Abstract
At the beginning of the SARS-COV-2 outbreak in Brazil, there was a striking difference between the contamination rate in the Amazonian States and the South and the Southeast States. The regions near the Amazon rainforest presented much higher and faster contaminations. This paper attempts to explain this phenomenon through a global analysis of the COVID-19 epidemic in Brazil. It also investigates the relationship between climate conditions and airborne transmission with the evolution of contagion in the Amazonian states. The method of investigation of the spread of SARS-COV-2 in these different macro-environments was based on the analysis of three extensive daily official databases on the number of deaths, the percentage of adherence of the populations to the restriction policies, and the local climatic conditions. Besides, the social conditions in those States were also taken into account. Then, it was compared the epidemiologic results for States with very different climatic characteristics and that had adopted, almost simultaneously, similar social isolation measures. However, all these analyses were not able to explain the remarkable difference in the evolution of the pandemic among Brazilian regions. So, it was necessary to invoke airborne transmission, facilitated by the very high air humidity, as a decisive factor to explain the faster evolution of contagion in the rainforest region. Air humidity seems to be the most important climatic factor in viral spreading, while usual ambient temperatures do not have a strong influence. Another very important result of this analysis was the observation that the onset of collective immunity may have been achieved with a contamination rate of about 15% of the Amazonian population.
Keywords: Covid-19, SARS-COV-2, Airborne transmission, Amazonian rainforest, Climatic conditions
Graphical abstract
1. Introduction
The ray of light that runs through a dark room reveals the existence of numerous small grains of dust that can float in the air for a long time. Since antiquity, this phenomenon was already known. A famous observation of this effect is documented in Lucretius's poem De Rerum Natura, written around 50 BCE. In addition to the empirical description of the phenomenon, and following the tradition of Democritus and Epicurus, Lucretius also proposed an atomistic explanation for the support of particles in the air, according to which their weight would be compensated by the collisions of air atoms (Lucrèce, 2010). However, the behavior of tiny bodies immersed in fluids was only understood from the 19th century on owing to the works of Brown (1828), George Gabriel Stokes, and finally with Einstein's famous work of 1905, On the movement of small particles in suspension within liquids at rest.
Currently, this phenomenon has gained tragic relevance due to the uncontrolled dispersion of the Covid-19 throughout the planet, since airborne transmission is one of the forms of viral contamination, as well as the direct reception of drops exhaled by a contaminated person and the contact with infected surfaces. There is still no consensus among researchers as to which of these forms of contagion is the most important in the case of the coronavirus. Despite being the third outbreak of this virus in less than two decades, existing research had not yet fully understood its transmission mechanisms. A similar situation occurred with the Influenza virus. While some important books and works drew attention to the relevance of the transmission by aerosols (Treanor, 2005; Prather et al., 2020; Morawska and Cao, 2020; Morawska and Milton, 2020), other authors argued that short-distance transmission by drops would be the main means of infection (Bell, 2006; Brankston et al., 2007), and this latter position prevailed for a long time among health authorities who practically ignored airborne transmission (Public Health Agency of Canada Canadian Pandemic Influenza Plan (Appendix F), 2004; U.S. Department of Health and Human Services Pandemic Influenza Plan, 2006). At the end of March 2020, the World Health Organization (WHO) released a bulletin stating that there was insufficient scientific evidence that SARS-COV-2 was significantly airborne transmitted. A few months ago, at the beginning of the current pandemic, several governments and the most important health authorities on the planet recommended that only hand washing and a distance of two meters between people would be safe protection procedures and that the use of masks was unnecessary throughout the population. However, with the rapid spread of the coronavirus in countries and in the world, the deadly reality has imposed itself and forced the health authorities to reverse this directive, saving thousands of lives by requiring the use of masks in several countries. From a scientific point of view, this late change in positioning was the authorities' recognition that air transmission of SARS-COV-2 is an unquestionable fact. Nevertheless, it remains to be understood how this process takes place.
Every global health crisis is a medical, epidemiological, scientific, political, social, and economic event (Bontempi, 2020). Only a multidisciplinary approach can fully understand this planetary event. This article is a contribution to this multidisciplinary scientific effort, discussing one of the most important scientific facets of viral transmission. It will be analyzed the SARS-COV-2 outbreak around the Amazon rainforest that may help to understand the relevance of the long-range viral airborne transmission. Amazonian States have a much higher contamination rate than the Southern and Southeastern States. The study of the Amazon region is particularly interesting because it has very high air humidity that can facilitate the survival of the virus in the external environment.
