Supplemental Digital Content is Available in the Text.
Key Words: PrEP, social network analysis, Black MSM
Abstract
Objectives:
We tested preliminary efficacy of a peer change agent type I network intervention to increase pre-exposure prophylaxis (PrEP) linkage to care among network members connected to young Black men who have sex with men.
Design:
Parent study is a pragmatic randomized controlled trial with 110 weeks of total follow-up. Interim midpoint analyses are performed here using participant data before crossover assignment at 55 weeks.
Methods:
We randomly assigned 423 participants in Chicago to receive the network intervention, an opinion leader workshop with telephonic booster sessions, versus a time-matched control from 2016 to 2018. The consolidated surrogate outcome was PrEP referral and linkage to clinical care among network members connected to study participants and was collected from independent administrative data.
Results:
Each study participant in the trial (n = 423) had on average 1822 network contacts who could be eligible for PrEP referral and linkage. During the 55-week observation period, PrEP referral was most likely to occur within 3 days of an intervention session compared to control [odds ratio (OR) 0.07 (0.02–0.013); P = 0.007] resulting in 1–2 referrals of network members per session. Network members with referral or linkage were more likely to be connected to study participants in the intervention arm than the control condition [aOR 1.50 (1.09–2.06); P = 0.012].
Conclusions:
A peer change agent type I network intervention is preliminarily effective at diffusing PrEP through a network of individuals highly susceptible to HIV over 55 weeks. This low-intensity intervention demonstrated network-level impact among populations that have experienced limited PrEP care engagement in the United States.
HIV prevention in the form of pre-exposure prophylaxis (PrEP) has demonstrated efficacy with FDA approval in 2012 for use in adults as once daily tenofovir/emtricitabine.1 More recently, there have been several PrEP advances, particularly in the timing of dosing,2 extension to individuals aged 13–17 years,3 and a newly efficacious product.4 During this timeframe, studies have documented limited PrEP awareness, referral, and linkage to care among several populations experiencing high HIV incidence, most notably young Black men who have sex with men (YBMSM).5–8 Broad implementation strategies are therefore required to improve the uptake of PrEP within most impacted populations.9,10
Decades of social diffusion research underscores the impact of social relationships in the adoption and spread of novel health interventions in a population.11 Diffusion of biomedical innovation has been described in landmark observational studies, such as the context of family-planning methods12,13 and in the diffusion of prescribing practices through provider networks.14 Underlying all diffusion processes is that innovation will spread to others through interpersonal networks.11 More recently, advances in network interventions have been proposed to accelerate this diffusion process from a public health framework. Network interventions, whether they aim to diffuse biomedical or behavioral innovations, are categorized as 4 types.15 The most common approach is a type 1 peer change agent approach where individuals are selected based upon their popularity or socially advantageous network position and trained to deliver innovation to others within their networks. This approach has been used previously in many other contexts including diabetes self-management, treatment of myocardial infarction, and vaginal delivery after previous cesarean section.16–19
Here, we describe the midpoint 55-week impact of PrEP Chicago, a type 1 network intervention. PrEP Chicago was developed to engage YBMSM—a population estimated to have a 1 in 2 chance of acquiring HIV in their lifetime.9 If successful, the intervention would be an important implementation strategy for ending the epidemic in the United States.20
METHODS
Study Population
The PrEP Chicago intervention recruited YBMSM living in Chicago and adjacent neighborhoods from 2016 to 2018. Cook County (Chicago) is a joint NIH/DHSS designated ending the epidemic jurisdiction and ranks third in total HIV burden in the United States.21 During the study period, the citywide PrEP4Love PrEP information campaign was in existence and included a warmline that provides information on PrEP and referral to PrEP care throughout the city.22 Accessible PrEP care was available throughout Chicago, including a network of sexual health clinics that provide the majority of PrEP care in the Midwest irrespective of insurance status.7
Participants were eligible if they were 18–35 years of age, identified as Black/African American, were male sex at birth, had sex with a man in the past 12 months, and, because the intervention emphasizes social media as a communication tool, had an active Facebook profile. Once deemed eligible, individuals were assigned randomly to 1 of the 2 treatment conditions. Those randomized to the intervention received the PrEPChicago intervention over 55 weeks and participants randomized to the time-matched control condition received an intervention over the same period. Randomization was computer generated in 1:1 intervention to control ratio and allocated immediately by study staff after participant consent.
