoes arthrodesis and no erosion will take place. Finally, if prosthesis failure happens, the surgeon can remove it and convert the surgery to the Sauvé-Kapandji procedure.
The Sauvé-Kapandji procedure is a well-known technique in the treatment of DRUJ arthrodesis (5). In this technique, pseudoarthrosis is made in the distal ulna, and the DRUJ goes for arthrodesis (5). Despite the high rate of success, the convergence of proximal stump in the Sauvé-Kapandji technique and its impingement on radius bone are among the most important complications of this procedure (9-11). It is claimed that our prosthesis is a modification of the Sauvé-Kapandji procedure which uses an implant to stabilize the proximal stump instead of the tendon tenodesis.
The DRUJ prostheses can be categorized into two groups of simple in which the ulnar component is replaced and multi-component in which sigmoid notch of radius is replaced in addition to the ulna head (15). Herbert UHP® (UHP, Martin GMBH, Germany) and uHead (U-Head, Small Bone Innovation, USA) prostheses are two samples of simple prostheses. Furthermore, favorable results are reported in short- and long-term follow-ups. Bone resorption in the distal ulna created by collar stress shielding of the prosthesis as well as sigmoid notch remodeling with prosthesis head were observed in most patients (13, 26). In uHead prostheses, two cases of stem loosening and one case of prosthesis instability were reported as complications (27).
One of the most well-known versions of multi-component prostheses is Aptis DRUJ prosthesis (Aptis Medical, USA). In med-term follow-ups, it demonstrated acceptable survival and function (28); however, one disadvantage of the Aptis prosthesis is complete resection of distal ulna and high amount of soft detachment which plays a significant role in forearm stability (25). As a systematic review reported, secondary surgery was more common in the Aptis prosthesis than other types (21%), mostly for ECU tendon tenosynovitis and stimulation of superficial radial nerve (29).
Regarding the limitations of the study, one can name its pilot nature and the limited number of patients (n=5). Moreover, the follow-up period was only about two years; therefore, it was impossible to make judgments about the durability of the prosthesis and its potential long-term complications. Future studies are recommended to be conducted with longer follow-up periods to investigate the efficiency of “intraosseous” DRUJ prosthesis.
In this study, a different design was proposed for the DRUJ prosthesis which was named “intraosseous” DRUJ prosthesis. Moreover, this study introduced the prosthesis insetion technique. The outstanding feature of this kind of prosthesis is that the index prosthesis works as a pseudoarthrosis not a real joint. Furthermore, the main advantage of “intraosseous” DRUJ prosthesis is that the distal ulna segment is not resected, and ulna styloid connections, ulnocarpal, and TFCC ligaments are reserved. Moreover, if any problem occurs during the prosthesis insertion process, it can be easily converted to the conventional Sauvé-Kapandji procedure. On the one hand, it is hard to judge the efficiency of this prosthesis given the limited number of patients and a short period of follow-ups. Nonetheless, the results reveal that this prosthesis can be considered as an alternative. Further studies with more patients are required for a better evaluation of “intraosseous” DRUJ prosthesis.
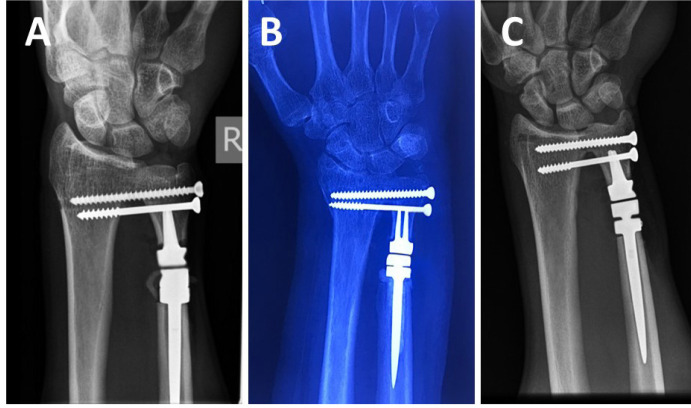
Figure 5.
Patients 3 to 5; Final follow up AP radiographs
Authors’ Contribution:
A.M, M.D. and M.h.E, M.D. are the designers of the prosthesis and involved in the prosthesis U.S. and Iran Patent.
