Abstract
Aim:
The aim of this study was to understand the impact of an active meditation protocol on heart rate variability (HRV) and mood in women as compared to breath-focused silence meditation.
Materials and Methods:
Women experienced two different practices of 20 min each: (a) control group: silence meditation focusing on breath and (b) experiment group: active meditation that included four activities, each lasting for 5 minutes – (1) simple humming, (2) coherent heart-focused breathing with 5s of inhalation and 5s of exhalation, (3) coherent heart-focused breathing while invoking positive emotions, and (4) guided imagery about a preidentified goal. The silence meditation encouraged women to only focus on the breath. The Positive and Negative Affect Scale measured mood before/after the practice (n = 24), and emWavePro device measured HRV parameters for 5 min before/after the practices (n = 18). Statistical data analysis was done using a paired t-test.
Results:
HRV (specifically, parasympathetic nervous system [PNS]) parameters showed a statistically significant improvement in the experiment group as compared to the control group. There was a statistically significant reduction in negative affect after both the practices, and the increase in positive affect was observed only for the experiment group.
Conclusions:
The active meditation provides a significant enhancement in mood and HRV parameters related to PNS as compared to silence meditation where the changes in HRV were not consistent and the positive mood did not increase significantly. Future research in this area could explore the impact of such practice for a longer duration and understand the impact of each component of the meditative practices.
Keywords: Active meditation, emotions, heart rate variability, Positive and Negative Affect Scale, self-hypnosis, silence meditation, The SEE protocol
Introduction
Emotional health's importance in well-being and quality of life is growing based on the mounting evidence of the role played by stress on mood, nervous system, sleep disruption, and chronic disease (noncommunicable disease).[1] Persistent stress plays a major role not just in physical but also emotional health and cognitive functions.[2] Recent evidence has demonstrated the linkage between stress levels and fertility.[3] The changes induced by stress on cognitive function impact the ability to learn and remember.[4] Finally, the evidence also confirms the linkage between stress and depression or mood via pathways that impact the autonomic nervous system (ANS), hormones, and also the immune system.[5] With a growing demand for development, in countries like India where only less than one-third of women (≥15 years age) are either working or actively looking for a job, there is a likelihood of more women joining the workforce.[6] With more work pressure and the need to manage the home, there is a likely increase in stress levels for women in India and, in general, across the developing countries.
Stress, mood, and implications on health and heart rate variability
To address the stress, it is important to understand how stress impairs the ANS, mood, and its implications for quality of well-being and health. ANS consists of two core parts: (a) sympathetic nervous system (SNS) – in charge of fight-or-flight situations such as when we are faced with an emergency such as a wild animal, the brain prepares our body to either fight with the animal or run away to a safe place. The internal changes related to such situations (even if it is imaginary or emotional and not a physical situation) are governed by SNS. (b) Parasympathetic nervous system (PNS) – which restores the energy and body balance after the trigger (e.g., wild animal) is gone.[7] Maintaining a healthy balance (also known as homeostasis) between the two core branches of ANS is important for long term physical and emotional well-being, and stress impairs this balance via overactivation of SNS.
Poor lifestyle choices such as sleep disruption, increased work-life balance challenges, reduced physical activity, and calorie-heavy diet, along with emotional stress, impact the quality of life, decrease heart rate variability (HRV) (beat-to-beat variations in heart rate-HR), and lead to increased prevalence of metabolic syndrome (set of measures defining the risk for chronic disease) and eventually chronic disease.[8] Moreover, studies have also confirmed a reciprocal link between depression and obesity. Depression is an important risk factor not only in binge eating but also in the development of obesity. At the same time, obesity is found to increase depression risk.[9] Together, these findings indicate a need to manage overall emotional well-being through self-regulation processes which can be easily learned and practiced regularly. The journey from good health to poor health, eventually leading to chronic disease or cognitive function decline, often disturbs the homeostasis of ANS leading to an increase in SNS activities.
