Abstract
This review explores the evolutionary interaction and co-development between immune system and somatic evolution. Over immense durations, continuous interactions between microbes, aberrant somatic cells, including malignant cells, and the immune system have successively shaped the evolutionary development of the immune system, somatic cells and microorganisms through continuous adaptive symbiotic processes of progressive immunological and somatic change providing what we observe today. The immune system is powerful enough to remove cancer and induce long-term cures. Our knowledge of how this occurs is just emerging. It is less clear why the immune system would detect cancer cells, when it is usually focused on combatting infection. Here we show the connections between immunity, infection and cancer, by searching back in time hundreds of millions of years and more to when multi-cellular organisms first began, and the immune system eventually evolved into the truly brilliant and efficient protective mechanism, the importance of which we are just beginning to now understand. What we do know is that comprehending these points will likely lead to more effective cancer therapies.
Keywords: Immune system, evolution, cancer, mutation, immune response, immunosurveillance, immunotherapy
Introduction and overview
It often goes unappreciated that the adaptive immune system developed hundreds of millions of years ago, and has evolved into a truly efficient protective mechanism, the importance of which we are just beginning to now understand in science and medicine. Acute immune responses have developed alongside infection and genetic diversity, as part of the entire evolutionary process of matching organism against organism. There has been a continuous development of the immune system's capacity to protect an organism against infections through rapid genetic somatic hypermutations that also lead to a dynamic, intricate interplay between genetic endowment and somatic mutations. The immune system acts as an ultimate high fidelity 'read-out' for cellular genetic change, detecting cellular aberration at very early stages as it develops, to remove or destroy aberrant cells. Such aberration arises from infection of cells by viruses, bacteria or other microbes, DNA damage, failed repair mechanisms, mutagens, and carcinogens including UV light, toxins and chemicals, and cellular ageing. Constant dynamic interaction occurs between cells and the immune system to preserve homeostasis. Because the rate of mutation during cell division and tissue turnover far exceeds the rate of malignant tumour diagnosis, the immune system must play an efficient role in detecting and eliminating aberrant and frankly malignant cells at a developmentally early stage. The reason why cancer occurs at all in humans and animals thus remains a mystery. However, the answer likely resides with observations that in the chronic state of antigen persistence the immune system continually appears to close itself down to avoid over-activation and to conserve energy. In the acute state, with exposure to each new pathogen the immune system responds rapidly over several days and then typically retains 'memory' of that encounter, enabling more rapid responses upon subsequent exposure. If the antigen can be acutely removed from the system, the immune system returns to steady basal state via homeostatic mechanisms. However, if the antigen persists and cannot be removed from the organism, the immune system responds again with a further cycle of activity. Over-reactivity is limited by eliciting an inhibitory response after each activation response, in the form of negative feedback for biological homeostatic damping. This cyclic feedback phenomenon is seen right across many, if not all, biological systems in nature. In the chronic state, the immune system repeatedly activates in response to persistent antigenic signals. When the antigenic signal cannot be removed with a second 'round' of activation, another cycle of activation and then inhibition occurs. This repetitive cycle continues until the antigenic focus is eventually removed, or the organism dies. Although this is an efficient system in the acute setting, in the chronic setting where the problem persists indefinitely and does not appear to resolve, 'chronic inflammation' can arise which is often far less energy efficient. Vast amounts of energy can be consumed in chronic severe inflammatory conditions. In areas of the world where infection has been effectively reduced by sanitation and other public health measures, chronic inflammatory diseases have emerged as the major causes of morbidity and mortality. Clinically, this manifests as a relapsing and remitting process, often with malaise and weight loss characteristic of many chronic illnesses. This rather maladaptive process consumes massive amounts of energy, damaging surrounding tissues and cells. Over a number of generations, natural selection can lead to efficiency improvements of immune responses to specific chronic infections through co-adaptation of hosts and pathogens; examples are endemic treponematoses 1, 2 or tuberculosis 3, 4.
This article considers cancer immunology in terms of immune system evolution and chronic inflammation.
Review
Developmental importance, genome diversity and evolutionary change
The immune system functions diversely across many organs to protect and maintain health. Importantly, the host’s immune system can regulate the genomic integrity across species and generations. Protection extends to all body barrier interfaces between the external and internal environment, where invasion of microbial agents is prevented or dealt with. The protection also acts against deleterious somatic mutations of host cells. The immune system is vital for maintenance of the health of all other body systems.
Essentially, the process of DNA-based evolution, besides adapting organisms to their physical environments, has pitted organism against organism in the quest for ultimate survival. According to Darwinian principles, the surviving organisms are the most successful either in conquering and terminating competing organisms, or in reaching symbiotic balance with them. That process requires protection of host DNA and also facilitates relatively rapid genomic constitutional adaptation by acquiring and modifying useful DNA from the environment 5. Indeed, the organism’s DNA is added to, modified and diversified to keep ahead of the ‘genetic superiority game’ by mutation, plasmid transfer, viral transduction, mitotic translocations, and meiotic acquisition. The immune system undergoes constant modification of innate and adaptive immunity with exposure to antigenic stimuli both at the individual and the population levels.
The mammalian immune system represents one of the final central arbiters over the course of human Darwinian evolution. Many of the advances necessary for human adaptation have been moderated, directed and shaped by the influence of the immune system. Most fundamentally, the defense against infection and therefore survival of individuals to permit reproduction and species continuity, is underpinned by immune system function. Less obvious, though equally fundamental, is the role of the immune system in maintenance of the organism’s homeostasis through removal of cells whose somatic mutations made them deleterious. Natural selection applies not only to the successful reproduction of entire organisms, but also to the clonal reproduction of cell lineages, both cancer and immunological, within an organism 6.
The genes for the hypervariable regions of the antibody molecule and the genes for the hypervariable regions of the T-cell receptor, mutate at a much faster rate (hypermutation) than somatic genes under usual environmental pressure. Somatic mutation is a relatively slow process where genetic changes through selection pressure on survival and evolution usually require generations of cell divisions. The immune system genes, however, constantly rapidly mutate in order to generate diverse conformations capable of binding the multitude of antigens to which an individual is exposed. Many of those antigens might be associated with threat and danger, for example, from microbial invasion. The immune system design has necessarily evolved, through continuous successive approximation, to detect subtle molecular cell surface aberrations. This occurs through both non-specific, and specific B- and T-cell, mechanisms in an elegantly integrated manner.
