Abstract
Pain is an unfortunate consequence of many medical procedures, which in some patients becomes chronic and debilitating. Among the factors affecting medical pain, clinician-patient (C-P) similarity and nonverbal communication are particularly important for pain diagnosis and treatment. Participants (N=66) were randomly assigned to the clinician and patient roles and were grouped into C-P dyads. Clinicians administered painful stimuli to patients as an analogue of a painful medical procedure. We manipulated the perceived C-P similarity of each dyad using groups ostensibly based on shared beliefs and values, and each patient was tested twice: Once with a same group clinician (concordant, CC) and once with a clinician from the other group (discordant, DC). Movement synchrony was calculated as a marker of nonverbal communication. We tested whether movement synchrony mediated the effects of group concordance on patients’ pain and trust in the clinician. Movement synchrony was higher in CC than DC dyads. Higher movement synchrony predicted reduced pain and increased trust in the clinician. Movement synchrony also formally mediated the group concordance effects on pain and trust. These findings increase our understanding of the role of nonverbal C-P communication on pain and related outcomes and suggest that interpersonal synchrony may be associated with better patient outcomes, independent of the specific treatment provided.
Keywords: Medical pain, placebo, therapeutic alliance, clinician-patient communication, trust toward the clinician
Introduction
Pain is a primary reason patients seek medical care and is a feature of a large number of clinical disorders. Pain is also an unfortunate consequence of many medical procedures that can become chronic and debilitating 65,98,99,117. Pain in postoperative and other contexts is associated with poor mental health, disability, and costs in work productivity and family relationships 2,3,7,18,25,51,105,142,145. Prevention and effective relief of acute pain may improve clinical outcomes, avoid clinical complications, save healthcare resources, and improve quality of life 36.
An important, but under-explored, aspect of the biobehavioral context surrounding pain is the interpersonal context, and interactions between clinicians and patients in particular 104. Indeed, clinician-patient (C-P) communication may play a key role in clinical outcomes 8,12,17,21,29,50,54,100,113,153 affecting patients’ satisfaction 43,44,150 and trust in clinicians 87. Moreover, effective C-P communication can improve patients outcomes, providing a partial explanation for the large placebo effects that are sometimes observed in pain 144. For instance, analgesia can be produced by social observation of others showing signs of pain relief 32,33,71 and social touch 57–59.
A large medical literature demonstrates the importance of C-P concordance, i.e., the match in perceived group membership between clinicians and patients. C-P concordance is related to multiple factors, particularly similarity perceived values and shared culture 28. Aspects of C-P discordance — particularly, discordance in race and gender — may negatively affect multiple clinical outcomes 10,15,19,22,26,28,34,60,73,116,126,141,147,149, including pain assessment 103,127 and trust in the clinician 60. In contrast, shared sociocultural group membership (e.g., race, gender, and language) has been reported to increase patient satisfaction and to decrease pain levels 30,40,70,90,92.
C-P concordance may have multiple benefits, but some of the most important include enhancing the therapeutic alliance and trust in the clinician 35,89. The therapeutic alliance is thought to be grounded in the coupling between the clinician’s and patient’s brains, providing access to internal states, which facilitates emotional sharing and common understanding, 20,83,124 which has in turn been associated with pain reduction 6,46,106.
Though they are demonstrably important, the mechanisms underlying C-P communication are understudied, and measures of effective C-P communication are lacking. One important aspect concerns nonverbal behavior, and in particular interpersonal synchrony. A large literature of nonverbal communication demonstrates that eye contact, supportive touch, smiling, nodding, and engaged posture are associated with stronger C-P relationships and improved patients’ health outcomes and satisfaction 44,77,79,84,102,107,123,131.
Movement synchrony is a particularly important aspect of interpersonal synchrony because it both provides a basis for inferred self-similarity and concordance (potentially increasing trust and therapeutic alliance) and can be measured non-invasively in interpersonal interactions.
Humans tend to coordinate their movements and imitate the postures and actions of others 13,109,128. This interpersonal motor (movement) synchrony is easy to interpret and understand because the link between perception and motor action is highly automatic 41,118,151. During C-P interactions, certain nonverbal behaviors such as smiling, nodding, eye contact, and forward trunk lean affect patient’s ratings of the clinician’s interpersonal skills, their relationship quality, and their rapport 23,66,67,130.
In this study, we simulated clinical interactions and manipulated feelings of similarity between participants who played the roles of patients and clinicians (hereafter clinicians and patients) by assigning them to color groups ostensibly based on their shared beliefs and values. Each “patient” (and “clinician” was paired with a “clinician” (and “patient”) in a concordant group and in a discordant group. In Losin et al., 2017, we previously found that patients with concordant clinicians felt more trust and similarity towards their clinician, which in turn predicted lower pain ratings 95. In the current study, we extend this work by investigating the role of motor synchrony between clinicians and patients, calculated from the recorded video of the interaction. We predicted that there would be lower pain ratings when patients were paired with concordant clinicians and that that effect would be mediated by their motor synchrony. We also predicted that higher patient ratings of trust toward the clinician in concordant interactions would be mediated by the motor synchrony between the partners.
Methods
Participants
Eighty individuals (40 male) aged 19 to 54 years old (mean = 26.19, SD = 9.43) were recruited and tested in dyads as reported in Losin et al., 2017 95. Videos of both participants in each dyad were recorded throughout the interaction using tripod-mounted cameras. Due to video recording failures or poor video quality, 14 simulated interactions were excluded from the analysis, resulting in a final sample size of 66 participants (34 male). Participants were in the moderate range in socioeconomic status (SES; mean = 33.55, SD = 12.32, scale from 8 to 66) and reported no current or recent neurological or psychiatric diagnoses. They also reported no use of psychoactive or pain medications, pain-related medical conditions, or unusual pain sensitivity. Participants were recruited through the Sona paid subject pool at the University of Colorado Boulder, which included members of the university and surrounding community. Only subjects from the Sona database who met the inclusion criteria were contacted. The study was approved by the University of Colorado Boulder institutional review board and written informed consent was obtained from all participants.
Measures
Pain rating
At the end of each trial, patients rated the overall pain intensity experienced on a 100-point generalized, labeled magnitude scale using a computer mouse (0 = no experience, 100 = strongest imaginable experience) 9. Intermediate ticks were marked at 1.4 (barely detectable), 6 (weak), 17 (moderate), 35 (strong), and 53 (very strong); only the labels and not the numbers were visible to the patients. The general labels on the scale have been reported to allow for effective comparison of sensory and affective experiences across modalities and people, and the label spacing has been reported to provide the scale with ratio properties 9.
Patient perceptions trust toward the clinician
After each simulated clinical interaction, the patients completed the following questionnaires about their trust toward their clinicians. The trust toward the clinician was measured by a trust visual analog scale (TVAS), a single-item measure that asked participants to rate how much they trusted the clinician (“I trust the green/yellow clinician’) on a scale ranging from 0 (not at all) to 150 (extremely) 95. The patients also completed The Wake Forest Physician Trust Scale 64, a clinically validated 10-item measure that assessed the patient’s perceptions of the clinician’s behavior and the patient’s trust in the clinician 138; patients rated their trust toward the clinicians on a scale from 1 (strongly agree) to 5 (strongly disagree), and the responses were summed with higher values corresponding to more trust 95. We modified the language of the Wake Forest Physician Trust Scale to apply to the medical simulation context. For example, “You have no worries about putting your life in your doctor’s hands” and “You completely trust your doctor’s decisions about which medical treatments are best for you” were modified to read “You completely trust the green/yellow doctor and his/her decisions about how to perform the study procedures.” and “ You have no worries about putting your safety in green doctor’s hands.” Because of the conceptual overlap in The Wake Forest Physician Trust Scale and the TVAS, they were rescaled and averaged to create a single composite measure of patients’ trust toward clinicians on a scale 0 to 150, with higher values reflecting higher levels of trust.