Study Procedures
The findings presented here represent analysis of the PrEPChicago intervention, a 2-arm pragmatic randomized trial (ClinicalTrials.gov number, NCT 02896699).23 The findings presented here include analysis before the 55-week intervention switch (baseline intervention receives control and baseline control receives intervention). PrEPChicago was approved by the institutional review board at the University of Chicago. Recruitment of study participants occurred between March 2016 and March 2017 using respondent-driven sampling,24 a variant of snowball sampling that draws on referrals, beginning with a set of initial “seeds” that meet study eligibility. Enrolled seeds are known members of the community who are asked to recruit members of their social networks into the study. After enrollment, these new participants were invited to recruit peers, and the process continued until the recruitment target was reached.
Data were collected from all participants at baseline and 12-month follow-up. To measure the PrEP diffusion outcome, digital network data were collected from each participant using Facebook's data download feature. Lists of a participant's Facebook friends at baseline were retained for analysis to match with independently collected administrative data of community members referred for PrEP or making a PrEP appointment. Data protections to secure third-party (nonparticipant) identities were established, and a waiver of consent from the IRB for third-party (nonparticipant) network members was obtained, given the minimal risk to these individuals.
Intervention Condition
The PrEP Chicago intervention aims to develop a participant's knowledge about PrEP and build skills around PrEP communication and motivation to engage peers in the PrEP care continuum.23 The intervention is composed of 2 parts: (1) a half-day, small group training workshop led by intervention staff and (2) a series of check-in calls (or “boosters”) between intervention staff and participants. The intervention workshop adapts the peer educational and mentoring program developed as part of the HIV Prevention Trials Network25,26 and is divided into 4 modules: (1) HIV facts and myths; (2) background on PrEP; (3) role playing conversations about motivating peers to engage in PrEP care; and (4) leveraging social media to spread awareness about PrEP. The third and fourth modules develop participants' PrEP engagement communication skills to increase their effectiveness as peer change agents. Participants are trained to motivate their peers to make a PrEP appointment through a number of PrEP clinics and the citywide PrEPline that refers clients to PrEP care.22 After the baseline workshop, trained staff administered a total of 8 monthly booster calls with each participant, each lasting 10–20 minutes. Boosters were designed to help participant peer change agents to devise personalized conversational strategies for approaching peers and to troubleshoot communication barriers.
Time-Matched Control Condition
Participants were randomized to the intervention condition just described or to a minimal contact attention control condition.27 The attention control condition consisted of a sexual risk assessment workshop, whereby participants wrote and discussed fictional narratives about what they believe constituted low, medium, and high HIV/STI risk scenarios.
Consolidated Surrogate Outcome
Outcome measurement in such a pragmatic randomized controlled trial28 is complicated by the fact that it is impossible to determine with certainty which participant(s) may have influenced a specific individual to engage in PrEP care activities, such as calling the PrEPline or making a clinic appointment. Moreover, information obtained by asking either party directly would likely have been incomplete and subject to reporting biases. In fact, over 80% of the data field “who recommended you to the PrEPline” was found to be missing in the citywide PrEPline database, which limited the original planned analysis. Thus, for this interim analysis, a new consolidated surrogate outcome was developed for network members not enrolled in the study who were linked to study participants over the observation period: (1) active referral to PrEP care; or (2) attendance of a first PrEP care appointment. The first source of data used to infer PrEP care engagement of network members was the citywide PrEPline database restricted to all referrals made to PrEP care over the 55-week study period, which were initiated by community members. The second source of information was electronic medical record data of all first PrEP appointments made by patients at the largest PrEP serving clinic system in Chicago over the 55-week study period. The use of warmline and clinic appointment measures collected independently of each other and independent of the study provide greater objectivity than other self-report measures typically used in diffusion of innovation studies.