2. Background
The airborne transmission of the coronavirus is now experimentally well demonstrated by important works published during the last months. A relevant study issued in the journal Nature revealed the existence of the RNA of the SARS-COV-2 in aerosols collected from the air of several closed environments and open places of two hospitals in Wuhan dedicated only to patients infected with Covid-19 (Liu et al., 2020). Another paper analyzed the air at the Nebraska Hospital Center and also found the SARS-COV-2 in most environments occupied by patients with mild and moderate infections (Santarpia et al., 2020). In these two studies it was not possible to confirm if these viruses were active. However, this doubt was finally resolved by a study published in the New England Journal of Medicine, where the presence of active SARS-COV-2 in droplets was observed more than 3 h after they were artificially produced in the laboratory (65% of relative humidity and temperatures between 21 and 23 °C) (van Doremalen et al., 2020). Now, it is certain that under normal day-to-day conditions SARS-COV-2 remains active for hours in the droplets suspended in the air. Extensive study published in The Lancet journal, analyzing empirical data from 16 countries on six continents, concluded that the probability of infection by SARS-CoV-2 decreases by 10,6% when using a protection for the eyes (Chu et al., 2020). That is, the risk of contagion through the eyes is very high and continues to be minimized by health authorities, including the WHO, as had happened in the case of masks. This may be a new mistake in combating the pandemic.
On the other hand, further experiments visualized the production of saliva droplets during a person's normal speech, breathing, sneeze and cough (Anfinrud and Bax, 2020; Stadnytskyi et al., 2020; Nicas et al., 2005). Thousands of drops were exhaled and their dispersion in the air was video recorded. They used a laser beam technique of high resolution that was able to identify even submicron droplets. In the video from Kyoto University (Yamakawa et al., n.d.), one can watch the movement of these drops, revealing that while the larger ones fall rapidly and settle on the ground and furniture, there are hundreds of micro droplets that remain suspended in the air several hours after being exhaled. And, most seriously, these small drops disperse rapidly and, a few minutes after their production, occupy the entire environment, covering distances greater than eight meters.
Besides these experiments, there were several empirical situations that put in evidence the dangerousness of the airborne coronavirus infection. Analysis of the most important focus of coronavirus transmission in the 2002–2003 epidemic in Hong Kong, the Amoy Gardens residential complex, demonstrated that a single infected person contaminated, through the ventilation system, more than 300 people living above in the same building. In addition, there are also strong indications that, in the same Amoy Gardens, contaminated droplets could have been carried by the wind for several tens of meters and have infected people in another building, far from patient zero (McKinney et al., 2006). Also, during the coronavirus (MERS-COV) epidemic in South Korea in 2015, research conducted in two hospitals that were sources of contamination revealed that transmission through ambient air may have been one of the main means of contagion (Kim et al., 2016). Concerning the current outbreak, a recent study demonstrated that the likely onset of the COVID-19 pandemic in Guangzhou, China, occurred by airborne transmission in a restaurant, where the air conditioning system played a decisive role in the spread of viruses exhaled by an infected man who had just arrived from Wuhan (Lu et al., 2020). In addition, mass contaminations provoked by only one contaminated person were recently observed in a choral at Los Angeles and a religious cult in France. Finally, a very recent work claims to have elucidated the intricate transmission pathways of the new coronavirus and sustains “that the airborne transmission route is highly virulent and dominant for the spread of COVID-19” (Zhang et al., 2020).