Movement synchrony analysis
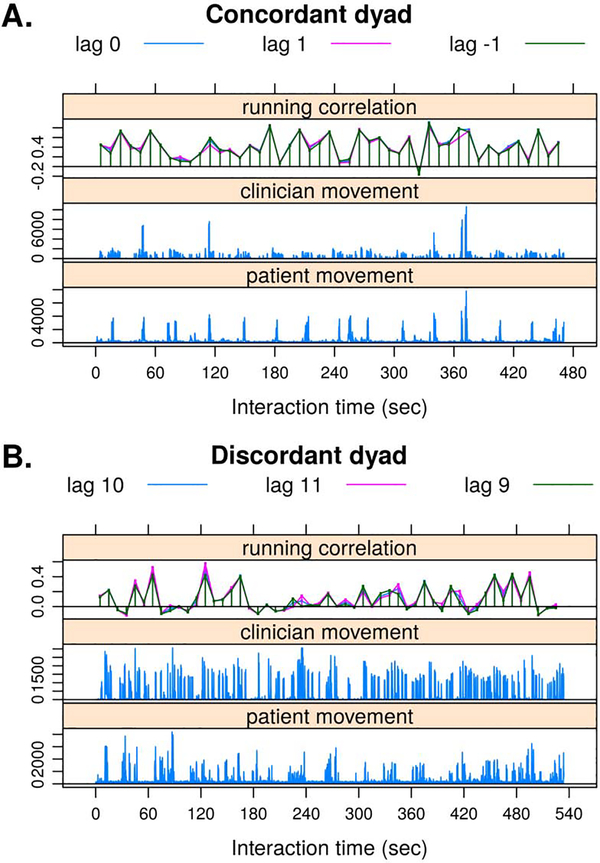
The video was processed by Motion Energy Analysis (MEA) software 120, designed to quantify movement in digital video recordings. Detection of frame-by-frame change allowed an objective quantification of movement occurring in spatially predefined regions of interest (ROIs). The method is based on the fact that each individual frame of a black-to-white scale has a fixed number of pixels that represent a distribution of gray-scale values ranging from 0 (black) to 255 (white). Motion energy is defined as differences in grayscale pixels between consecutive video frames 1,108,115,121. MEA thus generates time series of raw pixel changes within an ROI, and a second-order Butterworth low-pass filter with a cutoff at 2.4 Hz was applied prior to further analyses. Head motion synchrony was used as a marker of interpersonal synchrony based on previous studies using automatic techniques for measuring synchrony in velocity (for review, see 39). Head motion has also been used to analyze nonverbal dyad interactions in psychotherapy 114,120,121. In the current study, the participants’ head movements were tracked via Samsung HMX-QF30 HD (1,280 × 720 60p) video camera. Because the dyads may have differed in the dynamics of their interaction, for each dyad we identified three lags that showed the maximal correlation using 10-second running windows (applying windows of 5 and 15 seconds yielded similar results) and exploring all possible lags within a 5-second lag in each direction. The Fisher Z-transformed values of the maximum cross-correlations were averaged for each C-P interaction. Figure 1 presents the running window cross-correlations of the maximal three lags for a CC dyad (Fig. 1A) and a DC dyad (Fig. 1B). All lags were very close to zero (M=0.63, SD=1.43, min=0, max=11=1/3 sec).
Figure 1.
Example of the movement data and windowed cross-correlations for the 3 lags of the maximum correlation: (A) a CC C-P dyad and (B) a DC C-P dyad. The y-axis represents: 1) the moving window correlation over time (top subplot); 2) the clinician’s and the patient’s movement intensity (middle subplot); 3) and the patient’s movement intensity (bottom subplot),. The x-axis represents the interaction time. The running windows are 300 frames (10 s) of length. The numbers associated with the lag segments (e.g. lag 10) reflect the lagged difference (in # of frames ) between the interacting subjects that maximize the movement synchrony between them. Because the camera frequency is 30 Hz, lag 10 in Figure 1B indicates that the patient mostly led the partner (clinician) in his/her movements for about ⅓ of a second.
Study Design
Group assignment and manipulation check
To manipulate feelings of interpersonal similarity between participants, we created artificial sociocultural (green and yellow) groups on the basis of participants’ core beliefs and values (a modification of the minimal group paradigm) 134. Participants were paired with two different partners one assigned to be of the same group (concordant, CC) and one of a different group (discordant, DC), and underwent a simulated interaction with an opposite role partner, playing the role of clinician and patient (a modification of the minimal group paradigm) 134. We then randomly assigned participants to play doctor or patient roles. Each participant took part in two simulated clinician-patient interactions, one with an interaction partner from the same group (concordant, CC) and one with an interaction partner from a different group (discordant, DC). Participants were recruited and tested in groups of 4, with one doctor and one patient in each color group. Because previous studies have shown an effect of subject-experimenter gender concordance on pain ratings, each group was either all male or all female 4,93.
One week before the main laboratory session, participants completed the Personal Beliefs and Values Questionnaire (PBVQ), with a composite measure that included questions about the following: (1) gender role beliefs and values from the World Values Survey Wave 5 5, (2) religious beliefs and values from the Duke University Religion Index, 80 and (3) politically polarized beliefs and values used in a previous study 96. Participants completed the PBVQ online via Qualtrics (Qualtrics Labs, Inc).
Upon arrival at the lab, all participants reviewed the PBVQ as a reminder of its contents, and the experimenter explained that “We’re going to use your answers to that questionnaire to divide you into 2 groups. For confidentiality reasons, we’re going to use color labels of green and yellow to assign the groups, but you can assume those in your color group have more similar values to yours than those in the other group.” In order to avoid deception, participants were assigned to either the “yellow” or the “green” groups based on the correlations in their PBVQ responses and given group color-coded garments to wear during the session. However, the actual values and beliefs of the participants on a given day varied randomly because participants were not recruited for the study based on this information. Therefore, the group assignment did not systematically affect the degree of belief and value similarity between participants in the same group or result in any consistent association between group identity (green or yellow) and a particular belief or value orientation. Therefore, any consistent effects of the group manipulation were likely caused by the assumption of shared values and beliefs resulting from the group assignment – similar to the effects of real-world shared group membership perceived during brief clinical interactions.
To test efficacy of the group manipulation, participants completed a 3-item Group Identification Questionnaire at the end of the study, modified from the Collective Identification Scale 146 regarding their group membership (e.g., “I am proud to be a member of the green/yellow group”). Participants also responded to three questions designed to assess how realistic participants felt the current study was on a 150-point visual analog scale (0 = no belief to 150 = strongest belief), which we refer to as the Study Belief Index. These questions were: 1. To what degree did you believe the study was about investigating the effects of personal beliefs and values on the clinical interaction?, 2. To what degree did you believe the groups were assigned based on your reported personal values?; and 3. How realistic did the simulated clinical interactions feel to you? Each was rated on a 100 point scale from 0 (not at all) to 100 (completely). Summing these (Cronbach’s alpha=0.88) was meant to provide a rough indication of how much participants believed in the premise of the study and found it realistic, rather than provide a psychometrically validated measure. The participants were told that the study aims to investigate “the effects of people’s personal beliefs and values on their experience when they get medical care.” Responses to the Study Belief Index indicated moderate to strong belief in the stated purpose of the study, the stated basis for group assignment, and the realism of the simulated clinical interactions (patient participants: mean = 75.63, SD = 28.66; clinician participants: mean = 84.46, SD = 28.78).
Clinician and patient assignment and training
Participants were randomly assigned to the role of patient or clinician and provided with clothing to match their role: hospital gowns for patients or white lab coats with scrubs for clinicians (Fig. 2A, 2B). Clinicians practiced the interaction with patients by going through the entire procedure including introducing themselves, describing the procedure, and administering the procedure, on the experimenter training them not on patients. The patients went through the heat familiarization task and practiced making continuous within-trial and overall post-trial pain intensity ratings. Participants were trained in the simulated clinical interaction in groups of two based on their role, not a group assignment. Thus, yellow and green patients, as well as yellow and green clinicians, were trained together (Fig. 2A, 2B).
Figure 2.
The design of the current study. (A) We randomly assigned participants to the role of either patient or clinician (1 in each group/dyad). During each study session, a patient took part in two simulated clinical interactions, one with a clinician from the same color group (CC interaction) and one with a clinician from the other color group (DC interaction), with the interaction order counterbalanced. (B) An example of the recorded clinical simulation. Participants were provided with clothing to match their roles: hospital gowns for patients and white lab coats with scrubs for clinicians. (C) Each clinical interaction included 16 heat trials: a medium heat “washout” stimulus (47.5°C) delivered to each skin site (4 trials) at the beginning of the heat stimulation procedure for the initial habituation of the skin site to contact heat followed by a single trial at each temperature on each of the 4 skin sites (12 trials) in a randomized order.
Clinician and patient in simulated clinical interaction
During each study session, a patient took part in two simulated clinical interactions, one with a clinician from the same color group (concordant interaction) and one with a clinician from the other color group (discordant interaction), with the interaction order counterbalanced across participants. During the session, the experimenter was seated at a table behind and partially out of view of the subjects to track the quality and safety of the heat procedure while maximizing the realism of the simulated clinical interaction.
At the start of the clinical interaction, the clinician introduced himself or herself to the patient, repeating the explanation of the heat stimulation procedure and reminding the patient that it was being applied as an analogue to a painful medical procedure (Fig. 2C). The clinician also reminded the patient that the thermal stimulation could be stopped at any point if the pain became intolerable. The clinician was also allowed to engage in conversation on any other topic to establish rapport with the patient throughout the interaction. Afterwards, the clinician applied the thermal stimulation to the patient.
Thermal stimulation was applied using a script programmed in E-Prime stimulus presentation software (E-Prime 2.0; Psychology Software Tools, Inc, Pittsburgh, PA). Thermal stimulation was delivered to 4 evenly spaced locations on the volar surface of the left forearm of the patient at 3 target temperatures (46.5°C, 47.5°C, and 48.5°C) using a 16×16 mm contact Peltier thermode (Medoc, Inc, Ramat Yishai, Israel). All heat stimuli were 11 seconds in duration, consisting of 7.3 seconds at the target temperature, and 1.85-second ramp periods to get to/from the target temperature from/to the 32°C baseline temperature. Each trial was preceded by the clinician asking the patient if they were ready and the trials were separated by variable delays. Fig. 2C provides a more detailed explanation of the trial and task structure. Each clinical interaction included 16 heat trials: a medium heat “washout” stimulus (47.5°C) delivered to each skin site (4 trials) at the beginning of the heat stimulation procedure for the initial habituation of the skin site to contact heat followed by a single trial at each temperature on each of the 4 skin sites (12 trials) in a randomized order 62,74. The clinician intermittently reminded the patient throughout the procedure that he/she may terminate the heat stimulation at any time if the pain became intolerable or for any other reason.