To link the referral and appointment databases to the network members of study participants, a pool of network members not enrolled in the study who are linked to study participants was required. Facebook friend lists were abstracted from each study participant using the manual data download feature offered by Facebook, which allows a Facebook user to download all or parts of their data, including Facebook friends. Independent linkage of Facebook friends to the PrEPline and clinic data was conducted to determine which specific network members from this pool were either referred to PrEP care or attended a PrEP appointment, after enrollment. An honest broker not affiliated with the study and blinded to treatment condition matched Facebook aliases of study participant friends with the citywide PrEPline and clinic data. Referrals and appointments that were connected to both intervention and control participants were counted toward a specific arm based upon having more ties to a given arm; when equal ties across both arms were observed, such referrals/appointments were excluded from analyses.
Statistical Analyses
Two separate analyses were performed: (1) a timing analysis of PrEP referrals after intervention sessions; and (2) a primary comparison of intervention and control conditions. For the first approach, a timing analysis was performed to determine the relationship between intervention and the PrEP referral outcome. If the intervention was not effective in increasing the number of successful referrals, then there should be no association between the dates on which the intervention was delivered and the dates on which referrals were made. To examine this relationship, we modeled the number of PrEPline referrals initiated per day by the citywide PrEPline as a function of the number of workshops and boosters delivered on that day and the days immediately preceding, adjusting for weekly differences in the overall intensity of calls and in the number of workshops/boosters over the course of the study that might confound the causal association between them. We fit a mixed-effects negative binomial model29 to the data collected from the 55-week enrollment period. The model was fit in Stata 15.130 using maximum likelihood with mean-variance adaptive Gauss–Hermite quadrature. Estimates are presented, together with approximate 95% confidence intervals obtained by inverting the corresponding Wald test.
For the second analysis, if the intervention was not effective, then the likelihood of Facebook friends referred for PrEP or attending a PrEP appointment should be unrelated to whether the participant was assigned to the intervention or the control condition. To test this hypothesis, a conditional logistic regression31 was fit to the likelihood of Facebook friendship ties existing between study participants and those with PrEP referral or PrEP appointment as a function of participants' group assignments, adjusting for each participant's total number of Facebook friends and whether the person was referred into the study by another participant. Specifically, each PrEP referral or clinic visit among the pool of Facebook friends was treated as an independent observation for which the set of possible ties consisted of all study participants who had been recruited at the time of the referral (or visit). The model including all possible ties was fit using only those potential ties involving participants who had been recruited to the study within the first 12 weeks after intervention or control, to account for the possibility that the effect of the intervention was greatest within the first few weeks after the initial in-person session. Estimated odds ratios are presented, together with corresponding 95% confidence intervals.
RESULTS
Study Subjects
From March 2016 to March 2017, 423 individuals were recruited and randomized, with 209 assigned to the intervention group and 214 to the control group (Fig. 1). Demographic and other characteristics of the study participants were equivalent by arm except for gender identity (Table 1). There were 365,346 unique Facebook network members connected to study participants from which the surrogate outcome was measured.
FIGURE 1.
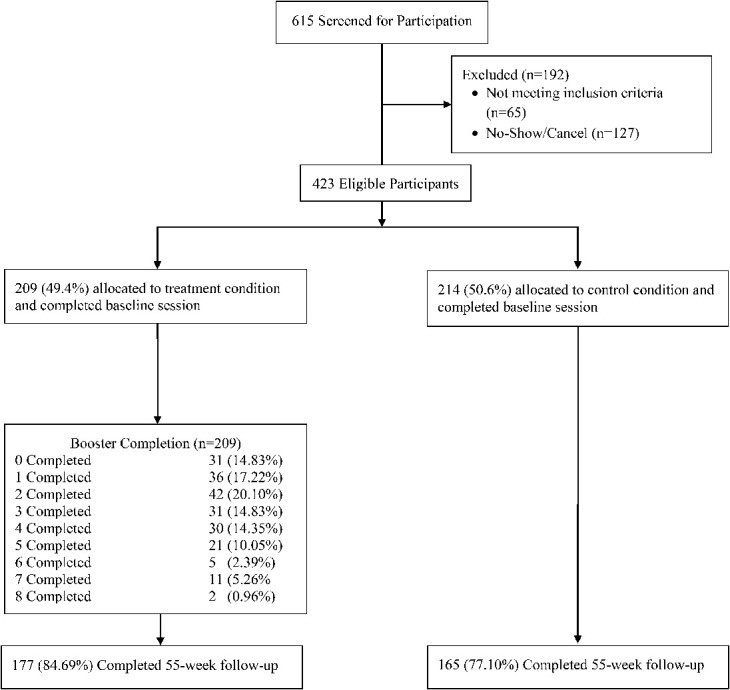
Enrollment and follow-up of study participants before 55-week intervention sequence switch.