How the genome monitors itself and evolves
Somatic changes of organisms occur generally at a gradual pace as part of the slow, but effective, evolutionary process through such mechanisms as random mutation, natural selection and viral infection. For example human morphological characteristics, such as stature, brain size and tooth size change at rates ranging from 0.3 darwins to 65 darwins 7. Microbial DNA sequences, for example from retroviruses like HIV, Herpes viruses and Mycobacterium tuberculosis, have been identified in the human genome, and these genes must have been structurally incorporated over time from repeated exposure, interaction and exchange between mammalian and microbial DNA 8, 9. Human Endogenous Retroviruses (HERVs) are estimated to make up 8% of the human genome, though fragmented and replication incompetent, it bears testament to long and intimate genetic interactions between a parasite with a few genes and 10,000 nucleotides, and a host of some 22,000 genes and some 2.85 billion nucleotides 10, 11. Interestingly, the (uninfected) C57 black mouse has several whole genomic copies of the LMP56 retrovirus in its germline 12. Clearly, the retrovirus became inserted into the murine genetic complement in the mammal's evolutionary past 13– 15. When infected with the virus in the experimental situation, the mouse develops a chronic immunodeficiency disease, the clinical course of which parallels HIV/AIDS in humans 16. It is now suggested that this chronic disease state is due to the murine immune system failing to differentiate between self and non-self, such that it homeostatically attenuates or down-regulates the response against the virus in vivo 17, 18. Failure to resolve the disease is due to persisting viral (self) antigens. The experimental similarity to the immune response in murine cancer models is strikingly compelling. In the case of cancer in the mouse the persisting antigens are due to the growing cancer which appears to exert a similar attenuating effect 19.
Over the millennia the constant exchange of genetic material between host and environmental microorganisms has offered incremental adaptive advantage to both organisms, but in fundamentally different ways, perhaps comprising the ultimate symbiotic relationship, since both have evolved and survived 20. However, many organisms can expand rapidly, possess mechanisms for evasion of host defences, and can mutate at a rate that far outpaces somatic evolutionary change via much faster division/reproduction rates. This may explain the immune system’s evolved ability to match these rapid microbial mutational rates to more effectively neutralize them via innate mechanisms, antibody production and cellular responses. Examples are the microorganisms that rapidly expand and produce outbreaks of disease in humans, animals, plants and insects, sometimes with transmission across species. Rapid, immediate 'revolutionary' adaptive change is advantageous to keep the immune system ahead of microbial mutation, virulence and growth 21. To oppose mutated, infected and otherwise aberrant cells, the immune system has a number of adaptive and protective mechanisms. These include somatic hypermutation genes for generation of hypervariable region binding domains for antibody molecules by plasma (B-) cells, and for hypervariable T-cell surface receptors by T-cells for rapid response to antigen exposure. In this way, adaptive immune responses can rapidly generate multiple molecules with variable affinity for binding whole or fragmented antigens. An analogy would be 'random number generation' to break unknown digital codes, or in contemporary terms to 'hack into' a computer system across encrypted firewalls 22– 24.
Without adequate host organism defence, infection would cause cellular damage and death. Humans are estimated to harbour some 10 14 microbes, mostly bacteria, while we consist of only 10 13 mammalian cells 25– 27. It might therefore be argued that in a cellular sense we are more bacterial than mammalian in constitution. Let's however, adhere to the notion that the host is the mammalian component. The human body, like any other multicellular organism, should be treated as a complex ecosystem whose balance is dynamically maintained by feedback interactions amongst its parts.
To understand the human immune system, we must appreciate that each facet of the immune system has evolved concurrently as life itself has evolved. The mammalian genome, therefore constantly monitors itself through the actions of the immune system, both non-specific and adaptive. This is in order to achieve a state of evolving homeostasis to achieve progressive protection of the genome, and of cellular and tissue function, as the environmental, microbial and other pressures continually change.
History of immune system development and cellular aberration
Life on earth commenced between 3 and 4 Ga (giga/billion years ago) as unicellular organisms adapted to survive environmental hazards through rapid reproduction and repopulation. Some 1.2 Ga algal mats developed as the first multicellular organisms, and then about 1 Ga more complex chlorophyll-containing organisms evolved. About 450 Ma (mega/million years ago) even more complex plants developed and acquired fundamental innate static immune systems largely through intracellular anti-microbial molecules to resist infection principally from fungi, bacteria and viruses.
Adaptive immunity developed rather precipitously around 450 Ma in primitive fish and amphibians, and with reptiles, about 300 Ma, this evolved rapidly for protection against infection.
Mammalian life began about 120 Ma, with immune system evolution to meet the need for local and systemic protection from invasive microorganisms, and placentation 20. Indeed, for effective adaptive symbiosis the mammalian immune system must have developed evolutionary tolerance for specific microorganisms since some organisms conferred adaptive advantages and others did not.
Over a mere 60 years or so, we have investigated the intricate interplay between non-specific (innate) and more specific (adaptive) immune mechanisms for fundamental evolutionary and developmental advantage. Often viewed as separate arms of the immune response, it is clear that they are rarely mutually exclusive or separate. The division arose for experimental explanatory research reasons, rather than physiological ones, but are inextricably inseparable.
Genomic intrinsic mutational pressures and exogenous infection of cells are significant forces capable of exerting phenotypic change to produce cell membrane 'aberration'. During cellular transformation to dysplasia, metaplasia and malignancy, cell membrane changes are detectable. Since gene mutations occur about 1 in every 10 6 cell divisions, the risk of cellular aberration is high in rapidly dividing tissues, with some leading to malignant transformation. The immune system is the only system capable of high level detection and action, and must therefore detect aberrant cells early and remove them exceedingly effectively and efficiently, otherwise, the rates of cancers would exceed that observed clinically. About 10 6 cells form a 5mm diameter tumour from some 30 divisions (assuming a regular process applies).