Statistical analysis
We applied the multilevel modeling (MLM) framework for the hypothesis testing and assumed random intercepts for patients and clinicians to treat the nested nature of the data with R package lme4. The model allowed taking the dependent structure of the data into account. In our case, we modeled C-P interactions nested in clinicians (2 data points) and patients (2 data points). Using this framework, mediation models were tested using a quasi-Bayesian Monte Carlo method with 5000 simulations and White’s heteroskedasticity-consistent estimator for the covariance matrix 140,155.
To examine a mediation model in which the grouping manipulation predicts changes in movement synchrony, which in turn predicts patient pain rating, we conducted a series of analyses (Fig. 3). The outcome measure for the mediation analysis was the patient pain rating at the end of each trial. Here we applied the following two models as described above: (a) to test the group concordance effect on movement synchrony; and (b) to test the association between movement synchrony and pain ratings, conditioned on the effect of the belief manipulation (group concordance). All the reported model coefficients are unstandardized.
Figure 3.
Proposed mediation model: movement synchrony mediates the effects of group concordance on pain perception and trust toward the clinician.
Finally, the mediation effect was defined as a*b and statistical inferences were made based on the approach described above 140,155. Cohen’s d statistics were provided as estimates of the model effect sizes 31. Robust inferential methods are available that perform well with relatively small sample sizes 125,152. Here we reanalyzed the data using an extension of this approach for linear mixed models 81 based on multivariate MM-estimators via R package robustlmm. Generally, the procedure fits weight for each observation using the Mahalanobis distance, i.e., the tail observations receive less weight. The estimated significance of the model was calculated using a robust Wald test and the mediation effect was tested based on the approach proposed by Zu and Yuan (2010) in which a bootstrap estimation of mediation effect was combined with a robust estimation routine 156.
It is important to emphasize that patients’ pain level was measured after the heat stimuli were terminated, and the video fragments of the ratings were cut from the analysis of motor synchrony because the participants were not engaged in interpersonal interaction during those times. In addition, trust toward the clinician was estimated at the end of each section. Thus, the data used in the mediation models had the appropriate temporal order.
In addition, we initially tested whether patients’ and clinicians’ movement intensities were associated with movement synchrony, patients’ pain rating, and their trust in the clinician. Variables with significant contribution were included in the mediation analysis as control variables.
Results
Manipulation checks and descriptive statistics
Patient participants (mean = 10.62, SD = 3.54) as well as clinician participants (mean = 9.03, SD = 3.97) reported moderate to strong identification with their assigned group (3 = no identification to 18 = strongest identification), confirming the validity of the grouping manipulation. Table 1 presents descriptive statistics of the patients’ pain ratings, trust in their clinicians, and movement synchrony by group concordance.
Table 1.
Descriptive statistics of the variables of interest: Movement synchrony, Patient’s Pain Ratings and Patients’ Trust in the Clinician
| Variables | Discordant | Concordant | Total |
|---|---|---|---|
| Movement synchrony Mean (SD) | 0.148 (0.0779) | 0.219 (0.0752) | 0.182 (0.0840) |
| Pain Ratings Mean (SD) | 50.0 (22.1) | 46.0 (20.8) | 48.0 (21.4) |
| Trust in a clinician Mean (SD) | 83.5 (23.0) | 100 (22.9) | 91.7 (24.3) |
Control variables
The absolute level of movement of the patient and clinician may have been related to their movement synchrony or the patients’ pain perception and trust toward the clinician. For this reason, the association between the movement intensity of both clinicians and patients with movement synchrony, pain ratings and trust was initially tested. Patient movement intensity increased movement synchrony (B=.0005, 95% CI [.0002, .0007], F(1, 55)=12.96, p=0.0007, Cohen’s d=0.48 [0.21, 0.75]), decreased patients’ pain ratings (B=−.034, 95% CI [−.064, −.005], F(1, 33)=5.21, p=0.03, Cohen’s d=0.40 [0.04, 0.75]), enhanced trust toward the clinician (B=.092, 95% CI [.009, .172], F(1, 63)=4.87, p=0.03, Cohen’s d=0.28 [0.03, 0.53]), and therefore, these factors were included as control variables in the subsequent analyses. Clinician movement intensity was not related to patient movement synchrony (B=.0001, 95% CI [−.0001, .0003], F(1, 57)=1.42, p=0.24), pain ratings (B=.015, 95% CI [−.013, .043], F(1, 34)=1.08, p=0.30), or trust toward the clinician (B=.045, 95% CI [−.028, .1109], F(1, 63)=1.45, p=0.23) so it was not included in subsequent analyses.
Mediation analysis
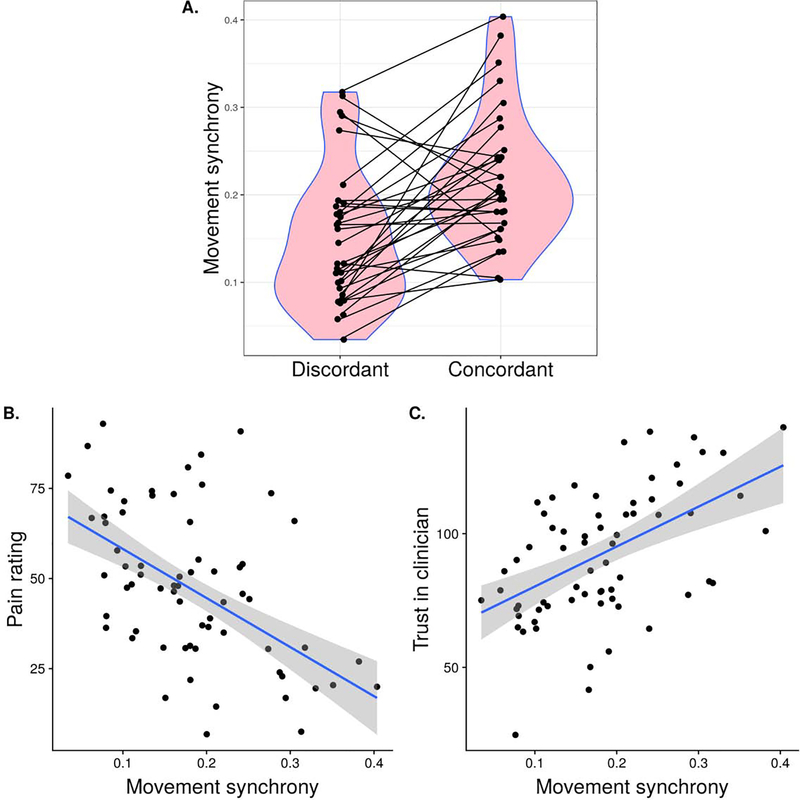
The concordance manipulation did not directly affect patients’ pain ratings (B=−2.45, 95% CI [−5.54, 0.59], F(1, 32)=2.60, p=0.11). However, the concordance manipulation enhanced movement synchrony (Fig. 4A) (B=0.05, 95% CI [0.03 0.08], F(1, 31)=16.06, p=0.0003, Cohen’s d=0.71 [0.34, 1.07]).
Figure 4.
(A) Movement synchrony differences between concordant and discordant dyads, based on the experimental manipulation of their perceived belief similarity (Cohen’s d=0.71). (B) Movement synchrony is negatively associated with patients’ pain ratings (Cohen’s d=0.49). (C) Movement synchrony is positively associated with patients’ trust toward the clinician Cohen’s d=0.45. Model prediction lines with corresponding 95% confidence intervals are presented.
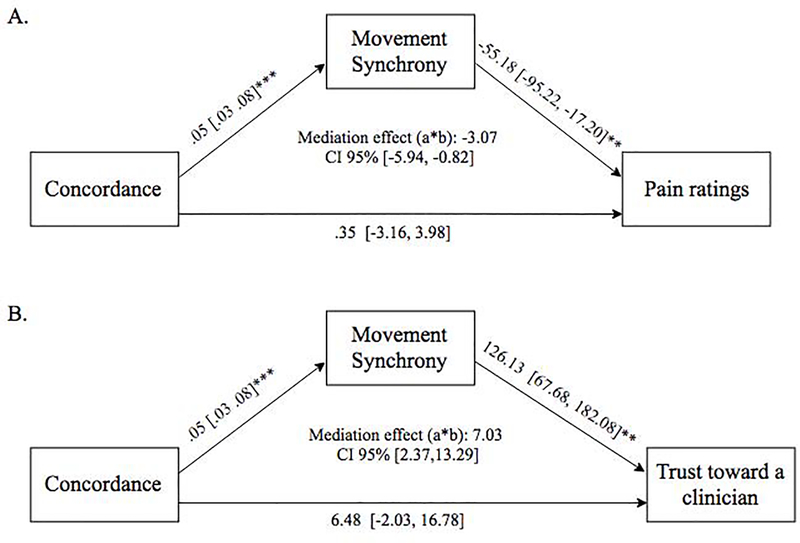
Moreover, adjusting for the concordance manipulation, movement synchrony was associated with decreased patient pain ratings (B=−55.18, 95% CI [−95.22, −17.20], F(1, 35)=8.49, p=0.006, Cohen’s d=0.49 [0.15, 0.84]) (Fig. 4B). This effect remained after controlling for trust in clinicians (B=−60.47, 95% CI [−100.50, −21.07], F(1, 32)=9.12, p=0.005 Cohen’s d=0.53 [0.17, 0.89]). Finally, C-P movement synchrony mediated the effect of C-P concordance on patient pain ratings (indirect=−3.07 [−5.94, −0.82], p=0.005).