3. SARS-COV-2 outbreak in the Amazon rainforest
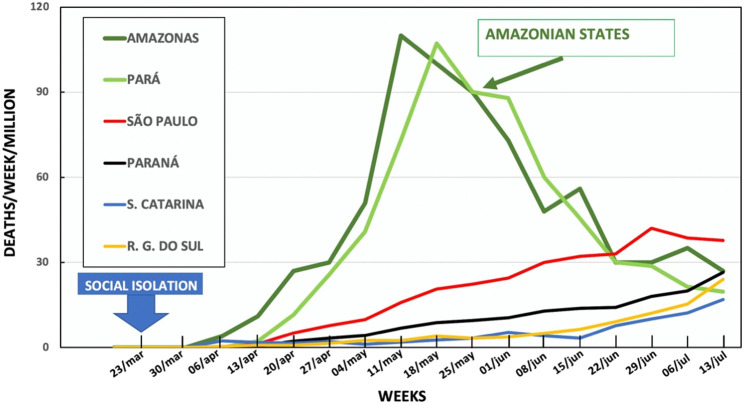
Another new and very relevant epidemiological event has occurred in the current COVID-19 pandemic in Brazil: the Amazonian States that house the forest have presented contamination rates higher than 15%, while in southern States this rate has been less than 1%. To understand this striking difference, this work analyzed the official primary data on the pandemic released daily by all States of the country. The number of deaths was used as an analysis parameter because there is a huge underestimation of the number of cases of the disease due to the extremely low number of tests performed by the Brazilian government. It should be kept in mind that the number of deaths is also undervalued. One of the results of this analysis is represented in Fig. 1 that compares the official number of deaths per week and per million inhabitants between the main Amazonian States and the Southern States of Brazil, and shows a tragic consequence of the great difference in the contamination rates. The blue arrow in the figure represents the moment of adoption of measures of social isolation by the States.
Fig. 1.
Official number of deaths per week and per million inhabitants during the current SARS-COV-2 epidemic in two Amazonian States and some southern States of Brazil. The large blue arrow indicates the weeks of implementation of social isolation by the States. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
(Source of primary data: State Health Departments)
3.1. Collective immunity
Fig. 1 reveals that near the forest the number of deaths has grown quickly but had also a sharp decrease, while the southern States showed much slower growth. The number of confirmed cases has similar behavior. It is important to emphasize that no additional measures of social isolation were taken after the first week indicated in Fig. 1. The evolution of the epidemic in the Amazonian States indicates an extremely important epidemiological result, because the sharp decrease of deaths after reaching the peak was probably due to the large contamination attained in the population. It is surprising that this apparent onset of collective immunity may have been achieved with a much lower percentage of population contamination than predicted by conventional statistical calculations. The actual contamination rate is very difficult to be calculated in Brazil due to the minor number of tests performed. However, extensive serological research conducted by several Brazilian universities calculated that in the State capitals of Amazonas and Pará, during the month of May, the percentage of infected persons was 13% and 15%, respectively. In other cities near the rainforest this percentage attained 20% to 25% (Candido et al., 2020). Therefore, the contamination rate that could have produced the interruption of the spread of the epidemic observed in Fig. 1 was only of the order of 15%. If confirmed by further studies, this result could be very useful in combating the pandemic.
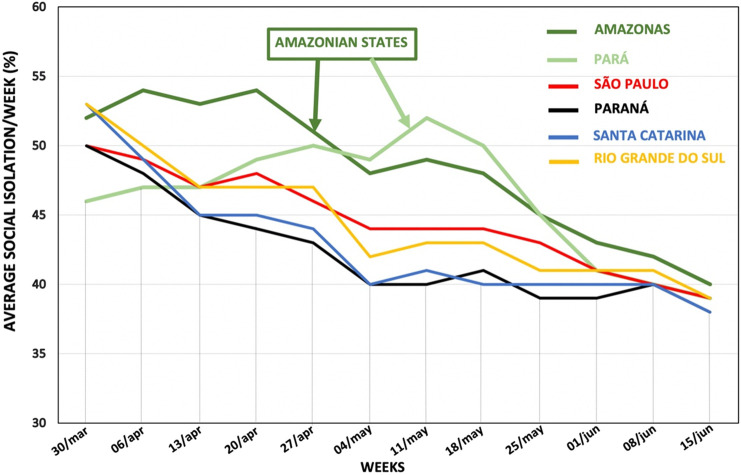
3.2. Social mobility
The striking difference observed between the North and South regions could not be explained by the issue of social isolation measures, since both adopted, almost simultaneously, similar isolation measures. However, a determining factor in viral dissemination is the degree of adherence of the population to the measures adopted. To investigate this factor, it was analyzed daily geo-localized mobile phone data that evaluate social mobility (Inloco Agency, 2020). Fig. 2 shows the result of the average social isolation, per week, calculated in the period investigated in this paper. As can be seen in this figure, during the pandemic in Brazil there was no true social isolation, and the result was the very high number of deaths. The main cause of this dramatic result was the denialist stance of the federal government. Fig. 2 also shows that the population of the Amazonian States presented lower social mobility than the other states in almost the entire period investigated. Therefore, social mobility should not be responsible for the difference in the number of deaths observed between Brazilian. Another important result that can be extracted from Fig. 2 is that the sudden decrease in the number of deaths observed in the Amazonian States since May 11 (see Fig. 1) cannot be attributed to a previous increase in social confinement.