TABLE 1.
Baseline Sociodemographic and Behavioral Characteristics Among PrEP Chicago Participants, Chicago, (2016–2018)
| Characteristics | Intervention (%)* (n = 209) | Control (%) (n = 214) | P |
| Age, mean (SD) | 26.1 (4.2) | 25.7 (4.3) | 0.28 |
| Education | 0.17 | ||
| High school or less | 141 (67.5) | 165 (77.1) | |
| Post HS vocational certification | 17 (8.1) | 11 (5.1) | |
| Associate's/Bachelor's/Grad. degree | 43 (20.6) | 29 (13.6) | |
| Employment | 0.31 | ||
| Employed | 109 (52.2) | 92 (43.0) | |
| Not employed | 81 (38.8) | 99 (46.3) | |
| Disabled | 6 (2.9) | 7 (3.3) | |
| Gender identity | 0.043 | ||
| Male | 193 (94.2) | 184 (88.0) | |
| Female/transfeminine | 7 (3.4) | 20 (9.6) | |
| Other | 5 (2.4) | 5 (2.4) | |
| Sexual orientation | |||
| Gay | 135 (64.6) | 123 (57.5) | 0.55 |
| Bisexual | 46 (22.0) | 62 (29.0) | |
| Straight | 5 (2.4) | 8 (3.7) | |
| Other | 11 (5.3) | 10 (4.7) | |
| HIV-Positive | 92 (48.4) | 87 (46.5) | 0.71 |
| Ever heard of PrEP | 0.20 | ||
| No | 50 (23.9) | 66 (30.8) | |
| Yes | 156 (74.7) | 143 (66.8) | |
| Experience taking PrEP | |||
| No | 180 (86.1) | 186 (86.9) | |
| Yes | 20 (9.6) | 20 (9.4) | 0.95 |
| Facebook friends, mean (SD) | 1810 (1394.3) | 1859 (1503.4) | 0.73 |
Temporal Relationship of Intervention and PrEP Referral
Table 2 shows estimates from a mixed-effects negative binomial model fit to the daily number of citywide PrEPline referrals. The number of participants completing an intervention workshop was positively associated with the number of PrEPline referrals, both on the same day and for the next 2 days (by the third day, the effect was no longer evident). Thus, a workshop involving 5 participants translates into approximately one additional PrEPline referral over 3 days, assuming a background referral rate of 5.4 calls per week. By contrast, booster sessions were not associated with an increase in the number of referrals—either on the same day or for the next 3 days (Fig. 2). The purpose of Figure 2 is to demonstrate in the most transparent way possible how the provision of the study intervention (ie, workshops and boosters) was associated with changes over time in the mean number of PreP referrals/care visits.
TABLE 2.