Fundamental reactivity to aberrant antigens
Aberrations, arising from multiple events such as infection of cells, cellular injury, trauma, ageing or from genetic mutation, are reflected by cell surface expression of aberrant proteins, lipids (especially glycolipids) and carbohydrates. Detection of aberration through both non-specific and specific adaptive mechanisms is essential for destruction and removal of abnormal cells to restore tissue integrity. Membrane profile alterations from normal to dysplastic and malignant transformation are evident using magnetic resonance spectroscopy 28– 30. The immune system is carefully tuned to detect relatively subtle changes in proteins through the standard HLA systems via Class I and II molecules, and the far less explored CD1 system for the detection of lipid, glycolipid and carbohydrate molecules 31. In addition, the Fc receptor mechanism of the non-specific arm of the immune system detects foreign and altered cells. Activation of granulocytes, macrophages, B-cells and T-cells pushes the immune system in one direction or in the other, producing either overall responsiveness/activation, or inhibition/tolerance. Increasingly, it is being appreciated that all levels of the immune system can either respond or inhibit. Therefore, infected, damaged or malignant cells can be either actively eliminated or tolerated. Clinically, this is precisely what is observed, in a variety of infections and malignancies. Indeed, chronic inflammatory states have emerged as the predominant illnesses affecting many individuals, including persistent infections, autoimmunity and malignancy. Diseases such as cancer, cardiovascular disease and diabetes are now appreciated as chronic persistent inflammatory states, capable of modulation by factors such as anti-inflammatory medication and immune modulation.
The cancer cell as an evolutionary entity
Cancer cells are often portrayed as profoundly defective 'rogue' cells. Certain acquired key mutations permit loss of cellular control in division and adhesion, to evade immune destruction. The extent of genetic heterogeneity occurring within the cancer mass(es), both primary and metastatic, appears considerable 32– 36.
Clearly, the cancer cell appears as an adaptive and highly evolved entity able to switch on certain genes to survive the onslaught of radiation and chemotherapy, despite having genetic/chromosomal errors. So, in this sense it is a very sophisticated survival machine. So much so, that a cancer cell is often described as being “immortalized”. For example, the HeLa cell line, from Henrietta Lacks who died of cervical cancer in 1951 has been cultivated for decades in tissue culture worldwide, with some 20 tonnes grown to date 37, 38.
Cancer remains a major protracted health problem globally despite decades of apparent sophisticated research and monies spent, with relatively minor reductions in mortality from advanced cancers of most types 39. Indeed, perhaps the strategies and “paradigms” currently used for cancer research and therapeutic intervention might be incorrect. In 2010, the successes of cancer research efforts were again questioned 40, 41, while in 2008 the USA National Cancer Institute, in frank admission of glacial progress, sought insights from the physical sciences into cancer biology (via 12 new so-called Physical Science-Oncology Centers; PS-OCs), hoping for radically new thinking 42. Novel ideas emerged from the PS-OC programme like the atavistic theory, where cancer is viewed not so much as a “dream run” of genetic accidents conferring extraordinary capabilities, but as a "default state" in reaction to an insult or stress, where cells abandon many recently-evolved capabilities to run on ancient core functionality – a sort of basic “safe mode” for cells. In other words, cancer is an inbuilt response to damage (or poor tissue environments) rather than a product of it 43, 44. Thus rather than cancer being a modern biological phenomenon, it has very deep evolutionary roots - confirmed by the fact that cancer is found across most classes of multicellular life, including simple organisms like hydra that possess only two cell types 45.
Cancer represents a reversion to a more primitive eukaryotic cellular state. In the single-celled world, cells are effectively immortal, and their prime imperative is replication in the face of diverse challenges. Proliferation is thus the default state of unicellular life and it has had 4 billion years to evolve mechanisms to preserve it when threatened. A major transition in biology occurred between about 1.0 and 1.5 billion years ago with the evolution of multicellularity, and later with primitive metazoan multicellularity somewhere in the Cambrian period approximately 550 Ma. In many multicellular organisms somatic cells outsource their immortality to specialized germ cells, and accept apoptosis as the price. However, this ancient contract is vulnerable to 'cheating' (as with all cooperative biological systems) and so it must be policed by layer upon layer of regulatory control. When the control mechanisms are damaged or compromised, reversion to unconstrained proliferation may ensue, manifesting as a neoplasm. Cancer is thus an ever-present threat – an accident waiting to happen – because of “pre-programmed” deeply-entrenched, highly-protected and ancient genome parts which can be variously triggered, including by random damage. Like a genie in a bottle, the bottle can be shattered in many ways, but once the genie escapes it executes its agenda with ruthless efficiency and determinism. Thus cancer follows a broadly predictable pattern of behaviour across organ types and species, with primary tumours followed by EMT, motility, dissemination via the vasculature, colonization of remote organs, MET and secondary growth, suggesting it is a very basic biological phenomenon and not an aberration.
The atavistic theory makes some specific and testable predictions about cancer progression. In defaulting to an ancestral phenotype, cancer is more comfortable in, and may even engineer niches to recreate, conditions resembling the Proterozoic oceans in which multicellularity evolved. For example, the Proterozoic environment at that time was hypoxic (the second great oxygenation event did not take place until about 800 million years ago). Sure enough, cancer metabolism prefers the ancestral, but less energy efficient mechanism of anaerobic fermentation (glycolysis) over the more recently-evolved oxidative phosphorylation. This atavistic reversion to an ancient mode of metabolism is known as the Warburg Effect and has been widely recognized, even if unexplained, since the 1930s 46. Another example concerns the long-recognized resemblance between embryo development and tumours, common features being hypoxia, cell motility (EMT), angiogenesis, invasiveness and rapid proliferation. But ontogeny roughly mimics phylogenetic evolution (von Bauer’s laws of ontogeny), so a reversion to a more primitive evolutionary state closely resembles a reversion to an embryonic developmental state. It is widely known that developmental genes tend to be inappropriately up-regulated in cancer 47, and these are in turn the ancient genes controlling the basic body plan.
In a refinement for the broad-brush (and fairly uncontentious) reversion theory, Lineweaver, Davies and Vincent 44 are examining the evolutionary ages of the genes that are up-regulated in cancer. This emerging field is known as phylostratigraphy. The atavism theory predicts that genes which are up-regulated in cancer (oncogenes) should be systematically older than those that are down-regulated (tumour suppressor genes), and that this skewed distribution should become more pronounced as a function of cancer progression in individual organisms. The theory thus makes a new prediction: that in cancer, there should be a correlation between gene ages and (anomalous) gene activity.