Conflict of Interests:
The authors confirm that there is no known conflict of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Funding:
One or more of the authors (A.M, M.D. and M.h.E, M.D.) has received funding from Mashhad University of Medical Sciences, mashad, iran, as a grant to conduct this study. The other authors received no financial support for the research, authorship, and/or publication of this article.
Ethical Consideration:
Informed consent was obtained from all participants included in the study.
We also Thank clinical research development unit, Ghaem Hosptal, Mashhad University of Medical Sciences for their assistance in this manuscript
References
- 1.Berger RA, Cooney WP. Use of an ulnar head endoprosthesis for treatment of an unstable distal ulnar resection: review of mechanics, indications, and surgical technique. Hand clinics. 2005;21(4):603–20. doi: 10.1016/j.hcl.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 2.Bell MJ, Hill RJ, McMurtry RY. Ulnar impingement syndrome. The Journal of bone and joint surgery. 1985;67(1):126–9. doi: 10.1302/0301-620X.67B1.3968131. [DOI] [PubMed] [Google Scholar]
- 3.DARRACH W. Partial Excision of Lower Shaft of Ulna for Deformity Following Colles’s Fracture. Clinical Orthopaedics and Related Research (1976-2007). 1992;275:3–4. [PubMed] [Google Scholar]
- 4.Bowers WH. Distal radioulnar joint arthroplasty: the hemiresection-interposition technique. Journal of Hand Surgery. 1985;10(2):169–78. doi: 10.1016/s0363-5023(85)80100-3. [DOI] [PubMed] [Google Scholar]
- 5.Kapandji IA. The Kapandji-Sauvé operation Its techniques and indications in non-rheumatoid diseases. Annales de chirurgie de la main: organe officiel des societes de chirurgie de la main. 1986;5(3):181–93. doi: 10.1016/s0753-9053(86)80057-6. [DOI] [PubMed] [Google Scholar]
- 6.Field J, Majkowski RJ, Leslie IJ. Poor results of Darrach’s procedure after wrist injuries. The Journal of bone and joint surgery. 1993;75(1):53–7. doi: 10.1302/0301-620X.75B1.8421034. [DOI] [PubMed] [Google Scholar]
- 7.Bieber EJ, Linscheid RL, Dobyns JH, Beckenbaugh RD. Failed distal ulna resections. The Journal of hand surgery. 1988;13(2):193–200. doi: 10.1016/s0363-5023(88)80047-9. [DOI] [PubMed] [Google Scholar]
- 8.Minami A, Iwasaki N, Ishikawa JI, Suenaga N, Yasuda K, Kato H. Treatments of osteoarthritis of the distal radioulnar joint: long-term results of three procedures. Hand Surgery. 2005;10(02n03):243–8. doi: 10.1142/S0218810405002942. [DOI] [PubMed] [Google Scholar]
- 9.Hagert CG. The distal radioulnar joint in relation to the whole forearm. Clinical orthopaedics and related research. 1992(275):56–64. [PubMed] [Google Scholar]
- 10.Lees VC, Scheker LR. The radiological demonstration of dynamic ulnar impingement. Journal of Hand Surgery. 1997;22(4):448–50. [Google Scholar]
- 11.Sanders RA, Frederick HA, Hontas RB. The Sauvé-Kapandji procedure: a salvage operation for the distal radioulnar joint. The Journal of hand surgery. 1991;16(6):1125–9. doi: 10.1016/s0363-5023(10)80078-4. [DOI] [PubMed] [Google Scholar]
- 12.Sauerbier M, Hahn ME, Fujita M, Neale PG, Berglund LJ, Berger RA. Analysis of dynamic distal radioulnar convergence after ulnar head resection and endoprosthesis implantation. The Journal of hand surgery. 2002;27(3):425–34. doi: 10.1053/jhsu.2002.31734. [DOI] [PubMed] [Google Scholar]
- 13.van Schoonhoven J, Fernandez DL, Bowers WH, Herbert TJ. Salvage of failed resection arthroplasties of the distal radioulnar joint using a new ulnar head prosthesis. The Journal of hand surgery. 2000;25(3):438–46. doi: 10.1053/jhsu.2000.6006. [DOI] [PubMed] [Google Scholar]
- 14.Gordon KD, Dunning CE, Johnson JA, King GJ. Kinematics of ulnar head arthroplasty. Journal of hand surgery. 2003;28(6):551–8. doi: 10.1016/s0266-7681(03)00150-5. [DOI] [PubMed] [Google Scholar]