Daily Number of PrEPline Calls on the Number of Intervention Workshops and Boosters, Adjusting for Day of Week and Weekly Variation Over Midpoint 55 Weeks of Follow-up*
| Estimate (95% CI) | P | |
| Daily workshops | ||
| Same day | 0.08 (0.02 to 0.13) | 0.009 |
| 1 day lag | 0.10 (0.04 to 0.15) | 0.001 |
| 2 day lag | 0.06 (0.00 to 0.12) | 0.044 |
| 3 day lag | 0.01 (−0.05 to 0.08) | 0.663 |
| Daily boosters | ||
| Same day | −0.07 (−0.14 to 0.00) | 0.054 |
| 1 day lag | 0.05 (−0.03 to 0.13) | 0.251 |
| 2 day lag | −0.01 (−0.07 to 0.05) | 0.719 |
| 3 day lag | 0.00 (−0.10 to 0.11) | 0.953 |
| Day of week (vs. Monday–Friday) | ||
| Saturday | −1.80 (−2.55 to −1.05) | <0.001 |
| Sunday | −2.50 (−3.53 to −1.46) | <0.001 |
| Constant | −0.14 (−0.38 to 0.10) | 0.249 |
| Log (α) | −1.43 (−2.34 to −0.52) | |
| σ† | 0.24 (0.09 to 0.64) |
Negative binomial mixed-effects regression models.
SD of the week-specific random effects.
FIGURE 2.
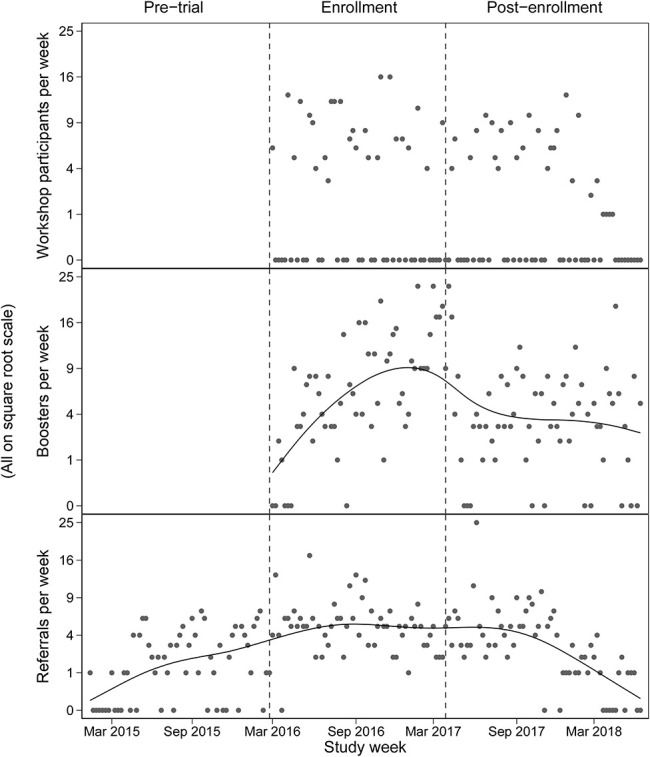
Number of participants completing an intervention workshop per week (Top); number of men completing a booster per week, with penalized spline smoother (Middle); weekly number of PrEPline referrals, with penalized spline smoother (Bottom).
Intervention Effect on PrEP Referrals and Appointments
Over 55 weeks, 15 network members referred from the PrEPline and 50 with a PrEP referral or care visit were identified as having a network tie to at least one study participant who had been recruited before the PrEP referral/visit (ie, they were “Facebook friends”). Two-hundred and sixteen participants (119 intervention and 97 control) were tied to at least one PrEP engaged individual; these participants had a mean of 2.6 ties, a median of 2, and a range of 1–10. Video 1, Supplemental Digital Content, http://links.lww.com/QAI/B565 is a dynamic network visualization that shows the diffusion of PrEP through this network. Estimates from a conditional logistic regression model fit to the likelihood of network ties between PrEP referrals/clinic visits and each of the study participants recruited before the referral/visit are presented in Table 3. Over a 12-month period, the odds of a tie existing between a referral/PrEP visit and a participant in the intervention group were 50% higher [95% confidence interval (CI): 9% to 106%] than for participants in the control group.
TABLE 3.