If this general trend towards a more primitive state is correct, it exposes an Achilles Heel of cancer. Reversion involves changes in cell functionality. The atavism theory claims that the gain of function in cancer is really regain of pre-existing ancient functionality. In contrast to the standard somatic mutation theory of cancer, in which neoplasms are treated as if created anew in each organism (and acquire their astonishing similarity via high-speed convergent evolution within the organism in a matter of months or years), the atavism theory asserts that cancer never invents anything new but merely appropriates, or co-opts, or re-acquires, existing biological functionalities that are deeply pre-programmed into the cells’ genetic and epigenetic pathways. Conversely, loss of function in cancer occurs when cells revert to a more primitive phenotype, because in so doing they jettison, or lose, or decouple from more-recently evolved (and usually more sophisticated) capabilities. Among the (relatively) more recently-evolved biological capabilities is the adaptive immune system. The atavism theory predicts that, as cancer advances, the neoplasm progressively loses contact with adaptive immunity and becomes, in effect, immunosuppressed. In the atavism theory, cancer immunosuppression – which is well known – represents a loss of function (due to a reversion to a phenotype that predates the evolution of adaptive immunity about 400 million years ago) rather than a gain of function conferring a survival trait (i.e. ability to evade immune attack). But immunosuppression is a two-edged sword. It may confer protection from immune attack, but it is also an obvious weakness, making the tumour environment vulnerable to infectious agents.
The history of the interaction of bacteria, viruses and cancer is a very long and somewhat confused one, since William Coley obtained some amazing clinical results over a century ago 48. Some infections will boost the immune system and bring additional pressure on cancer cells, but some agents will directly infect the cancer cells preferentially in their immunosuppressed niches, for example oncolytic viruses. A variety of new approaches 49– 55 to immunotherapy exploits these features. The atavism theory predicts that advanced cancer will be particularly vulnerable to certain infectious agents, and specific treatment regimes have been advocated to take advantage of that aspect 44, 56.
Homeostatic regulation of immune reactivity and cancer
The relapsing and remitting behaviour of many chronic inflammatory states, such as arthritis, inflammatory bowel diseases, multiple sclerosis, and thyroiditis is well recognised. Diabetes, cardiovascular diseases and cancers of all types are now being considered similarly. The fluctuating, oscillating nature of these diseases has largely confounded our understanding to date and remained frustratingly unexplained, but is indicative that the immune system must be transitioning between stimulation/activation and suppression/tolerance phases repeatedly to produce the observed clinical picture. Moreover, oscillatory behaviour is highly characteristic of any homeostatic biological system under negative feedback control. This cyclical dynamic is a physical expression of physiological control to maintain relative constancy of the milieu intérieur, as recognised by Claude Bernard around 1867, and later Walter Cannon. Physiological constancy, or homeostatic control, of the body's immune status requires proportioned synchrony between effector stimulation and regulatory functions to be operational. Many cyclical examples, such as the diurnal temperature cycles, peri-monthly menstrual cycles, and 24-hour cortisol cycles have been elucidated by close serial monitoring.
The association between cancer and the host immune response has been recognised for over a century 57– 62. In animals, North et al. and more recently Klatzmann et al., demonstrated that the time of delivery of cytotoxic agents after tumour transplantation was crucial in determining whether tumour regression occurred or not 63– 72. Early clinical observations of inflammation and cancer regression were made by those treating cancer 57– 60, particularly the development of infection/fever after surgery. Chronic inflammation has been associated with cancer development, for example chronic ulceration and Marjolin's squamous cell cancer of the skin.
The immune system has innate and adaptive arms. C-Reactive Protein (CRP) is a non-specific functional analogue of immunoglobulin that binds to self/non-self cellular breakdown products of inflammation to initiate the adaptive immune responses 73, 74. T & B cells respond to cellular changes due to infection, damage or mutagenesis. To fine tune and limit these responses, the ensuing immune response is down-regulated paradoxically by the same cytokines and receptors that initiated it, but on functionally different cell types. Regulatory T-cells play a major role in this homeostatic attenuation and experimental and clinical evidence has shown that when these cells are either removed or blocked, cancer can completely regress, while autoimmune conditions may develop or worsen.
In recent years, it has become clear that the immune system recognises and processes both self- and non-self antigens to either respond or tolerate the antigen, but that homeostatic balance usually prevails.
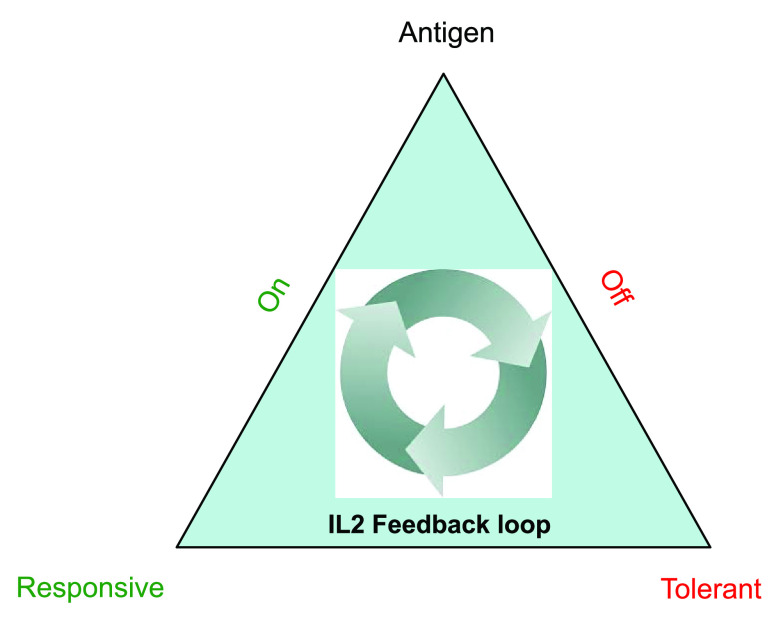
Immune responses can therefore be thought of as a “bi-stable” system existing in either of two principal states (responsive or tolerant). Antigen is the prime mover for either of these two states, and cytokines, most notably interleukin-2 (IL2), provide the feedback loop in the time domain to govern the direction. If antigen is continuously supplied to such a system (due to tumor cell growth/turnover) logic and physiology dictate that this response must oscillate 73– 82. Bi-stable oscillatory systems are characteristic of any homeostatic system with a feedback loop ( Figure 1).
Figure 1. The bi-stable oscillatory immune system pyramid with antigen at the apex and operational feedback facilitatory and inhibitory loops, driving both responsiveness and tolerance alternately to create homeostasis.
