Abstract
Anti-immigrant stigma or xenophobia is increasingly pervasive globally. Racism is a determinant of adverse health outcomes, but the epidemiological implications of the recent wave of xenophobic policies have not been well studied. The 2017 travel ban on individuals from Muslim majority countries is an example of such policy efforts in the United States. Using the 2009 – 2018 National Center for Health Statistics period linked infant birth-death data, we used time series methods to compare the monthly odds of preterm births to women from travel ban countries (Iran, Iraq, Libya, Somalia, Sudan, Syria, and Yemen) after the January 2017 travel ban to the number expected had the ban not been implemented. We estimated our counterfactual from the history of preterm birth among women born in countries included in the ban as well as trends in preterm birth among native-born non-Hispanic (NH) White women. Among the 18,945,795 singleton live births included in our study period (including 191,121 born to women from banned countries), the average monthly rate of births that were preterm birth was 8.5% (range: 6.8%, 10.6%) among women born in the countries affected by the ban and 8.6% (range: 7.7%, 9.8%) among native-born NH White women. Our results show an increase in the odds of preterm birth among infants born to women from travel ban countries in September 2017 and persisting through the cohort born in August 2018. The coefficient for exposed infants born in these months suggests that the odds of preterm birth increased by 6.8% among women from banned countries (p<0.001). Our results suggest that the first U.S. Executive Order (#13769) of the travel ban targeting individuals from Muslim majority countries may be associated with preterm births. We therefore conclude that structurally xenophobic and racist policies in the U.S. may have a harmful effect on birth outcomes and early life indicators of life-long health outcomes.
Keywords: birth weight, immigrants, infant health, prenatal stress, structural stigma, time series models
INTRODUCTION
As international migration has increased from 155 million migrants in 2000 to 227 million in 2019 (United Nations, 2020), migration policies have become increasingly hostile worldwide, from EU border control efforts to the US travel ban on individuals from Muslim majority countries. Globally, xenophobia and populism have fueled policies that are both anti-immigrant and anti-Islamic, creating widespread concern about associations with adverse health outcomes and the potential public health impacts (Juárez et al., 2019; Samari, 2016; Williams & Medlock, 2017). The potential effects of these policies are even more critical to examine in the wake of the COVID-19 pandemic, where migration policies have become increasingly restrictive, including a complete shutdown of the US asylum process. Despite the strong theoretical links (Samari, 2016; Samari et al., 2018), the health consequences of the recent wave of anti-Muslim xenophobia in the US have not yet been explored. One such opportunity to explore sociopolitical impacts on health is the travel ban on individuals from Muslim majority countries to the US on January 27, 2017, which was widely recognized as an acute instance of structural Islamophobia.
A growing literature examines the potential effects of anti-immigrant rhetoric and enforcement on migrant health (Juárez et al., 2019). Research in the US that focuses on Latinx immigrants documents links between immigration policy and residential choices, health care utilization, and food insecurity (Beniflah et al., 2013; Bohn & Pugatch, 2015; Potochnick et al., 2017). A smaller, but growing number of studies examine links between immigration enforcement and psychosocial well-being, self-rated health, and enforcement-related distress and stress-related health outcomes (Lopez et al., 2017; Rhodes et al., 2015; Sabo et al., 2014; White et al., 2014). Yet, a recent review finds that there remains a need to examine the differential health impacts of sociopolitical contexts, including policies, attitudes, and stigmatization, on migrants compared with non-migrants as well as whether effects differ amongst different migrant subgroups across a variety of health outcomes (Juárez et al., 2019).
Poor birth outcomes, such as preterm birth (< 37 weeks, PTB), are sensitive markers of temporally acute stressors from social and economic threats to war, hate crimes, and sociopolitical threats (Alhusen et al., 2016; Novak et al., 2017). In the US, studies have focused on sociopolitical stressors and birth outcomes since the 2016 Presidential election (Gemmill et al., 2019; Krieger et al., 2018), finding an increase in the rate of preterm birth among both native- and foreign-born Latina women following the election. Studies have also considered the effects of anti-immigrant legislation and enforcement on birth outcomes among US Latina immigrants (Novak et al., 2017; Torche & Sirois, 2018). One finds a 24% greater risk of low birth weight among births to Latina mothers following a federal immigration raid compared with births the year prior to the raid (Novak et al., 2017), and the other finds that the passage of restrictive immigration law in Arizona coincided with lower birth weight among children born to Latina immigrant women (Torche & Sirois, 2018). Among Arabic-named women there was a greater relative risk of poor birth outcomes compared to women without Arabic names following September 11, 2001, which could be attributed to discrimination and the corresponding stress (Lauderdale, 2006). It remains unclear whether these patterns extend to other immigrant subgroups, like immigrants from Muslim majority countries, who experience sociopolitical xenophobia across multiple dimensions of identity including race, religion, and nativity.