Likelihood of a Facebook Tie Between PrEPline Referral or First PrEP Clinic Appointment (n = 65) and Study Participant Over 55 Weeks of Follow-Up
| Covariate | OR* | 95% CI | P | |
| All ties over 12 months | Intervention vs. control | 1.19 | 0.99 to 1.43 | 0.067 |
| Seed vs. recruit | 1.46 | 1.19 to 1.79 | <0.001 | |
| No. of FB friends (thousands) | 1.67 | 1.57 to 1.78 | <0.001 | |
| Ties within 3 months of intervention | Intervention vs. control | 1.50 | 1.09 to 2.06 | 0.012 |
| Seed vs. recruit | 0.71 | 0.46 to 1.11 | 0.133 | |
| No. of FB friends (thousands) | 1.53 | 1.38 to 1.70 | <0.001 |
Conditional logistic regression model.
DISCUSSION
Results from this pragmatic randomized controlled trial at 55 weeks of follow-up demonstrate that the intervention was successful in generating PrEP referrals and linkage to first PrEP appointments. The results are robust with the use of 2 independently collected outcome measures as well as 2 separate analytic approaches to determine intervention effect. The 2 analytic approaches each yield evidence of intervention effectiveness over 55 weeks, an adequate time to examine PrEP linkage to care. When compared to control condition, the intervention yielded greater PrEP referral or first clinic appointment, an effect that was strongest within the first 3 months of the intervention. The analysis of referral timing indicates that unlike the workshops, the boosters did not increase the number of referrals over the next few days, although this does not address the possible value of the boosters in maintaining engagement over a longer period.
The estimated number of PrEPline referrals generated during the days immediately after the workshops likely underestimates the overall effect of the intervention—possibly by a large amount. This is due to the small observation window of less than a week that was required to keep potential effects separate from subsequent week interventions. By adjusting for week-to-week variation in PrEPline referral intensity and the number of workshops/boosters, the referral timing analysis focuses solely on the immediate effects of the intervention components, in an attempt to avoid spurious association due to factors throughout the study period that might have affected both the frequency of referrals or first PrEP appointments and the delivery of the intervention. However, the frequency of PrEPline referrals was higher during the study period than it had been before, and began to decline again once the workshops were nearing completion. Thus, it is likely that participants who received the intervention continued to influence network members throughout the study period. Such episodic influence would be nearly impossible, to measure without a mechanism for tracing the interactions between individual participants and PrEPline clients.
The use of Facebook data to measure social influence within the context of a PrEP intervention is important for pragmatic trials that measure downstream outcomes among individuals not enrolled in a study. However, apart from providing a convenient way to track the effect of the intervention, the Facebook results are also informative about potential mechanisms by which such influence occur. Specifically, they suggest the potential importance of Facebook as a means of communication within this community—one that may have real consequences for health-related behavior, which has also been demonstrated in other Facebook communication interventions.32 Furthermore, Facebook's move into dating services underscores the importance of interventions that include such traditional social media applications. Of course, as with the referral timing analysis, the Facebook results may capture only part of the intervention's overall effect because some referred network members or those making an appointment were not locatable on Facebook, appointments may be made at other clinic contexts, and referrals may be made in social contexts not reflected on Facebook. Despite this, diffusion of PrEP through networks could only be accelerated through both online and offline information and motivation.
There were a few limitations to the study. First, we were unable to observe direct communication and referral of network members for PrEP; however, an alternative explanation for the observed PrEP engagement is not available. Second, we did not measure onward diffusion of PrEP beyond the first-degree network members. Although this is possible and would potentially increase the impact of the PrEPChicago intervention more widely, we do know that secondary and tertiary network diffusion effects are much more limited and likely do not move much beyond the third degree. Finally, it is unclear as to whether why we did not observe an effect from the booster sessions. In addition, to several boosters being inadvertently skipped by study staff, it may be that the impact was lessened as the boosters were uncompensated sessions, which could have potentially contributed to limited participant enthusiasm and overall impact.