Anti-cancer agents and immune responses
Cytotoxic agents inhibit cell division to therapeutically damage and kill tumor cells. However, cancer cells divide asynchronously. About 20–30% of malignant cells within many solid cancers are dividing at any one time-point (greater rates of division occur in some cancers such as childhood leukaemia and testicular carcinoma). Regimens have evolved often with weekly dosing of sequential 'lines' (1st, 2nd, 3rd etc) of treatments or in combinations. Repetitive dosing of agents inducing multiple cycles of cell damage and antigen release (vaccination events) from the tumour is emerging as highly significant 56, 75– 77.
Cells of the immune system rapidly divide, but they divide synchronously and alternately (effector then regulatory) at different times sequentially to initiate then terminate an immune response in the time domain 73– 82.
Cytotoxic agents, unless applied discriminately, can aimlessly ablate different groups of proliferating immunological cells, as well as any proliferating tumor cells.
It is now clear that the immune system is not ignorant to the presence of tumors and that the normal homeostatic regulatory mechanisms are at the seat of the problem. This explains why immuno-modulatory agents, such as IL2, CTLA4, PD1/L1 monoclonal antibodies can deliver random dramatic complete responses in a limited percentage of late-stage cancer patients by interfering with the pre-existing homeostatic suppression/tolerance 81– 88. All of these agents can induce tolerance. The lack of efficacy of these agents in most patients is explained by induction of tolerance with some doses via regulatory T-cells while activating with other doses, the net balance of which can determine overall clinical outcome. Interestingly, autoimmunity can result from 'overdrive' of the immune system by some immunostimulatory agents and this has often been associated with better clinical responses against the cancer.
Improving results of natural selection
Most aberrant cells appearing in the human body as a result of somatic mutations are detected and disposed of by the immune system. Some are not and can produce pathology, with the majority of clinical cases of cancer occurring in older patients. This is explicable by the fact that natural selection operates principally by differential reproduction, consequently it is unable to operate for biological characteristic selection in non-reproductive (older) individuals. Thus, over the generations immune responses to malignant cells appearing in young people became adjusted by natural selection and, statistically speaking, operate efficiently, while such responses in older age were not “reachable” by natural selection for adjustment. This principle is not only applicable to specific immune responses, but encompasses the entire regulation of homeostatic balance of an organism. In practical terms, clinical intervention should imitate adaptation by selection of immunological processes occurring in younger organisms, to support, adjust and enhance natural operation of immune systems of older patients.
Concluding remarks and implications
Although knowledge has developed deeply concerning the immune system and cancer immunology, our contemporary understanding needs to be placed in evolutionary perspective. Our immune systems are the adaptive result of the necessity for defence against persistent selective pressures from environmental microbial pathogens. Over the millennia, the immune system and other body cells have undergone a continuous adaptive symbiotic process of synchronous, coordinated, cooperative, progressive immunological and somatic evolutionary change to provide what we observe today. Gradual evolution of adaptive immunity against infected and aberrant cells now explains many of the observations regarding cancer immunity and clinical responses. It is gradually being appreciated that normal immune regulatory mechanisms are holding back a primed immune response from selectively killing cancer cells. With an appreciation that immuno-modulation of pre-existing endogenous immune responses appears to occur with most cancer therapies, there is the serious prospect that serial immune monitoring might define optimal time-points for targeted administration of therapies to engineer effective complete clinical responses in a much more predictable, reliable and durable manner in the future. If achievable, increased long-term survival from advanced cancer, with reduced toxicity, might become a reality by harnessing the immuno-modulatory capacity of many currently existing therapeutic agents. The cost savings would be truly enormous 89.
Authors’ information
The authorship represents a unique collaboration between diverse disciplines with contributors having backgrounds and qualifications in cancer surgery, immunology, immunotherapy (BJC), basic science (MLA), evolutionary biology, anatomy, anthropology (MH), and the physical sciences, cancer biology (PD). As such, this work aims to approach the problem of cancer development and immune system recognition/responses uniquely from a scientific evolutionary perspective to explain many of the clinical observations that have been already made to date. Emanating from this understanding, new approaches and therapies might then be fruitfully generated for science and clinical medicine.
List of abbreviations
IL2 interleukin-2
CTLA4 cytotoxic T-lymphocyte associated protein 4
PD-1 programmed cell death protein 1
PD-L1 programmed death-ligand 1
HLA human leukocyte antigen
CD1 cluster of differentiation 1
DNA deoxyribonucleic acid
EMT epithelial-mesenchymal transition
MET mesenchymal–epithelial transition
PS-OC Physical Science-Oncology Centers
HIV human immunodeficiency virus
AIDS acquired immunodeficiency syndrome
HREV human endogenous retroviruses
Ma mega/million years
Ga giga/billion years
Funding Statement
This work was supported in part by NIH grant U54 CA143682.