HRV has emerged as an indicator of health and quality of life.[8] The studies have demonstrated that individuals with high HRV tend to have better emotional and physical well-being compared to those with low HRV.[10] Recent studies also indicate that (a) positive and negative mood induction tasks result in differential ANS responses as measured by HRV and specifically (b) multiple HRV indices have significant differences between happiness and sadness emotion states.[11,12] The evidence, therefore, indicates that an increase in HRV could lead to better mood and could enhance the autonomic function balance, and hence, studies involving HRV have the potential to provide insight into a wide variety of psychological and physiological processes.[13] In general, to counter the stress, the PNS-related HRV parameters must be enhanced to restore the overall balance.
Meditation, mood, and heart rate variability
Meditation research over the past several decades has, in general, demonstrated an improvement in mood, reduction in anxiety, and increase in focus and an overall improvement in HRV/ANS.[14,15,16] However, the studies have also indicated some negative implications of meditative practices. For example, recent research identified that out of >1100 respondents surveyed across several countries, 32% reported disturbing feelings of fear, dread, or terror during or as a result of their meditation practice.[17,18,19] The research indicates a need to study the adverse impact of meditation and also understand if some active practices could result in better outcomes. Active interventions such as slow and coherent breathing, hypnotic suggestions, or guided imagery have demonstrated an improvement in HRV parameters indicative of relaxation and increased cognition.[20,21,22]
The review of the literature identified an opportunity to define a protocol aimed to improve both physiology and emotions through coherent breathing and humming practices followed by self-suggestion based on positive emotions and guided imagery. Specifically, SNS activation is indicated by an increase in HR, a decrease in root mean square of successive differences (RMSSD) (The RMSSD reflects the beat-to-beat variations in heart's signals and is the primary time domain measure used to estimate the vagally mediated changes reflected in HRV), and a decrease in percentage of high frequency normalized unit power (%HF n.u.). HRV's frequency domain measurements are divided into ultra-low frequency, very low frequency and high frequency bands.[22] Whereas, an increase in RMSSD and % HF nu power value indicates an increase in PNS. An increase in PNS is also accompanied by a decrease in SNS activation related parameters, for example, reduction in HR. Therefore, the study aimed at not just measuring the mood of two different kinds of meditation but also measuring the changes in physiology through HRV parameters, specifically RMSSD, HR, and % HF nu.
Objectives
The objectives of the study were to validate that seated 20 min long active meditation via the SEE protocol has a statistically significant impact as compared with 20 min seated breath focused silence meditation on (a) the mood (positive affect [PA] and negative affect [NA], as measured by the Positive and Negative Affect Scale [PANAS] survey) and (b) physiology (as measured by HRV parameters such as HR, RMSSD, and % HF nu power).[10]
Hypothesis
We hypothesized that compared to breath-focused silence meditation, the experiment group (through active changes in physiology and emotions) would result in (a) a more pronounced increase in PA and (b) a similar decrease in NA and (c) more relaxation observed through key HRV parameters denoting the PNS components. The activity to increase coherence and invocation of positive emotion with guided imagery could be the elements driving the enhanced mood and increased relaxation for the experiment group.[23,24]
Materials and Methods
Subjects
The participants [all healthy women aged 20–60, details in Tables 1 and 2] were recruited for the study via the announcement on social media. Signed consent was taken from all participants after they responded to the announcement, and ethics committee approval was not required due to the simple nature of the practice. Exclusion criteria included any chronic disease (e.g., diabetes and hypertension). Due to limited availability of the HRV devices, the number of samples for HRV data was less (n = 18) as compared to the PANAS survey (n = 24).
Table 1.
Demographics for heart rate variability participants in both groups
| Parameter | HRV for silence | HRV for SEE protocol |
|---|---|---|
| n | 18 | 18 |
| Age (mean±SD) | 32.94±12.09 | 33.83±13.34 |
SD=Standard deviation, HRV=Heart rate variability, SEE= Society for Energy and Emotions
Table 2.