For the second mediation model with trust toward the clinician as an outcome, patients in the congruent condition reported an increased level of trust toward the clinician (B=13.59 [4.95, 23.84], F(1, 30) =7.76, p=0.009, Cohen’s d=0.51 [0.14, 0.88]) (Fig. 4C).In addition, movement synchrony was associated with an increase in patients’ trust toward the clinician (B=126.13, 95% CI [67.68, 182.08], F(1, 56)=11.50, p=0.001, Cohen’s d=0.45 [0.18, 0.71]), adjusting for the effect of group concordance. Conditioning on the effect of movement synchrony, the concordance group effect was not significant anymore (B=6.48, 95% CI [−2.03, 16.78], F(1, 36)=1.58, p=0.21). In addition, C-P motor synchrony mediated the group difference in patients’ trust toward the clinician (indirect=7.03 [2.37,13.29], p=0.001) (Fig. 5), suggesting complete mediation of the effect of C-P movement synchrony on the pain rating concordance bias. Finally, we found that both outcomes (patient pain and trust in clinician) are negatively correlated when controlling for patient and clinician movements (B=−0.33, 95% CI [−0.65, −0.06], F(1, 32)=5.40, p=0.03, Cohen’s d=0.41 [0.05, 0.77]), suggesting that the discovered similar mediation patterns for two study outcomes may underlie shared mediation mechanism.
Figure 5.
Mediation model findings for (A) patient pain ratings and (B) patient trust toward the clinician. The numbers in the brackets show 95% confidence intervals for the estimates.
Discussion
In this study, we tested the mediating role of C-P movement synchrony in the patient’s analgesia and trust toward the clinician as a result of perceived similarity with the clinician. Our findings support the hypothesis that group-concordant (CC) dyads demonstrated a higher level of movement synchrony than group-discordant (DC) dyads, which in turn predicted lower pain ratings in patients and greater trust toward the clinician. Mediation analyses showed that movement synchrony was a complete mediator of group concordance effects on perceived pain and trust toward the clinician, meaning that movement synchrony is sufficient to explain the interpersonal context effects on both pain and trust. Trust and pain were also associated, suggesting a link between them, though trust was not sufficient to explain the relationship between movement synchrony and pain.
Despite the best intentions of physicians to provide equal treatment to all, groups that are under-represented in the clinician workforce may experience a mismatch in group identity. Such perceptions may affect multiple patient outcomes 28,34,73 including pain 103,127 and trust toward clinicians 56,60, and thus patient-reported outcomes more broadly. Reduced trust due to low perceived concordance may also have other effects beyond what we tested here, including delays in seeking medical care or filling prescriptions 22,26,147,149, low adherence to physician recommendations 15,19,26, less utilization of some preventive services 26,69,126,141, more missed medical appointments, 15 and substitution of alternative medicine for conventional care 10. Among the mechanisms of poorer patient experiences in discordant C-P interactions is poorer quality communication 35.
These findings increase our understanding of how the biobehavioral context surrounding painful experiences influences pain perception. They fit with a broader literature showing that social, cultural, and contextual factors influence pain perception 37,82,94,132. Contextual factors, including the effects of interpersonal communication, are often categorized as ‘top-down’ effects, as they are driven by how an individual conceives of the context in which pain and other symptoms occur. Especially, movement synchrony in social interaction may be important for a variety of reasons. Humans show a tendency to imitate the postures or actions of others 109,128. This capacity develops early in life 49,91. It plays a key role in the development of infant-mother bonding and in social communication 45,129 and may be an important ingredient of empathy more broadly 11. Previous studies have highlighted the role of interpersonal synchrony in adaptive emotion-regulation 48,55,97,143, including regulation of anxiety and depression 121, touch-induced analgesia 58,59, and joint attention 42. Synchrony may influence trust and pain through several mechanisms. Movement synchrony may enhance receptiveness to clinicians’ suggestions, increase social connection and perceived self-other overlap 97, and reduce anxiety and negative mood, all of which have been linked to pain relief 72,95. Synchrony may have bidirectional effects; mimicking others appears to increase receptivity to others’ preferences, and being mimicked may increase feelings of affiliation 135.
Some research also suggests that movement and kinesthetic cues play a particularly important role in low-level inferences about what external objects or agents should be associated with the self. For example, in patients with phantom pain after limb amputation, seeing and feeling arm movements in synchrony can help patients ‘re-integrate’ the brain representation of a severed limb and reduce phantom pain 27,53. A meta-analysis of these and other manipulations of visual-kinesthetic ‘body illusions’ showed large therapeutic effects 16. Beyond the pain context, research has suggested that joint movement or movement synchrony is important for ‘kinesthetic empathy’ 11, which relates to awareness of the dynamic interactions between self and other, i.e., movement sensations in response to someone else’s body movements or postures 11,47 that enable a response to the other’s emotional state 139,154. Moreover, oxytocin, a hormone that is reported to encourage social bonding, has also been reported to enhance movement synchrony 75. Based on this evidence, movement synchrony might serve to increase low-level (and perhaps unconscious) inferences of self-relatedness, accompanied by enhanced positive affect and conscious feelings of affiliation and trust, accompanied by potentially enhanced oxytocin levels. These relationships remain to be tested more completely in future studies. In addition, because it can be readily measured from interpersonal interactions, movement synchrony may be useful as a behavioral marker for effective interactions 133,136,137. Currently, there is a large initiative to develop measures related to pain and its biological correlates (biomarkers) 61,76,78,110,122, including behavioral measures, but measures of interpersonal communication are still lacking.
Indeed, in the United States, about 50% of all patients leave an office visit without an adequate understanding of what the clinician has told them 101. Interpersonal movement synchrony could be used as a marker of the C-P communication quality. It is easier to interpret and understand (as compared to physiological synchrony) because the link between perception and motor action is highly automatic 41,118,151. Thus, the motor activity provides a continuous stream of behavior that can be spontaneously and effortlessly synchronized, even when a person’s conscious attention is directed elsewhere 111,148. Moreover, our tendency to automatically mimic and synchronize movements with others has been suggested to result in emotional contagion 85,112, to affect social behavior 85,86 and to play a key role in the development of empathy 119. Indeed, during C-P interactions, certain nonverbal behaviors such as smiling, nodding, eye contact, and forward trunk lean affect patient’s ratings of the clinician’s interpersonal skills, their relationship quality, and their rapport 23,66,67,130. Since movement-based cues can strengthen C-P relationship and improve patients’ health outcomes and satisfaction 44,77,79,84,102,107,123,131 biomarker of the clinical interaction quality, especially because it could be measured in a simple way using just a video camera. In clinical settings, practicing active listening can increase C-P movement synchrony, possibly by blurring the boundaries with the patient and increases the feeling of similarity 68.
Increased C-P movement synchrony could be a valuable addition to interventions, and may improve the C-P relationship. However, future studies should further investigate the mechanisms of movement synchrony dynamics. For example, we should strive to better understand the synchrony’s onsets and offsets, the factors that drive the synchrony (e.g. empathy), as well as the nature of the movement synchrony affecting health outcomes. Such research may result in the development of Artificial Intelligence that will help clinicians to establish safe and efficient communication with their patients.
Because our findings bear on the perceived similarity of group membership between clinicians and patients, they also bear on issues of ethnic and racial disparities in health care. Discordance between a patient and a clinician may affect both parties. The nature of the discordance is most likely implicit 38,52,103, but may be reflected in body movements during the communication between patients and healthcare providers, i.e., through kinesthetic cues. Assessing movement synchrony and related interpersonal variables may thus be a productive way of understanding and improving the quality of care in clinical settings.
These results should be interpreted in light of several limitations that need to be acknowledged. The use of artificial sociocultural groups allows for random assignment of individuals to groups, and thus assessments of causal effects of C-P concordance. This also potentially enhances the generalizability of our findings to a variety of groups. However, it is still unclear how the concordance effects we observed here will generalize to those of real-world sociocultural groups in clinical settings. We expect variation across groups related to the particular groups and cultures studied. Future studies should increase the ecological validity (realism) of the simulated clinical interactions, including studies with actual clinicians and patients in a hospital or other clinical settings. Likewise, our use of experimentally evoked pain provided a controlled stimulus that can be randomized and causal effects inferred; but clinical pain has distinct characteristics that are likely to vary across pain conditions and patient populations. The value of this study lies in demonstrating causal effects in a controlled setting, complementing ecological studies of clinical interactions ‘in the wild’. In addition, we calculated C-P synchrony based on head movements. However, C-P synchrony may be reflected in multiple types of data. Head movement data are interesting in part because they can be easily obtained from video camera data and can thus be easily deployed in clinical and research settings. Future studies should address this point by capturing C-P synchrony in whole-body movements, neurophysiological signals, and voice. Also, we recognize that artificial synchrony is complex—for example, if participants realize they are being mimicked then the effects could be substantially altered—and that the parameters that govern optimal synchronization in dyadic settings require further research 63. Finally, we did not try to infer a causal relationship between pain sensitivity and trust in the clinician. This causality may be complex; for example, movement synchrony may affect pain sensitivity, which in turn modulates trust in the clinician. Indeed, it has been reported that high (vs. low) movement synchrony affects trust and interpersonal liking during the Trust Game paradigm by modulating pain sensitivity 88.