Despite the increasing need to understand the vulnerability of different immigrant groups in a variety of xenophobic contexts, with few exceptions (Agbemenu et al., 2019; Kane et al., 2018; Lauderdale, 2006; Mason et al., 2010), research on immigrant birth outcomes in the US focuses on Latinas and specifically, Mexican-born immigrants. This is partially due to the conflation of data from countries of origins with data on race/ethnicity in US health disparities research. For example, immigrants from the Middle East and North Africa (MENA) to the US are classified as non-Hispanic White in data on racial and ethnic disparities because of their racialization and classification as ‘White’ by the U.S. Office of Management and Budget and the U.S. Census (Office of Management and Budget, 1997; Tehranian, 2008). Therefore, sociopolitical health impacts and the relationship between structural racism and health among MENA origin groups are largely overlooked. Research on birth outcomes that does not disaggregate by country of origin will miss any potential disparity among certain immigrant groups, including immigrants from MENA.
Despite a growing literature showing that structural racism and specifically, anti-immigrant policies and rhetoric, are associated with low birth weight and preterm birth (Gemmill et al., 2019; Novak et al., 2017; Torche & Sirois, 2018), no previous studies have considered the impact of a policy that is both xenophobic and Islamophobic (anti-immigrant and anti-Muslim) on birth outcomes of women from Muslim majority countries. This question has gained significance as debates on bans and border walls have remained central to discussions of US immigration policy. In this study, we used national vital statistics data, and methods that control for seasonal and temporal patterns, to examine associations between the enactment of the 2017 ban on individuals from Muslim majority countries with preterm birth among women from those countries residing in the United States. We hypothesize that the Muslim ban was associated with greater than expected levels of preterm birth among gestations exposed in utero to the initial Muslim ban, which was signed on January 27, 2017.
METHODS
Data
We obtained restricted natality data for the years 2009 – 2018 from the U.S. National Center for Health Statistics. These data include comprehensive birth certificate information from all deliveries in the United States, as well as information on mother’s birth country that allowed us to identify foreign-born women from countries that were included in the initial Muslim Ban (i.e. Executive Order 13769). Women born in affected countries (Iran, Iraq, Libya, Somalia, Sudan, Syria, and Yemen) comprised our main exposure group. We also included native-born, non-Hispanic White women in our study as a comparison (e.g. “unexposed”) group. Our analysis required monthly counts of preterm (i.e., < 37 weeks gestation) and term live births to exposed and unexposed mothers. We defined gestational age based on the date of the last menstrual period, rather than the obstetric estimate (OE), because national natality data from NCHS did not fully transition to the OE-based measure until 2014 (Martin et al., 2015). All analyses were limited to singleton live births among resident mothers. We excluded births with non-viable or implausible gestational ages (<20 weeks gestation or >45 weeks gestation), as well as records with any missing information gestational age, plurality, and country of birth (<1% of records).
This research was determined exempt from human subjects review because it used aggregate data with de-identified information that is available upon request. Data was stored on a stand-alone computer that is fully encrypted and password protected per the data agreement with the U.S. National Center for Health Statistics.
Statistical Analysis
Our test, implemented with a comparative interrupted time-series design (Ralph Catalano & Serxner, 1987; Cook et al., 2008), proceeded through the following 8 steps.
-
1
For each month beginning with January 2009, we estimated the population at risk of preterm delivery among live births to mothers from the banned countries (exposed) as well as to native-born non-Hispanic White mothers (unexposed) in month t by summing the number of preterm births in month t, the number of all births in months t+1 and t+2, and the number of all births less preterm births in month t+3. We include births from months t, t+1, t+2, and t+3 because the conception cohort at risk of yielding preterm births in month t was likely born during those 4 months. Our estimates improve on the common practice of using all births, most of which will have gestational ages greater than 36 weeks, in month t to estimate the population at risk of preterm birth in that month. However, our estimate of the population at risk does not fully account for all fetuses at risk because monthly measures of miscarriage and other pregnancy outcomes are not available (Basso, 2020; Joseph, 2019).
We begin our study in January 2009 to include the entire Obama presidency in our study period. As evidenced by trends in hate crimes, this choice assumes that women from banned countries, as well as the communities in which these women are embedded, had adapted to a social and political environment during the Obama presidency that was considerably less threatening than that associated with the travel ban (Edwards & Rushin, 2018; Samari et al., 2018).