Demographics for Positive and Negative Affect Scale participants in both groups
| Parameter | PANAS for silence | PANAS for SEE protocol |
|---|---|---|
| n | 24 | 24 |
| Age (mean±SD) | 33±13.9 | 30±11.12 |
PANAS=Positive and Negative Affect Scale, SD=Standard deviation, HRV=Heart rate variability, SEE= Society for Energy and Emotions
Design
Participants were randomly assigned to either experiment group or control group while ensuring they avoided meal and coffee or tea at least 3 h before the practice. The study was conducted in a quiet, air-conditioned room while maintaining the temperature of 25°C at the same venue.
Interventions
The methodology for the study is shown in Figure 1. Both the groups had similar measurement methodology, and each practice was 20 min long.
Figure 1.
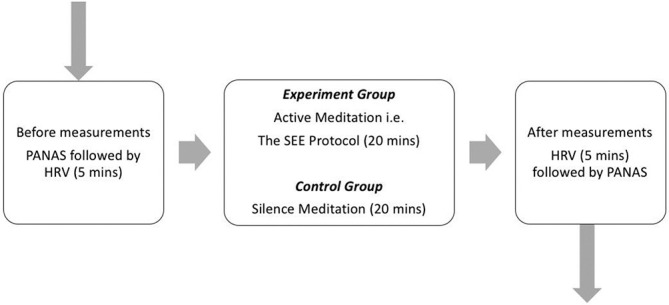
Methodology for the study
Breath-focused silence meditation
For silence meditation, the participants were instructed to sit with eyes closed throughout the 30-min. PANAS form was administered before and after the 30-min practice, while HRV data were measured throughout the practice. The instructions were given to focus only on the breath and allow the breath to be automatic (i.e., no regulation of the breath). If thoughts came up, the participants were instructed to bring the focus back to the breath.
Society for Energy and Emotions Protocol (the SEE Protocol)
For the experiment group, the detailed process was explained, and three authors (MS, VP, and MD) personally guided the participant and monitored the progress throughout the practice. PANAS form was administered, as shown in Figure 1 before and after the practice, and HRV data were measured throughout the practice. The detailed steps of the SEE protocol are captured in [Table 3]. This active meditation or self-hypnosis process was designed to invoke several important physiological and emotional states which are likely to improve HRV and therefore enhance emotional regulation.[25] The coherence through humming (simple monotonous nasal sound at a comfortable breathing length) and slow coherent breathing increase the high-amplitude oscillations that have a causal impact on the emotional regulation. Evidence also demonstrated that self-hypnosis or auto-suggestions have a positive impact on emotional regulation even for individuals with low suggestibility.[26]
Table 3.
Details of the SEE protocol
| Number | Activity | Description | Duration (min) |
|---|---|---|---|
| 1 | Simple humming | Comfortable seating position, avoid if vertigo | 5 |
| 2 | Coherent breathing | 10s (5 s inhalation and 5 s exhalation) as per the comfort Focus on the heart center | 5 |
| 3 | Invoking positive emotions (e.g., gratitude and love) | Focus on the heart center, maintain coherent breathing and invoke the emotions | 5 |
| 4 | Guided imagery | Based on prework on identified goal. Invoke the state related to the goal | 5 |
SEE= Society for Energy and Emotions
Most meditative practices result in prominent oscillations in normal heartbeats, and this is associated with high coherence between HR and breathing cycles. Active meditations are known to increase HR oscillations and thereby enhance the emotional states and reduce anxiety and other negative emotions.[27] Finally, evidence has demonstrated that guided imagery has a healing impact on the mind and body while enhancing the HRV.[28,29] All the above evidence was integrated into the design of the active meditative or SEE self-hypnosis protocol.