[version 1; peer review: 2 approved with reservations]
References
- 1. Hackett CJ: On the Origin of the Human Treponematoses (Pinta, Yaws, Endemic Syphilis and Venereal Syphilis). Bull World Health Organ. 1963;29:7–41. [PMC free article] [PubMed] [Google Scholar]
- 2. Hackett CJ: An introduction to diagnostic criteria of syphilis, treponarid and yaws (treponematoses) in dry bones, and some implications. Virchows Arch A Pathol Anat Histol. 1975;368(3):229–41. 10.1007/BF00432525 [DOI] [PubMed] [Google Scholar]
- 3. Holloway KL, Henneberg RJ, de Barros Lopes M, et al. : Evolution of human tuberculosis: a systematic review and meta-analysis of paleopathological evidence. Homo. 2011;62(6):402–58. 10.1016/j.jchb.2011.10.001 [DOI] [PubMed] [Google Scholar]
- 4. Holloway KL, Staub K, Rühli F, et al. : Lessons from history of socioeconomic improvements: a new approach to treating multi-drug-resistant tuberculosis. J Biosoc Sci. 2014;46(5):600–20. 10.1017/S0021932013000527 [DOI] [PubMed] [Google Scholar]
- 5. Alizon S, de Roode JC, Michalakis Y: Multiple infections and the evolution of virulence. Ecol Lett. 2013;16(4):556–67. 10.1111/ele.12076 [DOI] [PubMed] [Google Scholar]
- 6. Greaves M, Maley CC: Clonal evolution in cancer. Nature. 2012;481(7381):306–13. 10.1038/nature10762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Henneberg M: The rate of human morphological microevolution and taxonomic diversity of hominids. Studies in Historical Anthropology. 2006;4.2004:49–59. Reference Source [Google Scholar]
- 8. Rasmussen HB: Interactions between Exogenous and Endogenous Retroviruses. J Biomed Sci. 1997;4(1):1–8. 10.1007/BF02255587 [DOI] [PubMed] [Google Scholar]
- 9. Krone B, Kölmel KF, Henz BM, et al. : Protection against melanoma by vaccination with Bacille Calmette-Guerin (BCG) and/or vaccinia: an epidemiology-based hypothesis on the nature of a melanoma risk factor and its immunological control. Eur J Cancer. 2005;41(1):104–117. 10.1016/j.ejca.2004.08.010 [DOI] [PubMed] [Google Scholar]
- 10. Hohn O, Hanke K, Bannert N: HERV-K(HML-2), the Best Preserved Family of HERVs: Endogenization, Expression, and Implications in Health and Disease. Front Oncol. 2013;3:246. 10.3389/fonc.2013.00246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. International Human Genome Sequencing Consortium: Finishing the euchromatic sequence of the human genome. Nature. 2004;431(7011):931–45. 10.1038/nature03001 [DOI] [PubMed] [Google Scholar]
- 12. Jones RB, Garrison KE, Mujib S, et al. : HERV-K-specific T cells eliminate diverse HIV-1/2 and SIV primary isolates. J Clin Invest. 2012;122(12):4473–89. 10.1172/JCI64560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chattopadhyay SK, Lander MR, Rands E, et al. : Structure of endogenous murine leukemia virus DNA in mouse genomes. Proc Natl Acad Sci U S A. 1980;77(10):5774–8. 10.1073/pnas.77.10.5774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kubo Y, Nakagawa Y, Kakimi K, et al. : Molecular cloning and characterization of a murine AIDS virus-related endogenous transcript expressed in C57BL/6 mice. J Gen Virol. 1994;75(pt 4):881–8. 10.1099/0022-1317-75-4-881 [DOI] [PubMed] [Google Scholar]
- 15. Kubo Y, Kakimi K, Higo K, et al. : Possible origin of murine AIDS (MAIDS) virus: conversion of an endogenous retroviral p12gag sequence to a MAIDS-inducing sequence by frameshift mutations. J Virol. 1996;70(9):6405–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jolicoeur P: Murine acquired immunodeficiency syndrome (MAIDS): an animal model to study the AIDS pathogenesis. FASEB J. 1991;5(10):2398–405. [DOI] [PubMed] [Google Scholar]
- 17. Beilharz MW, Sammels LM, Paun A, et al. : Timed ablation of regulatory CD4 + T cells can prevent murine AIDS progression. J Immunol. 2004;172(8):4917–25. 10.4049/jimmunol.172.8.4917 [DOI] [PubMed] [Google Scholar]
- 18. Meng L, Tompkins M, Miller M, et al. : Lentivirus-activated T regulatory cells suppress T helper cell interleukin-2 production by inhibiting nuclear factor of activated T cells 2 binding to the interleukin-2 promoter. AIDS Res Hum Retroviruses. 2014;30(1):58–66. 10.1089/AID.2013.0062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ondondo B, Jones E, Godkin A, et al. : Home sweet home: the tumor microenvironment as a haven for regulatory T cells. Front Immunol. 2013;4:197. 10.3389/fimmu.2013.00197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lee A, Nolan A, Watson J, et al. : Identification of an ancient endogenous retrovirus, predating the divergence of the placental mammals. Philos Trans R Soc Lond B Biol Sci. 2013;368(1626):20120503. 10.1098/rstb.2012.0503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wright BE, Schmidt KH, Minnick MF: Kinetic models reveal the in vivo mechanisms of mutagenesis in microbes and man. Mutat Res. 2013;752(2):129–37. 10.1016/j.mrrev.2012.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. French DL, Laskov R, Scharff MD: The role of somatic hypermutation in the generation of antibody diversity. Science. 1989;244(4909):1152–1157. 10.1126/science.2658060 [DOI] [PubMed] [Google Scholar]
- 23. Tomlinson IM, Walter G, Jones PT, et al. : The imprint of somatic hypermutation on the repertoire of human germline V genes. J Mol Biol. 1996;256(5):813–17. 10.1006/jmbi.1996.0127 [DOI] [PubMed] [Google Scholar]
- 24. Jones JM, Gellert M: The taming of a transposon: V(D)J recombination and the immune system. Immunol Rev. 2004;200:233–48. 10.1111/j.0105-2896.2004.00168.x [DOI] [PubMed] [Google Scholar]
- 25. Bianconi E, Piovesan A, Facchin F, et al. : An estimation of the number of cells in the human body. Ann Hum Biol. 2013;40(6):463–71. 10.3109/03014460.2013.807878 [DOI] [PubMed] [Google Scholar]
- 26. Savage DC: Microbial ecology of the gastrointestinal tract. Annu Rev Microbiol. 1977;31:107–133. 10.1146/annurev.mi.31.100177.000543 [DOI] [PubMed] [Google Scholar]
- 27. Gerritsen J, Smidt H, Rijkers GT, et al. : Intestinal microbiota in human health and disease: the impact of probiotics. Genes Nutr. 2011;6(3):209–240. 10.1007/s12263-011-0229-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mountford CE, Grossman G, Reid G, et al. : Characterization of transformed cells and tumors by proton nuclear magnetic resonance spectroscopy. Cancer Res. 1982;42(6):2270–6. [PubMed] [Google Scholar]