In conclusion, these findings increase our understanding of the role that nonverbal C-P interactions may play in pain perception and pain-related outcomes and the mechanisms that may underlie this relationship. The findings suggest interpersonal movement synchrony as a measurable mechanism that underlies the effect of clinician-patient similarity on patients’ trust in clinicians and pain experienced during medical care. In addition, these findings contribute to a growing literature demonstrating improved patient outcomes through placebo effects based on improving C-P communication 14,24. Supporting clinicians in finding commonalities with their patients and enhancing positive nonverbal communication could improve patient outcomes and patient satisfaction, whatever the specific treatment provided.
Highlights.
Clinician-patient movement synchrony higher in sociocultural group concordant dyads
Higher clinician-patient movement synchrony predicts reductions in patients’ pain
Higher clinician-patient movement synchrony predicts increased trust in clinician
Clinician-patient movement synchrony mediates concordance effects on patients’ pain
Clinician-patient synchrony mediates concordance effects on trust in clinician
Perspective.
This article demonstrates that movement synchrony in clinician-patient interactions is an unobtrusive measure related to their relationship quality, trust towards the clinician, and pain. These findings suggest that interpersonal synchrony may be associated with better patient outcomes, independent of the specific treatment provided.
Acknowledgments
Funding: this work was supported by the National Institutes of Health grants 2R01MH076136 and R01DA035484 (T.D.W., PI).
Footnotes
The authors declare that they have no competing interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Altmann U: Investigation of Movement Synchrony Using Windowed Cross-Lagged Regression In: Esposito A, Vinciarelli A, Vicsi K, Pelachaud C, Nijholt A, editors. Analysis of Verbal and Nonverbal Communication and Enactment The Processing Issues Berlin, Heidelberg: Springer Berlin Heidelberg; page 335–45, 2011. [Google Scholar]
- 2.American Society of Anesthesiologists Task Force on Acute Pain Management: Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology 100:1573–81, 2004. [DOI] [PubMed] [Google Scholar]
- 3.Apfelbaum JL, Chen C, Mehta SS, Gan TJ: Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg 97:534–40, table of contents, 2003. [DOI] [PubMed] [Google Scholar]
- 4.Aslaksen PM, Myrbakk IN, Høifødt RS, Flaten MA: The effect of experimenter gender on autonomic and subjective responses to pain stimuli. Pain 129:260–8, 2007. [DOI] [PubMed] [Google Scholar]
- 5.Association WVS, Others: World values survey wave 5 2005−−2008 official aggregate v. 20140429. Madrid: Asep/JDS, Aggregate File Producer; 2005. [Google Scholar]
- 6.Atlas LY, Wager TD: A meta-analysis of brain mechanisms of placebo analgesia: consistent findings and unanswered questions. Handb Exp Pharmacol 225:37–69, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bair MJ, Robinson RL, Katon W, Kroenke K: Depression and pain comorbidity: a literature review. Arch Intern Med 163:2433–45, 2003. [DOI] [PubMed] [Google Scholar]
- 8.Barrier PA, Li JTC, Jensen NM: Two words to improve physician-patient communication: what else? Mayo Clin Proc 78:211–4, 2003. [DOI] [PubMed] [Google Scholar]
- 9.Bartoshuk LM, Fast K, Snyder DJ: Differences in Our Sensory Worlds: Invalid Comparisons With Labeled Scales. Curr Dir Psychol Sci SAGE Publications Inc; 14:122–5, 2005. [Google Scholar]
- 10.Bazargan M, Norris K, Bazargan-Hejazi S, Akhanjee L, Calderon JL, Safvati SD, Baker RS: Alternative healthcare use in the under-served population. Ethn Dis 15:531–9, 2005. [PubMed] [Google Scholar]
- 11.Behrends A, Müller S, Dziobek I: Moving in and out of synchrony: A concept for a new intervention fostering empathy through interactional movement and dance. The Arts in Psychotherapy 39:107–16, 2012. [Google Scholar]
- 12.Belasen A, Belasen AT: Doctor-patient communication: a review and a rationale for using an assessment framework. J Health Organ Manag 32:891–907, 2018. [DOI] [PubMed] [Google Scholar]
- 13.Bernieri JF, Rosenthal R: 11 Interpersonal coordination: Behavior matching and interactional synchrony. Fundamentals of nonverbal behavior [Internet] 401:, 1991. Available from: https://www.google.com/books?hl=iw&lr=&id=3quRXGmDGvQC&oi=fnd&pg=PA401&dq=11.+Interpersonal+coordination:+Behavior+matching+and+interactional+synchrony&ots=B85WLCQ7d0&sig=a-6C0NuRVOwluX5RF1VibhfSSo8 [Google Scholar]
- 14.Bingel U, Colloca L, Vase L: Mechanisms and Clinical Implications of the Placebo Effect: Is There a Potential for the Elderly? A Mini-Review. Gerontology 57:354–63, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bird ST, Bogart LM, Delahanty DL: Health-related correlates of perceived discrimination in HIV care. AIDS Patient Care STDS 18:19–26, 2004. [DOI] [PubMed] [Google Scholar]
- 16.Boesch E, Bellan V, Moseley GL, Stanton TR: The effect of bodily illusions on clinical pain: a systematic review and meta-analysis. Pain journals.lww.com; 157:516–29, 2016. [DOI] [PubMed] [Google Scholar]
- 17.Bogardus ST Jr, Holmboe E, Jekel JF: Perils, pitfalls, and possibilities in talking about medical risk. JAMA 281:1037–41, 1999. [DOI] [PubMed] [Google Scholar]
- 18.Breivik H: Postoperative pain management: why is it difficult to show that it improves outcome? Eur J Anaesthesiol 15:748–51, 1998. [DOI] [PubMed] [Google Scholar]
- 19.Brener L, von Hippel W, von Hippel C, Resnick I, Treloar C: Perceptions of discriminatory treatment by staff as predictors of drug treatment completion: utility of a mixed methods approach. Drug Alcohol Rev 29:491–7, 2010. [DOI] [PubMed] [Google Scholar]
- 20.Brown JL, Sheffield D, Leary MR, Robinson ME: Social support and experimental pain. Psychosom Med 65:276–83, 2003. [DOI] [PubMed] [Google Scholar]
- 21.Bull SA, Henry Hu X, Hunkeler EM, Lee JY, Ming EE, Markson LE, Fireman B: Discontinuation of Use and Switching of Antidepressants: Influence of Patient-Physician Communication. JAMA American Medical Association; 288:1403–9, 2002. [DOI] [PubMed] [Google Scholar]
- 22.Burgess DJ, Ding Y, Hargreaves M, van Ryn M, Phelan S: The association between perceived discrimination and underutilization of needed medical and mental health care in a multi-ethnic community sample. J Health Care Poor Underserved 19:894–911, 2008. [DOI] [PubMed] [Google Scholar]
- 23.Byrne PS, Heath CC: Practitioners’ use of non-verbal behaviour in real consultations. J R Coll Gen Pract 30:327–31, 1980. [PMC free article] [PubMed] [Google Scholar]
- 24.Bystad M, Bystad C, Wynn R: How can placebo effects best be applied in clinical practice? A narrative review. Psychol Res Behav Manag 8:41–5, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carr DB, Goudas LC: Acute pain. Lancet 353:2051–8, 1999. [DOI] [PubMed] [Google Scholar]
- 26.Casagrande SS, Gary TL, LaVeist TA, Gaskin DJ, Cooper LA: Perceived discrimination and adherence to medical care in a racially integrated community. J Gen Intern Med 22:389–95, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chan BL, Witt R, Charrow AP, Magee A, Howard R, Pasquina PF, Heilman KM, Tsao JW: Mirror therapy for phantom limb pain. New England Journal of Medicine Mass Medical Soc; 357:2206–7, 2007. [DOI] [PubMed] [Google Scholar]
- 28.Chapman EN, Kaatz A, Carnes M: Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med 28:1504–10, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ciechanowski PS, Katon WJ, Russo JE, Walker EA: The patient-provider relationship: attachment theory and adherence to treatment in diabetes. Am J Psychiatry 158:29–35, 2001. [DOI] [PubMed] [Google Scholar]
- 30.Cikara M, Van Bavel JJ: The Neuroscience of Intergroup Relations: An Integrative Review. Perspect Psychol Sci 9:245–74, 2014. [DOI] [PubMed] [Google Scholar]
- 31.Cohen J: Statistical power analysis for the behavioral sciences second edition. Lawrence Erlbaum Associates, Publishers, 1988. [Google Scholar]
- 32.Colloca L, Benedetti F: Placebo analgesia induced by social observational learning. Pain 144:28–34, 2009. [DOI] [PubMed] [Google Scholar]
- 33.Colloca L, Klinger R, Flor H, Bingel U: Placebo analgesia: psychological and neurobiological mechanisms. Pain 154:511–4, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, Greenwald AG, Inui TS: The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health 102:979–87, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR: Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med 139:907–15, 2003. [DOI] [PubMed] [Google Scholar]