Assessments and analysis
PANAS form, used for psychological assessments, is a self-report psychometric questionnaire that can be used across a diverse sample group. It can measure two segments or moods of an individual. Each segment has 10 terms in which the participant can rate from 1 to 5. The outcome provides PA and NA score ranging from 10 to 50, and a high score indicates higher PA and lower levels of negative scores indicating lower NA.[30] PANAS can measure the PA and NA of the participant before and after any intervention.[31,32] PANAS has been widely used to measure overall mood change in clinical studies involving patients as well as healthy individuals.[23] PANAS survey data were validated for normal distribution, entered into Excel, and analyzed via a paired t-test. HRV was measured using Emwave Pro device (HeartMath Inc.) that uses infrared pulse plethysmograph ear sensor or optional finger sensor to measure the beat-to-beat intervals. These data were exported via.txt file from the Emwave Pro software for further analysis with Kubios Premium HRV software. The output of Kubios (processed HRV data) was imported back into Microsoft Excel for further analysis, including the P value using a paired t-test after validation for the normal distribution. For this study, we used (a) HR, (b) RMSSD, and (c) HF power, i.e., % HF nu parameters of the HRV. Together, these three commonly used parameters of physiology provide an understanding of the PNS and SNS components of the ANS. Specifically, changes in HR provide an indicator of the reduction in SNS activity. The increase in RMSSD and to some extent % HF nu denotes a pronounced PNS activity.[24]
Results
Changes in Mood (Positive and Negative Affect Scale score)
PANAS results are captured below [Table 4] for both the groups:
Table 4.
Positive and Negative Affect Scale survey score before and after SEE protocol (experiment group)
| Group | Positive affect, mean±SD | Negative affect, mean±SD | ||||
|---|---|---|---|---|---|---|
| Before | After | P | Before | After | P | |
| SEE protocol | 35.25±6.75 | 38.38±7.97 | 0.007* | 16.13±4.86 | 12.13±3.80 | 0.000* |
| Silence | 36.71±6.77 | 38.46±8.32 | 0.100 | 16.13±3.80 | 13.79±5.18 | 0.001* |
*Denotes a statistically significant change in the “after” data as compared to “before.” Both PA and NA scores range from 10–50, high PA scores indicate higher positive affect, and lower levels of NA scores indicate lower negative affect. PA=Positive affect, NA=Negative affect, SD=Standard deviation, SEE= Society for Energy and Emotions
For the experiment group, the PA score increased from 35.25 to 38.38 and the NA score decreased from 16.13 to 12.13. Both these changes were statistically significant as measured via a paired t-test, with P = 0.007 for change in PA and 0.000 for change in NA.
For the control group, the mean PA score increased from 36.71 to 38.46, and this increase was not statistically significant (P = 0.10). For the control group (silence meditation), the reduction in NA scores from 16.13 to 13.79 was statistically significant (P = 0.001).
The PANAS survey findings indicate that the SEE Protocol results in statistically significant improvement in both PA and NA. However, for breath-focused silence practice, the reduction in NA was statistically significant and the increase in PA was not statistically significant. This outcome validates the primary objective of the study that the SEE protocol (active meditative or self-hypnosis protocol) has a bigger influence on the mood via the statistically significant change in both the moods as compared to silence.
HRV parameters for the experiment group (SEE protocol) and the control group (silence group) are captured in Table 5. Statistical analysis of the data indicates the following:
Table 5.
Changes in key heart rate variability parameters before (0–5 min) and after (20–25 min) both the interventions
| Group | HR, mean±SD | RMSSD, mean±SD | Percentage of HF nu power, mean±SD | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Before | After | P | Before | After | P | Before | After | P | |
| SEE protocol | 80.95±8.09 | 78.18±11.22 | 0.02* | 43.73±20.64 | 51.78±26.42 | 0.04* | 28.37±19.12 | 46.51±24.68 | 0.0002* |
| Silence | 75.72±10.04 | 72.42±6.2 | 0.02* | 49.86±25.7 | 60.82±34.6 | 0.004* | 47.78±21.32 | 46.24±18.94 | 0.39 |
*Denotes a statistically significant change in the “after” data as compared to “before.” HR=Heart rate, RMSSD=Root mean square of successive differences, HF nu = High-frequency normalized unit, SEE= Society for Energy and Emotions
For SEE protocol, there is a statistically significant reduction in all the three parameters, i.e., HR, RMSSD, and % HF nu power [Table 5]
For silence, there is a statistically significant reduction in HR and RMSSD. However, in % HF nu power, the changes are not statistically significant [Table 5]
% HF nu power correlates with a PNS denoting relaxation. Lower HF nu power is correlated with a negative state of mind such as stress, anxiety, or worry, and a statistically significant improvement in HF power denotes a reduction in negative mood (evident through PANAS results) and shows increased relaxation.[29] The changes in HR, RMSSD, and HF power clearly demonstrate an increase in overall PNS activity in SEE protocol. In silence, the HF power does not increase in a statistically significant manner, and hence, it can be inferred that during silence, the extent of decrease in PNS activity was not very consistent.