- 29. Mackinnon WB, Huschtscha L, Dent K, et al. : Correlation of cellular differentiation in human colorectal carcinoma and adenoma cell lines with metabolite profiles determined by 1H magnetic resonance spectroscopy. Int J Cancer. 1994;59(2):248–61. 10.1002/ijc.2910590218 [DOI] [PubMed] [Google Scholar]
- 30. Yakoub D, Keun HC, Goldin R, et al. : Metabolic profiling detects field effects in nondysplastic tissue from esophageal cancer patients. Cancer Res. 2010;70(22):9129–36. 10.1158/0008-5472.CAN-10-1566 [DOI] [PubMed] [Google Scholar]
- 31. Coventry B, Heinzel S: CD1a in human cancers: a new role for an old molecule. Trends Immunol. 2004;25(5):242–248. 10.1016/j.it.2004.03.002 [DOI] [PubMed] [Google Scholar]
- 32. Burrell RA, McGranahan N, Bartek J, et al. : The causes and consequences of genetic heterogeneity in cancer evolution. Nature. 2013;501(7467):338–45. 10.1038/nature12625 [DOI] [PubMed] [Google Scholar]
- 33. Munoz J, Swanton C, Kurzrock R: Molecular profiling and the reclassification of cancer: divide and conquer. Am Soc Clin Oncol Educ Book. 2013:127–34. 10.1200/EdBook_AM.2013.33.127 [DOI] [PubMed] [Google Scholar]
- 34. Murugaesu N, Chew SK, Swanton C: Adapting clinical paradigms to the challenges of cancer clonal evolution. Am J Pathol. 2013;182(6):1962–71. 10.1016/j.ajpath.2013.02.026 [DOI] [PubMed] [Google Scholar]
- 35. Jamal-Hanjani M, Thanopoulou E, Peggs KS, et al. : Tumour heterogeneity and immune-modulation. Curr Opin Pharmacol. 2013;13(4):497–503. 10.1016/j.coph.2013.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. S Datta R, Gutteridge A, Swanton C, et al. : Modelling the evolution of genetic instability during tumour progression. Evol Appl. 2013;6(1):20–33. 10.1111/eva.12024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ncayiyana DJ: The extraordinary story of the life after death of Henrietta Lacks. S Afr Med J. 2011;101(3):141. [DOI] [PubMed] [Google Scholar]
- 38. Njoku DB: The immortal life of Henrietta Lacks. Anesth Analg. 2013;117(1):286. 10.1213/ANE.0b013e31828bfecc [DOI] [PubMed] [Google Scholar]
- 39. Kiberstis PA, Travis J: Celebrating a glass half-full. Science. 2006;312(5777):1157. 10.1126/science.312.5777.1157 [DOI] [Google Scholar]
- 40. Tuma RS: Large trials, small gains: is change on the way? J Natl Cancer Inst. 2010;102(16):1216–1217, 1223. 10.1093/jnci/djq322 [DOI] [PubMed] [Google Scholar]
- 41. US National Institues of Health. President’s Cancer Panel. 2007– 2008 annual report.2012. Reference Source [Google Scholar]
- 42. Davies P: Rethinking cancer. Physics World. 2010;23(6):28. Reference Source [Google Scholar]
- 43. Davies PC, Lineweaver CH: Cancer tumors as Metazoa 1.0: tapping genes of ancient ancestors. Phys Biol. 2011;8(1):015001. 10.1088/1478-3975/8/1/015001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lineweaver CH, Davies PC, Vincent MD: Targeting cancer’s weaknesses (not its strengths): Therapeutic strategies suggested by the atavistic model. Bioessays. 2014;36(9):827–35. 10.1002/bies.201400070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Domazet-Lošo T, Klimovich A, Anokhin B, et al. : Naturally occurring tumours in the basal metazoan Hydra. Nat Commun. 2014;5:4222. 10.1038/ncomms5222 [DOI] [PubMed] [Google Scholar]
- 46. Warburg O: On the origin of cancer cells. Science. 1956;123(3191):309–314. 10.1126/science.123.3191.309 [DOI] [PubMed] [Google Scholar]
- 47. Adamson ED: Oncogenes in development. Development. 1987;99(4):449–71. [DOI] [PubMed] [Google Scholar]
- 48. Coley WB: The treatment of malignant tumors by repeated inoculations of erysipelas: with a report of ten original cases. Am J Med Sci. 1893;105(5):487–511. Reference Source [PubMed] [Google Scholar]
- 49. Kim SH, Castro F, Paterson Y, et al. : High efficacy of a Listeria-based vaccine against metastatic breast cancer reveals a dual mode of action. Cancer Res. 2009;69(14):5860–6. 10.1158/0008-5472.CAN-08-4855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gravekamp C, Paterson Y: Harnessing Listeria monocytogenes to target tumors. Cancer Biol Ther. 2010;9(4):257–65. 10.4161/cbt.9.4.11216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Nguyen VH, Kim HS, Ha JM, et al. : Genetically engineered Salmonella typhimurium as an imageable therapeutic probe for cancer. Cancer Res. 2010;70(1):18–23. 10.1158/0008-5472.CAN-09-3453 [DOI] [PubMed] [Google Scholar]
- 52. Galmbacher K, Heisig M, Hotz C, et al. : Shigella mediated depletion of macrophages in a murine breast model is associated with tumor regression. PLoS One. 2010;5(3):e9572. 10.1371/journal.pone.0009572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Quispe-Tintaya W, Chandra D, Jahangir A, et al. : Nontoxic radioactive Listeria at is a highly effective therapy against metastatic pancreatic cancer. Proc Natl Acad Sci USA. 2013;110(21):8668–73. 10.1073/pnas.1211287110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Coster TS, Hoge CW, VanDeVerg LL, et al. : Vaccination against shigellosis with attenuated Shigella flexneri 2a strain SC602. Infect Immun. 1999;67(7):3437–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Donnelly O, Harrington K, Melcher A, et al. : Live viruses to treat cancer. J R Soc Med. 2013;106(8):310–4. 10.1177/0141076813494196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Coventry BJ, Lilly CA, Hersey P, et al. : Prolonged repeated vaccine immuno-chemotherapy induces long-term clinical responses and survival for advanced metastatic melanoma. J Immunother Cancer. 2014;2:9. 10.1186/2051-1426-2-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Coley WB: Contribution to the knowledge of sarcoma. Ann Surg. 1891;14(3):199–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Coley WB: Treatment of inoperable malignant tumors with toxins of erysipelas and the bacillus prodigiosus. Trans Am Surg Assn. 1894;12:183–212. [Google Scholar]
- 59. Coley WB: Disappearance of a recurrent carcinoma after injections of mixed toxins. Ann Surg. 1912;55:897–8. [Google Scholar]
- 60. Erysipelas and prodigiosus toxins (Coley). JAMA. 1934;103(14):1070–71. 10.1001/jama.1934.02750400038015 [DOI] [Google Scholar]
- 61. Hoption Cann SA, van Netten JP, van Netten C, et al. : Spontaneous regression: a hidden treasure buried in time. Med Hypotheses. 2002;58(2):115–9. 10.1054/mehy.2001.1469 [DOI] [PubMed] [Google Scholar]