- 36.Cousins MJ, Power I, Smith G: 1996 Labat Lecture: Pain—A Persistent Problem. Reg Anesth Pain Med 25:6, 2000. [DOI] [PubMed] [Google Scholar]
- 37.Craig KD: The social communication model of pain. Canadian Psychology/Psychologie canadienne Educational Publishing Foundation; 50:22, 2009. [Google Scholar]
- 38.Dehon E, Weiss N, Jones J, Faulconer W, Hinton E, Sterling S: A Systematic Review of the Impact of Physician Implicit Racial Bias on Clinical Decision Making. Acad Emerg Med 24:895–904, 2017. [DOI] [PubMed] [Google Scholar]
- 39.Delaherche E, Chetouani M, Mahdhaoui A, Saint-Georges C, Viaux S, Cohen D: Interpersonal Synchrony: A Survey of Evaluation Methods across Disciplines. IEEE Transactions on Affective Computing 3:349–65, 2012. [Google Scholar]
- 40.Derose KP, Hays RD, McCaffrey DF, Baker DW: Does physician gender affect satisfaction of men and women visiting the emergency department? J Gen Intern Med 16:218–26, 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dijksterhuis A, Bargh JA: The perception-behavior expressway: Automatic effects of social perception on social behavior Advances in Experimental Social Psychology Academic Press; page 1–402001. [Google Scholar]
- 42.Dikker S, Wan L, Davidesco I, Kaggen L, Oostrik M, McClintock J, Rowland J, Michalareas G, Van Bavel JJ, Ding M, Poeppel D: Brain-to-Brain Synchrony Tracks Real-World Dynamic Group Interactions in the Classroom. Curr Biol 27:1375–80, 2017. [DOI] [PubMed] [Google Scholar]
- 43.DiMatteo MR, Hays RD, Prince LM: Relationship of physicians’ nonverbal communication skill to patient satisfaction, appointment noncompliance, and physician workload. Health Psychol 5:581–94, 1986. [DOI] [PubMed] [Google Scholar]
- 44.DiMatteo MR, Taranta A, Friedman HS, Prince LM: Predicting patient satisfaction from physicians’ nonverbal communication skills. Med Care 18:376–87, 1980. [DOI] [PubMed] [Google Scholar]
- 45.Dumas G, Lachat F, Martinerie J, Nadel J, George N: From social behaviour to brain synchronization: Review and perspectives in hyperscanning . IRBM [Internet] 32:, 2011. Available from: 10.1016/j.irbm.2011.01.002 [DOI] [Google Scholar]
- 46.Enck P, Benedetti F, Schedlowski M: New insights into the placebo and nocebo responses. Neuron 59:195–206, 2008. [DOI] [PubMed] [Google Scholar]
- 47.Federman DJ: Kinesthetic ability and the development of empathy in Dance Movement Therapy. Journal of Applied Arts & Health 2:137–54, 2011. [Google Scholar]
- 48.Feldman R: Mutual influences between child emotion regulation and parent-child reciprocity support development across the first 10 years of life: Implications for developmental psychopathology. Dev Psychopathol 27:1007–23, 2015. [DOI] [PubMed] [Google Scholar]
- 49.Feldman R, Magori-Cohen R, Galili G, Singer M, Louzoun Y: Mother and infant coordinate heart rhythms through episodes of interaction synchrony. Infant Behav Dev Elsevier; 34:569–77, 2011. [DOI] [PubMed] [Google Scholar]
- 50.Finset A: 50 years of research on the effect of physician communication behavior on health outcomes. Patient Educ Couns 96:1–2, 2014. [DOI] [PubMed] [Google Scholar]
- 51.Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS: Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clin J Pain 13:116–37, 1997. [DOI] [PubMed] [Google Scholar]
- 52.FitzGerald C, Hurst S: Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics 18:19, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Foell J, Bekrater-Bodmann R, Diers M, Flor H: Mirror therapy for phantom limb pain: brain changes and the role of body representation. Eur J Pain 18:729–39, 2014. [DOI] [PubMed] [Google Scholar]
- 54.Friedman R : Improving Communication Between Doctor and PatientImproving Communication Between Doctor and Patient Wedding D, editor. PsycCRITIQUES [Internet] 6262:, 2017. Available from: http://access.portico.org/stable?au=phzpnwm6f [Google Scholar]
- 55.Gashi S, Di Lascio E, Santini S: Using Students’ Physiological Synchrony to Quantify the Classroom Emotional Climate. Proceedings of the 2018 ACM International Joint Conference and 2018 International Symposium on Pervasive and Ubiquitous Computing and Wearable Computers New York, NY, USA: ACM; page 698–701, 2018. [Google Scholar]
- 56.Glover LM, Sims M, Winters K: Perceived Discrimination and Reported Trust and Satisfaction with Providers in African Americans: The Jackson Heart Study. Ethn Dis 27:209–16, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Goldstein P, Shamay-Tsoory GS, Yellinek S, Weissman-Fogel I: Empathy predicts an experimental pain reduction during touch. J Pain [Internet] Elsevier;, 2016. Available from: http://www.sciencedirect.com/science/article/pii/S1526590016301080 [DOI] [PubMed]
- 58.Goldstein P, Weissman-Fogel I, Dumas G, Shamay-Tsoory SG: Brain-to-brain coupling during handholding is associated with pain reduction. Proc Natl Acad Sci U S A 115:E2528–37, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Goldstein P, Weissman-Fogel I, Shamay-Tsoory SG: The role of touch in regulating inter-partner physiological coupling during empathy for pain. Sci Rep 7:3252, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gordon HS, Street RL Jr, Sharf BF, Kelly PA, Souchek J: Racial differences in trust and lung cancer patients’ perceptions of physician communication. J Clin Oncol 24:904–9, 2006. [DOI] [PubMed] [Google Scholar]
- 61.Gormley P, Anttila V, Winsvold BS, Palta P, Esko T, Pers TH, Farh K-H, Cuenca-Leon E, Muona M, Furlotte NA, Kurth T, Ingason A, McMahon G, Ligthart L, Terwindt GM, Kallela M, Freilinger TM, Ran C, Gordon SG, Stam AH, Steinberg S, Borck G, Koiranen M, Quaye L, Adams HHH, Lehtimäki T, Sarin A-P, Wedenoja J, Hinds DA, Buring JE, Schürks M, Ridker PM, Hrafnsdottir MG, Stefansson H, Ring SM, Hottenga J-J, Penninx BWJH, Färkkilä M, Artto V, Kaunisto M, Vepsäläinen S, Malik R, Heath AC, Madden PAF, Martin NG, Montgomery GW, Kurki MI, Kals M, Mägi R, Pärn K, Hämäläinen E, Huang H, Byrnes AE, Franke L, Huang J, Stergiakouli E, Lee PH, Sandor C, Webber C, Cader Z, Muller-Myhsok B, Schreiber S, Meitinger T, Eriksson JG, Salomaa V, Heikkilä K, Loehrer E, Uitterlinden AG, Hofman A, van Duijn CM, Cherkas L, Pedersen LM, Stubhaug A, Nielsen CS, Männikkö M, Mihailov E, Milani L, Göbel H, Esserlind A-L, Christensen AF, Hansen TF, Werge T, International Headache Genetics Consortium, Kaprio J, Aromaa AJ, Raitakari O, Ikram MA, Spector T, Järvelin M-R, Metspalu A, Kubisch C, Strachan DP, Ferrari MD, Belin AC, Dichgans M, Wessman M, van den Maagdenberg AMJM, Zwart J-A, Boomsma DI, et al. : Meta-analysis of 375,000 individuals identifies 38 susceptibility loci for migraine. Nat Genet 48:856–66, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Greffrath W, Baumgärtner U, Treede R-D: Peripheral and central components of habituation of heat pain perception and evoked potentials in humans. Pain 132:301–11, 2007. [DOI] [PubMed] [Google Scholar]
- 63.Hale J, Ward JA, Buccheri F, Oliver D, Hamilton AF de C: Are You on My Wavelength? Interpersonal Coordination in Dyadic Conversations. J Nonverbal Behav [Internet], 2019. Available from: 10.1007/s109-19-01900320-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hall MA, Zheng B, Dugan E, Camacho F, Kidd KE, Mishra A, Balkrishnan R: Measuring patients’ trust in their primary care providers. Med Care Res Rev 59:293–318, 2002. [DOI] [PubMed] [Google Scholar]
- 65.Haroutiunian S, Nikolajsen L, Finnerup NB, Jensen TS: The neuropathic component in persistent postsurgical pain: a systematic literature review. Pain 154:95–102, 2013. [DOI] [PubMed] [Google Scholar]
- 66.Harrigan JA, Oxman TE, Rosenthal R: Rapport expressed through nonverbal behavior. J Nonverbal Behav 9:95–110, 1985. [Google Scholar]
- 67.Harrigan JA, Rosenthal R: Physicians’ H]ead and Body Positions as Determinants of Perceived Rapport. J Appl Social Pyschol 13:496–509, 1983. [Google Scholar]