Together, the above results validate the primary objective (b) that during the SEE protocol, there is a statistically significant improvement across multiple HRV parameters. In silence, not all the parameters, specifically related to the PNS system, show a statistically significant change.
Discussion
Unique findings
The results provide an interesting perspective about the statistically significant increase in PA and changes in HRV parameters, i.e., the reduction in HR denotes SNS reduction and the increase of RMSSD and HF power denotes enhancement in PNS. Specifically, RMSSD denotes the increased amplitude of heart oscillations denoting enhanced emotional regulation. The HF power reflects HRV attributable to respiratory sinus arrhythmia considered as a marker of vagal modulation of beat-to-beat heart intervals and a cardiac parasympathetic effect. Earlier research has demonstrated the positive impact of guided imagery on the total power and HF power.[33] An increase in HF power has been also been reported in quite a few studies related to meditation.[34] Studies have also reported an increase in HF power in response to positive emotion induction, relaxation exercises, and meditation. At the same time, there is evidence that some individuals may face a decrease in HF power, and this could be associated with risk factors or psychophysiology. The use of various coherence inducing techniques, positive emotions, and guided imagery together may have played a role in the increase of HF power and an increase in RMSSD which could have contributed to positive emotions resulting in the increase in PA during SEE protocol. This is a unique outcome from the study since the breath-focused silence meditation, with the absence of any active practices that could influence HF power, did not generate a statistically significant increase in both PA and HF power (though in silence there were SNS reduction due to decrease in HR and also some activation in PNS through increase in RMSSD). The findings can be leveraged to improve the experience of the meditative practice, and a longer practice could have a lasting impact on the ANS.
Limitations and future work
The use of multiple techniques in the SEE protocol together is a limitation since that makes it difficult to identify which activity contributed to the increase in HRV parameters including HF power and mood. Future work in this area should separate various components of the SEE protocol and explore how each component correlates with the increase in HRV parameters. This could also be explored for individuals with autonomic dysfunction to understand if their results related to HRV changes would vary compared to an apparently healthy group. Future work should use a bigger sample size and add more specific positive and negative emotion-related measurements to gain a deeper understanding of the changes. For this study, the participants' unsolicited qualitative feedback ranged from an increase in creativity to improvement in quality of sleep. Along with an increase in sample size, future work could explore the impact of longer practice (i.e., 4–6 weeks) on anxiety, depression, and sleep quality. Participants of the SEE protocol group also reported the complexity of multiple different activities in the protocol. Proper training must be incorporated in future studies and/or additional ongoing assistance to ensure better quality results and benefits for the participants.
Conclusions
The findings of the study provide a strong case to incorporate active practices in meditation as compared to just silence due to the positive impact on the mood and nervous system. Specifically, an increase in PNS measures and the positive mood could benefit the individuals who may be facing some negative emotions during “silence” meditation. Such active practice could be more beneficial to individuals with anxiety and depression as compared to silence and may have a positive impact on sleep quality. These are the areas for possible future work related to such active meditation. Finally, the specific components of the active meditation could be separately studied to understand if the combined use of various techniques resulted in this outcome or was contributed by any specific element of the practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to acknowledge the role of Riri G Trivedi (regression and hypnotherapy trainer and HeartMath certified mentor) in the design and development of the SEE protocol. Authors would also like to acknowledge the generous encouragement and support of Puey Chin Chew.