- 62. Hoption Cann SA, van Netten JP, van Netten C: Dr William Coley and tumour regression: a place in history or in the future. Postgrad Med J. 2003;79(938):672–680. [PMC free article] [PubMed] [Google Scholar]
- 63. North RJ, Awwad M: T cell suppression as an obstacle to immunologically-mediated tumor regression: elimination of suppression results in regression. Prog Clin Biol Res. 1987;244:345–58. [PubMed] [Google Scholar]
- 64. Awwad M, North RJ: Immunologically mediated regression of a murine lymphoma after treatment with anti-L3T4 antibody. A consequence of removing L3T4+ suppressor T cells from a host generating predominantly Lyt-2+ T cell-mediated immunity. J Exp Med. 1988;168(6):2193–206. 10.1084/jem.168.6.2193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Awwad M, North RJ: Cyclophosphamide (Cy)-facilitated adoptive immunotherapy of a Cy-resistant tumour. Evidence that Cy permits the expression of adoptive T-cell mediated immunity by removing suppressor T cells rather than by reducing tumour burden. Immunology. 1988;65(1):87–92. [PMC free article] [PubMed] [Google Scholar]
- 66. Awwad M, North RJ: Sublethal, whole-body ionizing irradiation can be tumor promotive or tumor destructive depending on the stage of development of underlying antitumor immunity. Cancer Immunol Immunother. 1988;26(1):55–60. 10.1007/BF00199848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Hill JO, Awwad M, North RJ: Elimination of CD4+ suppressor T cells from susceptible BALB/c mice releases CD8+ T lymphocytes to mediate protective immunity against Leishmania. J Exp Med. 1989;169(5):1819–27. 10.1084/jem.169.5.1819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Awwad M, North RJ: Cyclophosphamide-induced immunologically mediated regression of a cyclophosphamide-resistant murine tumor: a consequence of eliminating precursor L3T4+ suppressor T-cells. Cancer Res. 1989;49(7):1649–54. [PubMed] [Google Scholar]
- 69. North RJ, Awwad M, Dunn PL: The immune response to tumors. Transplant Proc. 1989;21(1 Pt 1):575–7. [PubMed] [Google Scholar]
- 70. North RJ, Awwad M: Elimination of cycling CD4+ suppressor T cells with an anti-mitotic drug releases non-cycling CD8+ T cells to cause regression of an advanced lymphoma. Immunology. 1990;71(1):90–5. [PMC free article] [PubMed] [Google Scholar]
- 71. Awwad M, North RJ: Radiosensitive barrier to T-cell-mediated adoptive immunotherapy of established tumors. Cancer Res. 1990;50(8):2228–33. [PubMed] [Google Scholar]
- 72. Darrasse-Jèze G, Bergot AS, Durgeau A, et al. : Tumor emergence is sensed by self-specific CD44 hi memory Tregs that create a dominant tolerogenic environment for tumors in mice. J Clin Invest. 2009;119(9):2648–62. 10.1172/JCI36628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Coventry BJ, Ashdown ML, Quinn MA, et al. : CRP identifies homeostatic immune oscillations in cancer patients: a potential treatment targeting tool? J Transl Med. 2009;7:102. 10.1186/1479-5876-7-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Ashdown ML Coventry BJ: A Matter of Time. Australasian Science. 2010;18–20. Reference Source [Google Scholar]
- 75. Coventry BJ, Hersey P, Halligan A-M, et al. : Immuno-Chemotherapy Using Repeated Vaccine Treatment Can Produce Successful Clinical Responses in Advanced Metastatic Melanoma. Journal of Cancer Therapy. 2010;1:205–213. 10.4236/jct.2010.14032 [DOI] [Google Scholar]
- 76. Coventry BJ, Ashdown ML, Markovic SN: Immune Therapies for Cancer: Bimodality—The Blind Spot to Clinical Efficacy—Lost in Translation. J Immunother. 2011;34:717. [Google Scholar]
- 77. Coventry BJ, Ashdown ML: Complete clinical responses to cancer therapy caused by multiple divergent approaches: a repeating theme lost in translation. Cancer Manag Res. 2012;4:137–149. 10.2147/CMAR.S31887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Coventry BJ, Ashdown ML: The 20th anniversary of interleukin-2 therapy: bimodal role explaining longstanding random induction of complete clinical responses. Cancer Manag Res. 2012;4:215–21. 10.2147/CMAR.S33979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. McNally A, Hill GR, Sparwasser T, et al. : CD4 + CD25 + regulatory T cells control CD8 + T-cell effector differentiation by modulating IL-2 homeostasis. Proc Natl Acad Sci U S A. 2011;108(18):7529–7534. 10.1073/pnas.1103782108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Boyman O, Sprent J: The role of interleukin-2 during homeostasis and activation of the immune system. Nat Rev Immunol. 2012;12(3):180–190. 10.1038/nri3156 [DOI] [PubMed] [Google Scholar]
- 81. Jain N, Nguyen H, Chambers C, et al. : Dual function of CTLA-4 in regulatory T cells and conventional T cells to prevent multiorgan autoimmunity. Proc Natl Acad Sci U S A. 2010;107(4):1524–8. 10.1073/pnas.0910341107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. A delicate balance: tweaking IL-2 immunotherapy. Nat Med. 2012;18(2):208–209. 10.1038/nm0212-208 [DOI] [PubMed] [Google Scholar]
- 83. Hodi FS, O’Day SJ, McDermott DF, et al. : Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–723. 10.1056/NEJMoa1003466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Prieto PA, Yang JC, Sherry RM, et al. : CTLA-4 blockade with ipilimumab: long-term follow-up of 177 patients with metastatic melanoma. Clin Cancer Res. 2012;18(7):2039–2047. 10.1158/1078-0432.CCR-11-1823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Topalian SL, Hodi FS, Brahmer JR, et al. : Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443–54. 10.1056/NEJMoa1200690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Brahmer JR, Tykodi SS, Chow LQ, et al. : Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366(26):2455–65. 10.1056/NEJMoa1200694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Ott PA, Hodi FS, Robert C: CTLA-4 and PD-1/PD-L1 Blockade: New Immunotherapeutic Modalities with Durable Clinical Benefit in Melanoma Patients. Clin Cancer Res. 2013;19(19):5300–5309. 10.1158/1078-0432.CCR-13-0143 [DOI] [PubMed] [Google Scholar]
- 88. Wolchok JD, Kluger H, Callahan MK, et al. : Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 2013;369(2):122–33. 10.1056/NEJMoa1302369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Murphy KM, Topel RH: The value of health and longevity. J Polit Econ. 2006;114(51):871–904. Reference Source [Google Scholar]