- 68.Hart Y, Czerniak E, Karnieli-Miller O, Mayo AE, Ziv A, Biegon A, Citron A, Alon U: Automated Video Analysis of Non-verbal Communication in a Medical Setting. Front Psychol 7:1130, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hausmann LRM, Jeong K, Bost JE, Ibrahim SA: Perceived discrimination in health care and use of preventive health services. J Gen Intern Med 23:1679–84, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hein G, Engelmann JB, Tobler PN: Pain relief provided by an outgroup member enhances analgesia. Proc Biol Sci [Internet] 285:, 2018. Available from: 10.1098/rspb.2018.0501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hunter T, Siess F, Colloca L: Socially induced placebo analgesia: a comparison of a pre-recorded versus live face-to-face observation. Eur J Pain 18:914–22, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jamison RN, Edwards RR, Liu X, Ross EL, Michna E, Warnick M, Wasan AD: Relationship of negative affect and outcome of an opioid therapy trial among low back pain patients. Pain Pract Wiley Online Library; 13:173–81, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sabin Janice A., Nosek Brian A., Greenwald Anthony G., Rivara Frederick P.: Physicians’ Implicit and Explicit Attitudes About Race by MD Race, Ethnicity, and Gender. J Health Care Poor Underserved 20:896–913, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jepma M, Jones M, Wager TD: The dynamics of pain: evidence for simultaneous site-specific habituation and site-nonspecific sensitization in thermal pain. J Pain 15:734–46, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Josef L, Goldstein P, Mayseless N, Ayalon L, Shamay-Tsoory SG: The oxytocinergic system mediates synchronized interpersonal movement during dance. Sci Rep 9:1894, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kawi J, Lukkahatai N, Inouye J, Thomason D, Connelly K: Effects of Exercise on Select Biomarkers and Associated Outcomes in Chronic Pain Conditions: Systematic Review. Biol Res Nurs 18:147–59, 2016. [DOI] [PubMed] [Google Scholar]
- 77.Kee JWY, Khoo HS, Lim I, Koh MYH: Communication Skills in Patient-Doctor Interactions: Learning from Patient Complaints. Health Professions Education 4:97–106, 2018. [Google Scholar]
- 78.Khan AN, Jacobsen HE, Khan J, Filippi CG, Levine M, Lehman RA Jr, Riew KD, Lenke LG, Chahine NO: Inflammatory biomarkers of low back pain and disc degeneration: a review. Ann N Y Acad Sci 1410:68–84, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Khan FH, Hanif R, Tabassum R, Qidwai W, Nanji K: Patient Attitudes towards Physician Nonverbal Behaviors during Consultancy: Result from a Developing Country. ISRN Family Med 2014:473654, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Koenig HG, Büssing A: The Duke University Religion Index (DUREL): A Five-Item Measure for Use in Epidemological Studies. Religions Molecular Diversity Preservation International; 1:78–85, 2010. [Google Scholar]
- 81.Koller M: robustlmm : An R Package for Robust Estimation of Linear Mixed-Effects Models. J Stat Softw UCLA Statistics; 75:24, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Konvalinka I, Xygalatas D, Bulbulia J, Schjødt U, Jegindø E-M, Wallot S, Van Orden G, Roepstorff A: Synchronized arousal between performers and related spectators in a fire-walking ritual. Proceedings of the National Academy of Sciences National Acad Sciences; 108:8514–9, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Koole SL, Tschacher W: Synchrony in Psychotherapy: A Review and an Integrative Framework for the Therapeutic Alliance. Front Psychol 7:862, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Koss T, Rosenthal R: Interactional synchrony, positivity, and patient satisfaction in the physician-patient relationship. Med Care 35:1158–63, 1997. [DOI] [PubMed] [Google Scholar]
- 85.Kret ME: Emotional expressions beyond facial muscle actions. A call for studying autonomic signals and their impact on social perception. Front Psychol 6:711, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kret ME, De Dreu CKW: Pupil-mimicry conditions trust in partners: moderation by oxytocin and group membership. Proc Biol Sci [Internet] 284:, 2017. Available from: 10.1098/rspb.2016.2554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kushnir T, Bachner YG, Carmel S, Flusser H, Galil A: Pediatricians?? Communication Styles as Correlates of Global Trust Among Jewish and Bedouin Parents of Disabled Children. J Dev Behav Pediatr [Internet] PAP:, 2008. Available from: https://insights.ovid.com/crossref?an=00004703-900000000-99994 [DOI] [PubMed] [Google Scholar]
- 88.Lang M, Bahna V, Shaver JH, Reddish P, Xygalatas D: Sync to link: Endorphin-mediated synchrony effects on cooperation. Biol Psychol 127:191–7, 2017. [DOI] [PubMed] [Google Scholar]
- 89.Laska KM, Gurman AS, Wampold BE: Expanding the lens of evidence-based practice in psychotherapy: a common factors perspective. Psychotherapy 51:467–81, 2014. [DOI] [PubMed] [Google Scholar]
- 90.Laveist TA, Nuru-Jeter A: Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav 43:296–306, 2002. [PubMed] [Google Scholar]
- 91.Leclère C, Viaux S, Avril M, Achard C, Chetouani M, Missonnier S, Cohen D: Why synchrony matters during mother-child interactions: a systematic review. PLoS One [Internet] 9:, 2014. Available from: 10.1371/journal.pone.0113571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lee LJ, Batal HA, Maselli JH, Kutner JS: Effect of Spanish Interpretation Method on Patient Satisfaction in an Urban Walk-in Clinic. J Gen Intern Med Wiley Online Library; 17:641–6, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Levine FM, De Simone LL: The effects of experimenter gender on pain report in male and female subjects. Pain 44:69–72, 1991. [DOI] [PubMed] [Google Scholar]
- 94.Loeser JD, Melzack R: Pain: an overview. Lancet 353:1607–9, 1999. [DOI] [PubMed] [Google Scholar]
- 95.Losin EAR, Anderson SR, Wager TD: Feelings of Clinician-Patient Similarity and Trust Influence Pain: Evidence From Simulated Clinical Interactions. J Pain 18:787–99, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Losin EAR, Cross KA, Iacoboni M, Dapretto M: Neural processing of race during imitation: self-similarity versus social status. Hum Brain Mapp 35:1723–39, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lumsden J, Miles LK, Macrae CN: Sync or sink? Interpersonal synchrony impacts self-esteem. Front Psychol 5:1064, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Macrae WA: Chronic pain after surgery. Br J Anaesth 87:88–98, 2001. [DOI] [PubMed] [Google Scholar]
- 99.Macrae WA: Chronic post-surgical pain: 10 years on. Br J Anaesth 101:77–86, 2008. [DOI] [PubMed] [Google Scholar]
- 100.Makoul G, van Dulmen S: What Is Effective Doctor-Patient Communication? Review of the Evidence In: Brown J, Noble LM, Papageorgiou A, Kidd J, editors. Clinical Communication in Medicine Chichester, UK: John Wiley & Sons, Ltd; page 30–9, 2015. [Google Scholar]
- 101.Margolius D, Bodenheimer T: Transforming primary care: from past practice to the practice of the future. Health Aff 29:779–84, 2010. [DOI] [PubMed] [Google Scholar]
- 102.Mast MS: On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Couns 67:315–8, 2007. [DOI] [PubMed] [Google Scholar]
- 103.Mathur VA, Richeson JA, Paice JA, Muzyka M, Chiao JY: Racial bias in pain perception and response: experimental examination of automatic and deliberate processes. J Pain 15:476–84, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.McCarthy DM, Buckley BA, Engel KG, Forth VE, Adams JG, Cameron KA: Understanding patient-provider conversations: what are we talking about? Acad Emerg Med 20:441–8, 2013. [DOI] [PubMed] [Google Scholar]
- 105.McWilliams LA, Cox BJ, Enns MW: Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain 106:127–33, 2003. [DOI] [PubMed] [Google Scholar]
- 106.Mistiaen P, van Osch M, van Vliet L, Howick J, Bishop FL, Di Blasi Z, Bensing J, van Dulmen S: The effect of patient-practitioner communication on pain: a systematic review. Eur J Pain 20:675–88, 2016. [DOI] [PubMed] [Google Scholar]
- 107.Montague E, Chen P-Y, Xu J, Chewning B, Barrett B: Nonverbal interpersonal interactions in clinical encounters and patient perceptions of empathy. J Particip Med 5:e33, 2013. [Google Scholar]
- 108.Nagaoka C, Komori M: Body Movement Synchrony in Psychotherapeutic Counseling: A Study Using the Video-Based Quantification Method. IEICE Trans Inf Syst E91.D:1634. –40, 2008. [Google Scholar]
- 109.Noy L, Dekel E, Alon U: The mirror game as a paradigm for studying the dynamics of two people improvising motion together. Proceedings of the National Academy of Sciences National Acad Sciences; 108:20947–52, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nwagwu CD, Sarris C, Tao Y-X, Mammis A: Biomarkers for Chronic Neuropathic Pain and their Potential Application in Spinal Cord Stimulation: A Review. Transl Perioper Pain Med 1:33–8, 2016. [PMC free article] [PubMed] [Google Scholar]
- 111.Oullier O, de Guzman GC, Jantzen KJ, Lagarde J, Kelso JAS: Social coordination dynamics: measuring human bonding. Soc Neurosci 3:178–92, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Palumbo RV, Marraccini ME, Weyandt LL, Wilder-Smith O, McGee HA, Liu S, Goodwin MS: Interpersonal Autonomic Physiology: A Systematic Review of the Literature. Pers Soc Psychol Rev 21:99–141, 2017. [DOI] [PubMed] [Google Scholar]