Fig. 2.
Average social isolation per week for in two states located in the Amazon rainforest and in four southern and southeastern Brazilian States. The calculation used evaluations of geo-localized mobile phone data.
Primary data source: Inloco Agency (Candido et al., 2020).
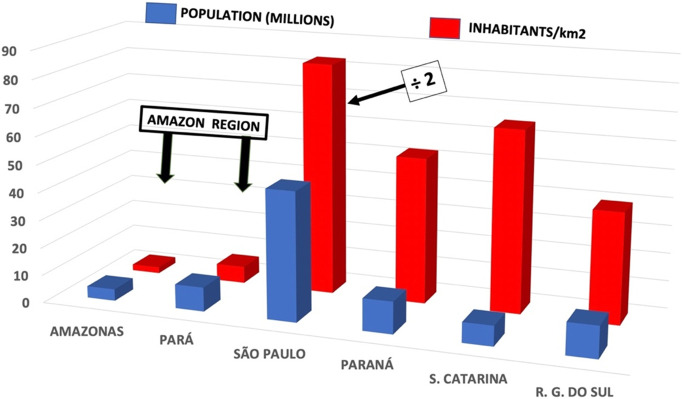
3.3. Social conditions
Other possible explanation for a rapid evolution of the epidemic would be a high population concentration. Fig. 3 shows the number of inhabitants and population density in the States under investigation (Instituto Brasileiro de Geografia e Estatística (IBGE), 2020). As it can be seen, the States in the Amazon region, Amazonas and Pará, have a smaller population and much lower population density (inhabitants/km2) than the Southern and Southeastern States. Therefore, from this point of view, one would expect contamination to be faster in states with higher population density, contrary to what happened.
Fig. 3.
Population, in millions of inhabitants, and population densities, in inhabitants per km2, of Brazilian States under investigation.
Source of primary data: IBGE – Instituto Brasileiro de Geografia e Estatística (Inloco Agency, 2020).
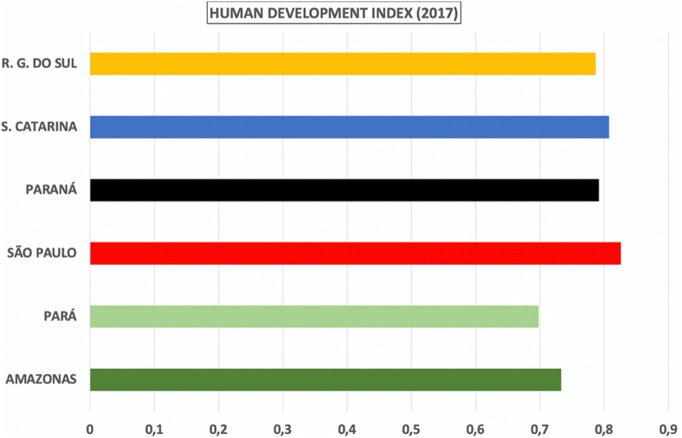
On the other hand, it could be argued that the worst average social conditions in the Northern region of the country would explain the rapid progression of contamination in those States. However, comparing the Human Development Index (HDI) of these states shown in Fig. 4 , it can be seen that the average difference is less than 10% (Instituto Brasileiro de Geografia e Estatística (IBGE), 2020). In addition, the large cities in the South and Southeast regions have thousands of slums where the inhabitants live very concentrated in precarious dwellings. The HDI in these neighborhoods are equal to or lower than the Northern States. Therefore, the striking difference in the evolution of the epidemic observed between the North and South regions cannot be explained by social factors. A possible difference in health care system between regions could also not be claimed as an explanation of this phenomenon, as it would not justify the sudden decrease in the number of deaths observed in Fig. 1. So, the remarkable disparity in the evolution of the contamination in these regions needs to be deeply investigated.
Fig. 4.
The Human Development Index of the Brazilian States under investigation.
Source of primary data: Instituto Brasileiro de Geografia e Estatística (IBGE).
