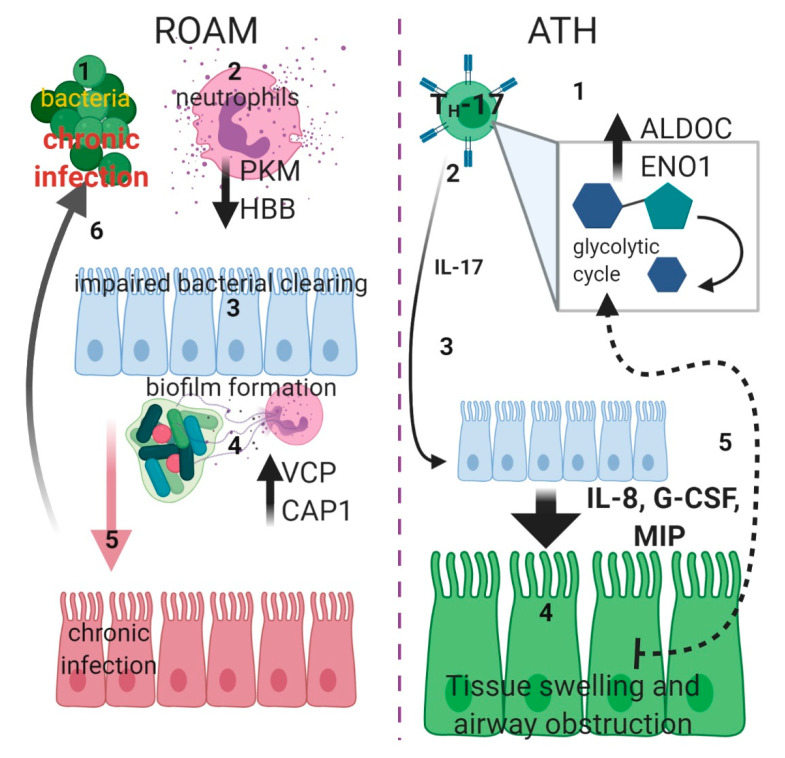
Figure 7.
Schematic diagram displaying putative pathogenic mechanisms In ROAM (left side): bacterial infections (1) triggers neutrophils degranulation (2), but this is not effective due to lower PKM and HBB levels (black arrow downwards). Defective bacterial clearing (3) causes chronic infection (through formation of biofilm) in the median ear, with a consequent increase of NETs formation (4), due to higher proteasome activity provoked by increased VCP and CAP1 levels (black arrow upwards). Chronic bacterial infection of ear tissue (5) (red) establishes a milieu in which recurrent infections (6) are facilitated. In ATH (right side), TH-17 cells are activated (1) and switch to glycolytic metabolism (gray square), with increased levels of ALDOC and ENO1 (black arrow upwards). Activation of these cells causes increasing Interleukin-17 (IL-17) (2) production. This cytokine (3) could drive epithelial expression of granulopoietic and chemotactic factors such as Interleukin-8 (IL-8), Granulocyte Colony-Stimulating Factor (G-CSF) and Macrophage Inflammatory Proteins (MIP) (big arrow downwards) that could induce swelling of adenoidal tissue (4) (green), followed by upper airway obstruction. The imperfect oxygen intake could then trigger a self-sustained cycle (5) (dotted arrow), inducing furthermore a switch toward glycolytic metabolism (created with BioRender.com).