- 113.Paternotte E, van Dulmen S, van der Lee N, Scherpbier AJJA, Scheele F: Factors influencing intercultural doctor–patient communication: A realist review. Patient Educ Couns Elsevier; 98:420–45, 2015. [DOI] [PubMed] [Google Scholar]
- 114.Paulick J, Deisenhofer A-K, Ramseyer F, Tschacher W, Boyle K, Rubel J, Lutz W: Nonverbal synchrony: A new approach to better understand psychotherapeutic processes and drop-out. J Psychother Integr 28:367–84, 2018. [Google Scholar]
- 115.Paxton A, Dale R: Frame-differencing methods for measuring bodily synchrony in conversation. Behav Res Methods 45:329–43, 2013. [DOI] [PubMed] [Google Scholar]
- 116.Penner LA, Hagiwara N, Eggly S, Gaertner SL, Albrecht TL, Dovidio JF: Racial Healthcare Disparities: A Social Psychological Analysis. Eur Rev Soc Psychol 24:70–122, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Perkins FM, Kehlet H: Chronic Pain as an Outcome of SurgeryA Review of Predictive Factors. Anesthesiology The American Society of Anesthesiologists; 93:1123–33, 2000. [DOI] [PubMed] [Google Scholar]
- 118.Prinz W: A Common Coding Approach to Perception and Action In: Neumann O, Prinz W, editors. Relationships Between Perception and Action: Current Approaches Berlin, Heidelberg: Springer Berlin Heidelberg; page 167–201, 1990. [Google Scholar]
- 119.Prochazkova E, Kret ME: Connecting minds and sharing emotions through mimicry: A neurocognitive model of emotional contagion. Neurosci Biobehav Rev 80:99–114, 2017. [DOI] [PubMed] [Google Scholar]
- 120.Ramseyer F, Tschacher W: Nonverbal synchrony in psychotherapy: coordinated body movement reflects relationship quality and outcome. J Consult Clin Psychol 79:284–95, 2011. [DOI] [PubMed] [Google Scholar]
- 121.Ramseyer F, Tschacher W: Nonverbal synchrony of head- and body-movement in psychotherapy: different signals have different associations with outcome. Front Psychol 5:979, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Reddan MC, Wager TD: Modeling Pain Using fMRI: From Regions to Biomarkers. Neurosci Bull 34:208–15, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Riess H, Kraft-Todd G: EMPATHY: a tool to enhance nonverbal communication between clinicians and their patients. Acad Med LWW; 89:1108–12, 2014. [DOI] [PubMed] [Google Scholar]
- 124.Roberts MH, Klatzkin RR, Mechlin B: Social Support Attenuates Physiological Stress Responses and Experimental Pain Sensitivity to Cold Pressor Pain. Ann Behav Med 49:557–69, 2015. [DOI] [PubMed] [Google Scholar]
- 125.Ronchetti E: Small sample asymptotics: a review with applications to robust statistics. Comput Stat Data Anal Elsevier; 10:207–23, 1990. [Google Scholar]
- 126.Ryan AM, Gee GC, Griffith D: The effects of perceived discrimination on diabetes management. J Health Care Poor Underserved 19:149–63, 2008. [DOI] [PubMed] [Google Scholar]
- 127.Sabin JA, Greenwald AG: The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. Am J Public Health 102:988–95, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sebanz N, Bekkering H, Knoblich G: Joint action: bodies and minds moving together. Trends Cogn Sci Elsevier; 10:70–6, 2006. [DOI] [PubMed] [Google Scholar]
- 129.Siller M, Sigman M: The behaviors of parents of children with autism predict the subsequent development of their children’s communication. J Autism Dev Disord 32:77–89, 2002. [DOI] [PubMed] [Google Scholar]
- 130.Smith CK, Larsen KM: Sequential nonverbal behavior in the patient-physician interview. J Fam Pract 18:257–61, 1984. [PubMed] [Google Scholar]
- 131.Stepanikova I, Zhang Q, Wieland D, Eleazer GP, Stewart T: Non-verbal communication between primary care physicians and older patients: how does race matter? J Gen Intern Med 27:576–81, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC: Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain 17:52–64, 2001. [DOI] [PubMed] [Google Scholar]
- 133.Sullivan P, Blacker M: The Effect of Different Phases of Synchrony on Pain Threshold in a Drumming Task. Front Psychol 8:1034, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Tafjel H, Turner JC: An Integrative Theory of Intergroup Conflict. 1979.
- 135.Tanner RJ, Ferraro R, Chartrand TL, Bettman JR, Van Baaren R: Of Chameleons and Consumption: The Impact of Mimicry on Choice and Preferences. J Consum Res Oxford University Press; 34:754–66, 2008. [Google Scholar]
- 136.Tarr B, Launay J, Cohen E, Dunbar R: Synchrony and exertion during dance independently raise pain threshold and encourage social bonding. Biol Lett [Internet] 11:, 2015. Available from: 10.1098/rsbl.2015.0767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Tarr B, Launay J, Dunbar RIM: Silent disco: dancing in synchrony leads to elevated pain thresholds and social closeness. Evol Hum Behav 37:343–9, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Thom DH, Wong ST, Guzman D, Wu A, Penko J, Miaskowski C, Kushel M: Physician trust in the patient: development and validation of a new measure. Ann Fam Med 9:148–54, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Thompson L: Theoretical approaches in dance-movement therapy. vol. II: Bernstein Penny Lewis, Editor (Dubuque: Kendall/Hunt Publishing Company, 1984, 368 pages, $16.95; ). The Arts in Psychotherapy 13:349–51, 1986. [Google Scholar]
- 140.Tingley D, Yamamoto T, Hirose K, Keele L, Imai K: mediation: R Package for Causal Mediation Analysis. Journal of Statistical Software, Articles 59:1–38, 2014.26917999 [Google Scholar]
- 141.Trivedi AN, Ayanian JZ: Perceived discrimination and use of preventive health services. J Gen Intern Med 21:553–8, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Tsang A, Von Korff M, Lee S, Alonso J, Karam E, Angermeyer MC, Borges GLG, Bromet EJ, Demytteneare K, de Girolamo G, de Graaf R, Gureje O, Lepine J-P, Haro JM, Levinson D, Oakley Browne MA, Posada-Villa J, Seedat S, Watanabe M: Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain 9:883–91, 2008. [DOI] [PubMed] [Google Scholar]
- 143.Tschacher W, Rees GM, Ramseyer F: Nonverbal synchrony and affect in dyadic interactions. Front Psychol 5:1323, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Tuttle AH, Tohyama S, Ramsay T, Kimmelman J, Schweinhardt P, Bennett GJ, Mogil JS: Increasing placebo responses over time in U.S. clinical trials of neuropathic pain. Pain 156:2616–26, 2015. [DOI] [PubMed] [Google Scholar]
- 145.Twersky R, Fishman D, Homel P: What happens after discharge? Return hospital visits after ambulatory surgery. Anesth Analg 84:319–24, 1997. [DOI] [PubMed] [Google Scholar]
- 146.Van Bavel JJ, Cunningham WA: A social identity approach to person memory: group membership, collective identification, and social role shape attention and memory. Pers Soc Psychol Bull 38:1566–78, 2012. [DOI] [PubMed] [Google Scholar]
- 147.Van Houtven CH, Voils CI, Oddone EZ, Weinfurt KP, Friedman JY, Schulman KA, Bosworth HB: Perceived discrimination and reported delay of pharmacy prescriptions and medical tests. J Gen Intern Med 20:578–83, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Varlet M, Marin L, Lagarde J, Bardy BG: Social postural coordination. J Exp Psychol Hum Percept Perform 37:473–83, 2011. [DOI] [PubMed] [Google Scholar]
- 149.Wamala S, Merlo J, Boström G, Hogstedt C: Perceived discrimination, socioeconomic disadvantage and refraining from seeking medical treatment in Sweden. J Epidemiol Community Health 61:409–15, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Weinberger M, Greene JY, Mamlin JJ: The impact of clinical encounter events on patient and physician satisfaction. Soc Sci Med E 15:239–44, 1981. [DOI] [PubMed] [Google Scholar]
- 151.Wheatley T, Kang O, Parkinson C, Looser CE: From mind perception to mental connection: Synchrony as a mechanism for social understanding. Soc Personal Psychol Compass Wiley Online Library; 6:589–606, 2012. [Google Scholar]
- 152.Wilcox RR: Introduction to Robust Estimation and Hypothesis Testing. Academic Press; 2011. [Google Scholar]
- 153.Włoszczak-Szubzda A, Jarosz MJ, Goniewicz M, Goniewicz K: Evaluation of communication and acceptance of the patients by medical personnel. Rocz Panstw Zakl Hig 67:427–33, 2016. [PubMed] [Google Scholar]
- 154.Young J: The Therapeutic Movement Relationship in Dance/Movement Therapy: A Phenomenological Study. Am J Dance Ther Springer US; 39:93–112, 2017. [Google Scholar]
- 155.Zeileis A: Object-oriented Computation of Sandwich Estimators. Vienna: Department of Statistics and Mathematics, WU Vienna University of Economics and Business; :10, 2006. [Google Scholar]
- 156.Zu J, Yuan K-H: Local Influence and Robust Procedures for Mediation Analysis. Multivariate Behav Res Taylor & Francis; 45:1–44, 2010. [DOI] [PubMed] [Google Scholar]