3.4. Climate influence
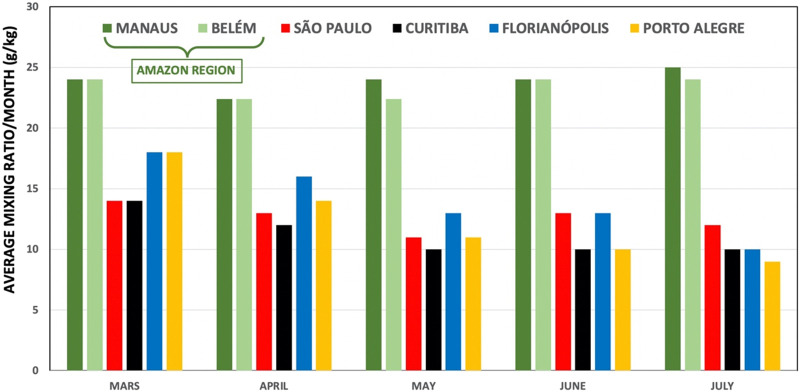
A factor that can play an important role in the spread of SARS-COV-2 is the climate. During the months investigated in this work, in the regions surrounding the forest, the average temperatures were always above 30 °C and the average relative humidity, above 80%. In southern States, average temperatures and average relative humidity were not higher than 22 °C and 50%, respectively. Therefore, there is no direct relationship between high ambient temperature and decreased transmissibility. On the other hand, some studies showed that, in general, in environments with relative humidity above 60%, approximately, the drops absorb more than evaporate water into the air (Marr et al., 2019; Shaman and Kohn, 2009). So, one can suppose that the airborne transmission of the SARS-COV-2, facilitated by the high humidity of the air, could be a primary factor in the development of the epidemic in Brazil. This hypothesis is confirmed by other studies conducted in some cities in Brazil at the beginning of the pandemic, although these studies use the number of cases as an analysis variable (Euler et al., 2020; Sobral et al., 2020). To better understand this relationship, it is interesting to know the amount of water vapor that actually exists in the atmosphere, that is, its absolute humidity. One kilo of air with relative humidity 70%, at 30 °C, contains approximately 19 g of water in the form of vapor, while at a relative humidity of 40%, at 22 °C, the amount of water is only 6 g.
Fig. 5 compares the average monthly value of the amount of water vapor contained in a kilo of air (average mixing ratio) in the capitals of the States under investigation (Instituto Nacional de Meteorologia (INMET). Ministério da Agricultura, Pecuária e Abastecimento, 2020). The weekly average values of this variable show the same behavior. Manaus and Belém, the capitals in the Amazon rainforest region, have almost twice as much water in the air compared to the Southern capitals. That is, the process of water evaporation/absorption is very complex in the Amazonian weather conditions, and, on average, the drops expelled by an infected person will absorb water from the atmosphere, allowing the viruses to survive much longer in suspension or deposited on surfaces. These processes may have facilitated the rapid transmission of the virus observed in the Amazon and Pará.
Fig. 5.
Average mixing ratio, in g/kg. Average monthly amount of water vapor per kilo of air from the capitals of the States investigated.
Source of primary data: Instituto Nacional de Meteorologia (INMET)
A similar situation has occurred in abattoirs in France, Germany, and the USA that have become huge poles of contamination. The dominant explanation for this phenomenon has been the airborne transmission facilitated by the low temperature of these environments. However, the pandemic evolution in Brazil, Middle East, Europe, China, and USA has demonstrated that habitual temperatures seem to have little influence on the survival of the virus in the external environment. Therefore, as in the Amazonian case, one can suppose that also in the abattoirs the most important factor was the very high humidity of the air needed in these environments. These examples confirm old and classical work that showed the existence of a very complex relationship between coronavirus survival and air temperature and humidity (Ijaz et al., 1985).
4. Conclusions
The very high SARS-COV-2 transmission rates in Amazonian States in Brazil and many abattoirs around the world provide empirical corroboration of the relevance of the airborne way of contagion. These two environments have high air humidity that allows viruses to survive much longer in droplets in suspension or deposited on surfaces. Therefore, air humidity seems to be the major climatic factor in the development of the COVID-19 epidemic. On the other hand, apparently, there is no direct relationship between high ambient temperature and decreased transmissibility. Besides, the onset of collective immunity in Amazonian States may have been achieved with a contamination rate of around 15% of the population, much lower than predict conventional statistical studies. If corroborated by other research, this result will have an important impact on the management of the pandemic.