References
- 1.Han KS, Kim L, Shim I. Stress and sleep disorder.Exp Neurobiol? 2012 Dec;21(4):141–50. doi: 10.5607/en.2012.21.4.141. doi: 10.5607/en.2012.21.4.141. Epub 2012 Dec 26. PMID: 23319874; PMCID: PMC3538178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trivedi GT, Saboo B, Hasnani D. Importance of screening for sleep disorders (Chronic disease) J Clin Diabetol. 2018;5:3. [Google Scholar]
- 3.Rooney KL, Domar AD. The relationship between stress and infertility. Dialogues Clin Neurosci. 2018;20:41–7. doi: 10.31887/DCNS.2018.20.1/klrooney. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vogel S, Schwabe L. Learning and memory under stress: Implications for the classroom. NPJ Sci Learn. 2016;1:16011. doi: 10.1038/npjscilearn.2016.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Won E, Yong-Ku K. Stress, the autonomic nervous system, and the immune-kynurenine pathway in the etiology of depression. Curr Neuropharmacol. 2016;14:665–73. doi: 10.2174/1570159X14666151208113006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The World Bank Website. [[Last accessed on 2020 Mar 03]]. Available from: https://wwwworldbankorg/en/news/feature/2019/03/08/working-for-women-in-india .
- 7.Trivedi Gunjan Y, Hemalatha R, Ramani KV. Chronic Diseases and Mind Body Management, an Introduction (Technical Note), Reference No: CMHS0044TEC Indian Institute of Management. 2018 May [Google Scholar]
- 8.Trivedi G, Saboo B, Singh R, Maheshwari A, Sharma K, Verma N. Can decreased heart rate variability be a marker of autonomic dysfunction, metabolic syndrome and diabetes? J Diabetol. 2019;10:48. [Google Scholar]
- 9.Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Archives of General Psychiatry. 2010;67:220–9. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 10.SEE Protocol was Developed by Gunjan Y Trivedi and Riri G Trivedi Society for Energy & Emotions Wellness Space Ahmedabad India. [[Last accessed on 2020 Jul 05]]. Available from: http://wwwwellness-space net/SEE .
- 11.Kop WJ, Synowski SJ, Newell ME, Schmidt LA, Waldstein SR, Fox NA. Autonomic nervous system reactivity to positive and negative mood induction: The role of acute psychological responses and frontal electrocortical activity. Biol Psychol. 2011;86:230–8. doi: 10.1016/j.biopsycho.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shi H, Yang L, Zhao L, Su Z, Mao X, Zhang L, et al. Differences of heart rate variability between happiness and sadness emotion states: A pilot study. Journal of Medical and Biological Engineering. 2017;37:527–39. [Google Scholar]
- 13.Grippo AJ. Opinion: Heart rate variability, health and well-being: A systems perspective research topic. Front Public Health. 2017;5:246. doi: 10.3389/fpubh.2017.00246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Basso JC, McHale A, Ende V, Oberlin DJ, Suzuki WA. Brief, daily meditation enhances attention, memory, mood, and emotional regulation in non-experienced meditators. Behavioural Brain Research. 2019;356:208–20. doi: 10.1016/j.bbr.2018.08.023. [DOI] [PubMed] [Google Scholar]
- 15.Manocha, Ramesh, et al. “A randomized, controlled trial of meditation for work stress, anxiety and depressed mood in full-time workers”. Evidence-based Complementary and Alternative Medicine eCAM 2011 (2011) doi: 10.1155/2011/960583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Needleman J, Deane H. Shapiro, Jr Meditation: Classic and Contemporary Perspectives. 2017:1713. [Google Scholar]