- 15.Schuurman AH, Teunis T. A new total distal radioulnar joint prosthesis: functional outcome. The Journal of hand surgery. 2010;35(10):1614–9. doi: 10.1016/j.jhsa.2010.06.026. [DOI] [PubMed] [Google Scholar]
- 16.Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (Quick DASH): validity and reliability based on responses within the full-length DASH. BMC musculoskeletal disorders. 2006;7(1):44. doi: 10.1186/1471-2474-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ebrahimzadeh MH, Moradi A, Vahedi E, Kachooei AR, Birjandinejad A. Validity and reliability of the Persian version of shortened disabilities of the arm, shoulder and hand questionnaire (quick-DASH) International journal of preventive medicine. 2015:6. doi: 10.4103/2008-7802.160336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.da Silva Rodrigues EK, Fonseca MD, MacDermid JC. Brazilian version of the Patient Rated Wrist Evaluation (PRWE-BR): Cross-cultural adaptation, internal consistency, test-retest reliability and construct validity. Journal of Hand Therapy. 2015;28(1):69–76. doi: 10.1016/j.jht.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 19.Hassankhani GG, Moradi A, Vahedi E, Hoseinian SH, Jahani Z, Rahmani M, et al. Psychometric Properties of the Persian Version of the Patient Rated Wris t Evaluation. Archives of Bone and Joint Surgery. 2017;5(4):243. [PMC free article] [PubMed] [Google Scholar]
- 20.Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain. 1997;72(1-2):95–7. doi: 10.1016/s0304-3959(97)00005-5. [DOI] [PubMed] [Google Scholar]
- 21.contributors W. Grip strength: Wikipedia, The Free Encyclopedia. [; [updated 23 July 2017 09:37 UTC]]. Available from: https://en.wikipedia.org/w/index.php?title=Grip_strength&oldid=791924225.
- 22.SINGH DAP. Normal Wrist Motion. Available from: http://boneandspine.com/normal-wrist-motion/
- 23.Sauerbier M, Fujita M, Hahn ME, Neale PG, Berger RA. The dynamic radioulnar convergence of the Darrach procedure and the ulnar head hemiresection interposition arthroplasty: a biomechanical study. Journal of hand surgery. 2002;27(4):307–16. doi: 10.1054/jhsb.2002.0763. [DOI] [PubMed] [Google Scholar]
- 24.Masaoka S, Longsworth SH, Werner FW, Short WH, Green JK. Biomechanical analysis of two ulnar head prostheses. The Journal of hand surgery. 2002;27(5):845–53. doi: 10.1053/jhsu.2002.34010. [DOI] [PubMed] [Google Scholar]
- 25.Conaway DA, Kuhl TL, Adams BD. Comparison of the native ulnar head and a partial ulnar head resurfacing implant. The Journal of hand surgery. 2009;34(6):1056–62. doi: 10.1016/j.jhsa.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 26.van Schoonhoven J, Mühldorfer-Fodor M, Fernandez DL, Herbert TJ. Salvage of failed resection arthroplasties of the distal radioulnar joint using an ulnar head prosthesis: long-term results. The Journal of hand surgery. 2012;37(7):1372–80. doi: 10.1016/j.jhsa.2012.04.028. [DOI] [PubMed] [Google Scholar]
- 27.Willis AA, Berger RA, Cooney III WP. Arthroplasty of the distal radioulnar joint using a new ulnar head endoprosthesis: preliminary report. The Journal of hand surgery. 2007;32(2):177–89. doi: 10.1016/j.jhsa.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 28.Axelsson P, Sollerman C. Constrained implant arthroplasty as a secondary procedure at the distal radioulnar joint: early outcomes. The Journal of hand surgery. 2013;38(6):1111–8. doi: 10.1016/j.jhsa.2013.03.030. [DOI] [PubMed] [Google Scholar]
- 29.Calcagni M, Giesen T. Distal radioulnar joint arthroplasty with implants: a systematic review. EFORT open reviews. 2016;1(5):191–6. doi: 10.1302/2058-5241.1.160008. [DOI] [PMC free article] [PubMed] [Google Scholar]