Diffusion of behaviors have also been observed for smoking cessation,33 adolescent substance use,34 and other HIV-prevention activities.35–37 The ability to reach larger portions of targeted populations38,39 while also overcoming socially derived barriers such as stigma and discrimination through peer leadership and support makes social network interventions powerful strategies for engaging communities most impacted by HIV in biomedical innovations like PrEP. PrEPChicago is thus one of several low-cost strategies that could be used to address HIV spread locally and regionally, such as in national DHHS ending the epidemic strategies. Given that the most impactful component from the interim analysis presented herein was the in-person group intervention, a single session is thus useful in diffusing innovation and represents a low-cost intervention that is potentially scalable. Final analysis will examine the durability of the intervention over 110 weeks for PrEP linkage as well as explore impact beyond linkage such as important PrEP persistence metrics. Future research should continue to explore how such interventions can be used to help end the domestic HIV epidemic, especially in settings where there is low PrEP awareness and access.
ACKNOWLEDGMENTS
The authors acknowledge the study participants for their engagement in the study and with the PrEP Chicago investigative team. The authors thank the PrEPline staff and the PrEP providers in Chicago for working to provide PrEP care. The authors thank NIAID for supporting this work through R01AI120700.
Footnotes
D.M. and B.H. received funding from The Center for Health Administration Studies at the University of Chicago and the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) Grant Number 5UL1TR002389-02. L.Y. received support from K99 (K99HD094648). All authors received support from R01AI120700.
The authors have no funding or conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
REFERENCES
- 1.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. New Engl J Med. 2010;363:2587–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. New Engl J Med. 2015;373:2237–2246. [DOI] [PubMed] [Google Scholar]
- 3.Hosek SG, Landovitz RJ, Kapogiannis B, et al. Safety and feasibility of antiretroviral preexposure prophylaxis for adolescent men who have sex with men aged 15 to 17 Years in the United States. JAMA Pediatr. 2017;171:1063–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hare B, Coll P, Ruane P. The Phase 3 DISCOVER Study: Daily F/TAF or F/TDF for HIV Preexposure Prophylaxis. 2019. The annual Conference on Retroviruses and Opportunistic Infections (CROI); March 4–7, 2019; Seattle, WA. [Google Scholar]
- 5.Wheeler DP, Fields SD, Beauchamp G, et al. Pre-exposure prophylaxis initiation and adherence among Black men who have sex with men (MSM) in three US cities: results from the HPTN 073 study. J Int AIDS Soc. 2019;22:e25223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelley CF, Kahle E, Siegler A, et al. Applying a PrEP continuum of care for men who have sex with men in atlanta, Georgia. Clin Infect Dis. 2015;61:1590–1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rusie LK, Orengo C, Burrell D, et al. Preexposure prophylaxis initiation and retention in care over 5 years, 2012–2017: are quarterly visits too much? Clin Infect Dis. 2018;67:283–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khanna AS, Michaels S, Skaathun B, et al. Preexposure prophylaxis Awareness and use in a population-based sample of young Black men who have sex with men. JAMA Intern Med. 2016;176:136–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hess KL, Hu X, Lansky A, et al. Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol. 2017;27:238–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McNulty M, Smith JD, Villamar J, et al. Implementation research methodologies for achieving scientific equity and health equity. Ethn Dis. 2019;29:83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rogers EM. Diffusion of Innovations. New York, NY: Simon and Schuster; 2010. [Google Scholar]
- 12.Rogers EM, Kincaid DL. Communication Networks: Toward a New Paradigm for Research. New York, NY: Free Press, 1981. [Google Scholar]
- 13.Freedman R, Chow LP, Hermalin A, et al. The family planning program for all of Taiwan. Stud Fam Plann; 1969;44;8–15. [Google Scholar]
- 14.Iyengar R, Bulte CVd, Valente TW. Opinion leadership and social contagion in new product diffusion. Marketing Sci. 2011;30:195–212. [Google Scholar]
- 15.Valente TW. Network interventions. Science. 2012;337:49. [DOI] [PubMed] [Google Scholar]