CRediT authorship contribution statement
This paper was conceived and written by only one author.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Editor: Jay Gan
References
- Anfinrud P., Bax C. A Bax. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2007800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell D.M. WHO Writing Group: nonpharmaceutical interventions for pandemic influenza, international measures. Emerg. Infect. Dis. 2006;12:81–87. doi: 10.3201/eid1201.051370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E. Commercial exchanges instead of air pollution as possible origin of COVID-19 initial diffusion phase in Italy: more efforts are necessary to address interdisciplinary research. Environ. Res. 2020;188:109775. doi: 10.1016/j.envres.2020.109775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brankston G., et al. Transmission of influenza A in human beings. Lancet. 2007;7:257–265. doi: 10.1016/S1473-3099(07)70029-4. [DOI] [PubMed] [Google Scholar]
- Brown R. Edinb. New Philos. J. 1828:358–371. [Google Scholar]
- Candido D.S., et al. EPICOVID19. 2020. https://bit.ly/Epicovid19BRfases1-3
- Chu D.K., et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19. Lancet. 2020 doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New Engl. J. Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Euler A.C., et al. Evidence that high temperatures and intermediate relative humidity might favor the spread of COVID-19 in tropical climate: A case study for the most affected Brazilian cities. Sci. Total Environ. 2020:729. doi: 10.1016/j.scitotenv.2020.139090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ijaz M.K., et al. Survival characteristics of airborne human coronavirus 229E. J. Gen. Virol. 1985 doi: 10.1099/0022-1317-66-12-2743. [DOI] [PubMed] [Google Scholar]
- Inloco Agency 2020. http://inloco.com.br
- Instituto Brasileiro de Geografia e Estatística (IBGE) 2020. http://ibge.gov.br
- Instituto Nacional de Meteorologia (INMET). Ministério da Agricultura, Pecuária e Abastecimento 2020. http://portal.inmet.gov.br
- Kim S.H., et al. Extensive viable Middle East respiratory syndrome (MERS) coronavirus contamination in air and surrounding environment in MERS isolation wards. Clin. Infect. Dis. 2016;63:363–369. doi: 10.1093/cid/ciw239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020 doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- Lu J., et al. COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerg. Infect. Dis. 2020;26 doi: 10.3201/eid2611.203774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucrèce . Éditions Gallimard, Essais Folio; Paris: 2010. La Nature des choses. [Google Scholar]
- Marr L.C., et al. Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. J. R. Soc. Interface. 2019;16:20180298. doi: 10.1098/rsif.2018.0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinney K.R., et al. Environmental transmission of SARS at Amoy gardens. J. Environ. Health. 2006;68:26–30. [PubMed] [Google Scholar]
- Morawska L., Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ. Int. 2020;139:105730. doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Milton D.K. It is time to address airborne transmission of COVID-19. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicas M., et al. Toward understanding the risk of secondary airborne infection: emission of respirable pathogens. J. Occup. Environ. Hyg. 2005;2:143–154. doi: 10.1080/15459620590918466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prather K.A., et al. Science. 2020 doi: 10.1126/science.abc6197. [DOI] [Google Scholar]
- Public Health Agency of Canada Canadian Pandemic Influenza Plan (Appendix F) 2004. http://www.phac-aspc.gc.ca/cpip-pclcpi/pdf-cpip-03/cpip-appendix-f.pdf
- Santarpia J.L., et al. 2020. medRxiv. [DOI] [Google Scholar]
- Shaman J., Kohn M. Absolute humidity modulates influenza survival, transmission, and seasonality. PNAS. 2009;106:3243. doi: 10.1073/pnas.0806852106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobral M.F.F., et al. Association between climate variables and global transmission of SARS-CoV-2. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138997. (doi:10.1016%2Fj.scitotenv.2020.138997) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stadnytskyi V., et al. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. PNAS. 2020 doi: 10.1073/pnas.2006874117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treanor J.J. Douglas and Bennett’s Principles and Practice of Infectious Diseases. Elsevier Churchill Livingstone; 2005. Influenza virus; pp. 2060–2085. [Google Scholar]
- U.S. Department of Health and Human Services Pandemic Influenza Plan 2006. http://www.hhs.gov/pandemicflu/plan/
- M. Yamakawa et al, Kyoto University, https://vimeo.com/402577241
- Zhang R., et al. Identifying airborne transmission as the dominant route for the spread of COVID-19. PNAS. 2020;117(26):14857–14863. doi: 10.1073/pnas.2009637117. [DOI] [PMC free article] [PubMed] [Google Scholar]