- 17.Vieten C, Wahbeh H, Cahn BR, MacLean K, Estrada M, Mills P, et al. Future directions in meditation research: Recommendations for expanding the field of contemplative science. PLoS One. 2018;13:e0205740. doi: 10.1371/journal.pone.0205740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schlosser M, Sparby T, Vörös S, Jones R, Marchant NL. Unpleasant meditation-related experiences in regular meditators: Prevalence, predictors, and conceptual considerations. PLoS One. 2019;14:E0216643. doi: 10.1371/journal.pone.0216643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Léonard, Anne, et al. “Changes in heart rate variability during heartfulness meditation: A power spectral analysis including the residual spectrum”. Frontiers in cardiovascular medicine. 2019;6:62. doi: 10.3389/fcvm.2019.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yüksel R, Ozcan O, Dane S. The effects of hypnosis on heart rate variability. Int J Clin Experim Hypnosis. 2013;61(2):162–71. doi: 10.1080/00207144.2013.753826. [DOI] [PubMed] [Google Scholar]
- 21.Boselli E, Musellec H, Martin L, Bernard F, Fusco N, Guillou N, et al. “Effects of hypnosis on the relative parasympathetic tone assessed by ANI (Analgesia/Nociception Index) in healthy volunteers: a prospective observational study.” Journal of clinical monitoring and computing 32, no3. 2018:487–492. doi: 10.1007/s10877-017-0056-5. [DOI] [PubMed] [Google Scholar]
- 22.Shaffer F, McCraty R, Zerr CL. A healthy heart is not a metronome: An integrative review of the heart's anatomy and heart rate variability. Front Psychol. 2014;5:1040. doi: 10.3389/fpsyg.2014.01040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ding X, Tang Y, Tang R, et al. Improving creativity performance by short-term meditation? Behav Brain Funct. 2014;10:9. doi: 10.1186/1744-9081-10-9. Doi: https://doi.org/10.1186/1744-9081-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kubios Website: https://www.kubios.com/about-hrv/kubioscom/about-hrv/ [Google Scholar]
- 25.Mather M, Thayer J. How heart rate variability affects emotion regulation brain networks? Curr Opin Behav Sci. 2018;19:98–104. doi: 10.1016/j.cobeha.2017.12.017. doi:10.1016/j.cobeha.2017.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jensen MP, Jamieson GA, Lutz A, Mazzoni G, McGeown WJ, Santarcangelo EL, et al. New directions in hypnosis research: strategies for advancing the cognitive and clinical neuroscience of hypnosis. Neuroscience of Consciousness. 2017;2017:nix004. doi: 10.1093/nc/nix004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peng CK, et al. Heart rate dynamics during three forms of meditation, International Journal of Cardiology. 95:19. doi: 10.1016/j.ijcard.2003.02.006. [DOI] [PubMed] [Google Scholar]
- 28.Bedford FL. A perception theory in mind–body medicine: guided imagery and mindful meditation as cross-modal adaptation. Psychonomic Bulletin and Review. 2012;19:24–45. doi: 10.3758/s13423-011-0166-x. [DOI] [PubMed] [Google Scholar]
- 29.Daniel L, Patrick W, Corey P, Judson B. Meditation-induced changes in high-frequency heart rate variability predict smoking outcomes, Frontiers in Human Neuroscience. 2012;6 doi: 10.3389/fnhum.2012.00054. DOI=103389/fnhum201200054, ISSN=1662-5161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 31.John C, Julie H. The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. The British journal of clinical psychology/the British Psychological Society. 2004;43:245–65. doi: 10.1348/0144665031752934. 101348/0144665031752934. [DOI] [PubMed] [Google Scholar]
- 32.Humboldt v, Monteiro S, Isabel LA. Validation of the PANAS: A Measure of Positive and Negative Affect for Use with Cross-National Older Adults. Review of European Studies. 2017;9 10 105539/resv9n2p10. [Google Scholar]
- 33.Yijing Z, Xiaoping D, Fang L, Xiaolu J, Bin W. The effects of guided imagery on heart rate variability in simulated spaceflight emergency tasks performers. BioMed Research International. 2015 doi: 10.1155/2015/687020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tyagi A, Cohen M. Yoga and heart rate variability: A comprehensive review of the literature. [[cited 2020 Mar 06]];Int J Yoga [serial online] 2016 9:97–113. doi: 10.4103/0973-6131.183712. Available from: http://wwwijoyorgin/textasp2016/9/2/97/183712 . [DOI] [PMC free article] [PubMed] [Google Scholar]