- 16.Piatt GA, Rodgers EA, Xue L, et al. Integration and utilization of peer leaders for diabetes self-management support: results from project SEED (support, education, and evaluation in diabetes). Diabetes Edu. 2018;44:373–382. [DOI] [PubMed] [Google Scholar]
- 17.Wyman PA, Brown CH, LoMurray M, et al. An outcome evaluation of the Sources of Strength suicide prevention program delivered by adolescent peer leaders in high schools. Am J Public Health. 2010;100:1653–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soumerai SB, McLaughlin TJ, Gurwitz JH, et al. Effect of local medical opinion leaders on quality of care for acute myocardial infarction: a randomized controlled trial. JAMA. 1998;279:1358–1363. [DOI] [PubMed] [Google Scholar]
- 19.Lomas J, Enkin M, Anderson GM, et al. Opinion leaders vs audit and feedback to implement practice guidelines. Delivery after previous cesarean section. JAMA. 1991;265:2202–2207. [PubMed] [Google Scholar]
- 20.What Is Ending the HIV Epidemic: A Plan for America? 2019. Available at: https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview. [Google Scholar]
- 21.Understanding HIV where You Live 2019. Available at: https://aidsvu.org/. Accessed May 1, 2020. [Google Scholar]
- 22.Dehlin JM, Stillwagon R, Pickett J, et al. #PrEP4Love: an evaluation of a sex-positive HIV prevention campaign. JMIR Public Health Surveill. 2019;5:e12822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Young LE, Schumm P, Alon L, et al. PrEP Chicago: a randomized controlled peer change agent intervention to promote the adoption of pre-exposure prophylaxis for HIV prevention among young Black men who have sex with men. Clin trials. 2018;15:44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Soc Probl. 1997;44:174. [Google Scholar]
- 25.Latkin CA, Donnell D, Liu TY, et al. The dynamic relationship between social norms and behaviors: the results of an HIV prevention network intervention for injection drug users. Addiction. 2013;108:934–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mihailovic A, Tobin K, Latkin CA. The influence of a peer-based HIV prevention intervention on conversation about HIV prevention among people who inject drugs in baltimore, Maryland. AIDS Behav. 2015;19:1792–1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lindquist R, Wyman JF, Talley K, et al. Design of control-group conditions in clinical trials of behavioral interventions. J Nurs Scholarsh. 2007;39:214–221. [DOI] [PubMed] [Google Scholar]
- 28.Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA. 2003;290:1624–1632. [DOI] [PubMed] [Google Scholar]
- 29.Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. 3rd ed College Station, TX: Stata Press; 2012. [Google Scholar]
- 30.StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 31.Hosmer DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression. 3rd ed Hoboken, NJ: Wiley; 2013. [Google Scholar]
- 32.Young SD, Cumberland WG, Nianogo R, et al. The HOPE social media intervention for global HIV prevention in Peru: a cluster randomised controlled trial. Lancet HIV. 2015;2:e27–e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. New Engl J Med. 2008;358:2249–2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Valente TW, Gallaher P, Mouttapa M. Using social networks to understand and prevent substance use: a transdisciplinary perspective. Subst Use Misuse. 2004;39:1685–1712. [DOI] [PubMed] [Google Scholar]
- 35.Elford J, Sherr L, Bolding G, et al. Peer-led HIV prevention among gay men in London: process evaluation. AIDS Care. 2002;14:351–360. [DOI] [PubMed] [Google Scholar]
- 36.Kelly JA, St Lawrence JS, Stevenson LY, et al. Community AIDS/HIV risk reduction: the effects of endorsements by popular people in three cities. Am J Public Health. 1992;82:1483–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wohlfeiler D. Community organizing and community building among gay and bisexual men: the STOP AIDS Project. In. Community organizing and community building for health. 1998:230–243. [Google Scholar]
- 38.Ghosh D, Krishnan A, Gibson B, et al. Social network strategies to address HIV prevention and treatment continuum of care among at-risk and HIV-infected substance users: a systematic scoping Review. AIDS Behav. 2017;21:1183–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Latkin CA, Davey-Rothwell MA, Knowlton AR, et al. Social network approaches to recruitment, HIV prevention, medical care, and medication adherence. J Acquir Immune Defic Syndr 2013;63:S54–S8. [DOI] [PMC free article] [PubMed] [Google Scholar]