-
2
We calculated the monthly odds of preterm birth in exposed and unexposed mothers by dividing the number of preterm births by the difference between the population at risk (estimated in step 1) and the number of preterm births (i.e. calculated as the number of events that produce the outcome to the number that do not). Our 120 months of data yielded 117 cohorts because we could not estimate the population at risk for the last 3 cohorts of 2018 without data from the first 3 months of 2019, which we did not have at time of our analyses.
-
3
We transformed the monthly odds to natural logarithms to make their distributions more normal and to allow us to express any discovered associations as percentage change in the odds of preterm birth.
-
4
We regressed the log odds of preterm birth among exposed mothers on those among unexposed mothers to control for causes of preterm birth that, unlike the travel ban, could affect preterm birth rates among both groups of women, such as changes in clinical practice or record-keeping. We estimated the regression for 97 months (i.e., January 2009 through January 2017) before implementation of the ban.
-
5
We used Box-Jenkins (Box et al., 2015) methods to detect autocorrelation in the residuals of the regression estimated in step 4. These methods detect trends, cycles (e.g., seasonality), and the tendency for a series to remain elevated or depressed, or to oscillate, after high or low values. Any autocorrelation detected in this step would appear only among exposed mothers because the regression in step 4 would control that shared with unexposed mothers.
-
6
We specified and estimated a time-series regression, or “transfer function,” that predicted the log odds of preterm births to exposed mothers from those among unexposed mothers and from autocorrelation detected in Step 4. We estimated this transfer function for the 97 months prior to the implementation of the travel ban (i.e., from January 2009 through January 2017).
-
7
We applied the model and model coefficients estimated in step 6 to all 117 birth cohorts and used the methods of Alwan and Roberts (1988) to detect cohorts with observed values outside the 99.5% confidence interval of the values expected from the associations estimated from the 97 cohorts born before the start of the travel ban (i.e., before February 2017). We set the confidence at 99.5% because we infer support for our hypothesis if a sequence of high outlying birth cohorts appears among the 8 cohorts in gestation for less than 36 complete weeks in February 2017.
-
8
We added a binary variable scored 1 for any outlying cohorts detected by Alwan and Roberts (1988) methods and 0 otherwise to the transfer function developed in step 6 and estimated the model again for all 117 cohorts. The coefficient for the binary variable estimates the percentage increase in the odds of preterm birth among the cohorts in any outlying sequence detected by Alwan and Roberts (1988) methods.
RESULTS
Our analyses included 18,945,795 singleton live births from January 1, 2009, through December 31, 2018; 191,121 of these births were to women from banned countries. The average monthly rate of preterm birth was 8.5% (range: 6.8%, 10.6%) among women born in the countries affected by the ban and 8.6% (range: 7.7%, 9.8%) among native-born NH White women (Table 1). The average monthly rate of preterm birth remained the same for native-born NH White women following the ban, but increased to 8.6% among women born in affected countries. The corresponding average monthly odds of preterm birth are shown in Table 1.
Table 1.
Means and range of the monthly rate and odds of preterm birth among women affected by the travel ban and among native-born non-Hispanic White women. N = 117 months from January 2009 through September 2018, and stratified by months before ban and after the ban.
| All months: January 2009 - September 2018 | Before ban: January 2009 - December 2016 | After ban: February 2017 - September 2018 | ||||
|---|---|---|---|---|---|---|
| Mean | Range | Mean | Range | Mean | Range | |
| Preterm birth rate | ||||||
| Women affected by ban | 8.5% | (6.8%, 10.6%) | 8.5% | (6.8%, 10.6%) | 8.6% | (7.1%, 10.0%) |
| Native-born non-Hispanic White women | 8.6% | (7.7%, 9.8%) | 8.6% | (7.7%, 9.8%) | 8.6% | (8.1%, 9.1%) |
| Odds of preterm birth | ||||||
| Women affected by ban | 0.029 | (0.023, 0.036) | 0.029 | (0.023, 0.036) | 0.030 | (0.023, 0.036) |
| Native-born non-Hispanic White women | 0.029 | (0.026, 0.033) | 0.029 | (0.026, 0.033) | 0.029 | (0.027, 0.032) |
The first column of Table 2 presents model coefficients from Steps 5 and 6 of our study, which express the log odds of preterm birth among exposed mothers as a function of those among unexposed mothers and of autocorrelation for the 97 pre-ban birth cohorts. The autoregressive parameter a t-1 and moving average parameter at t-2 suggest that the odds of preterm birth among women born in the countries included in the ban exhibited autocorrelation different from that among cohorts born to native-born non-Hispanic White women. The tendency of high or low values at month t to remain elevated, or depressed, at t+1 and t+2 appears stronger among the former.
Table 2.
Coefficients and standard errors for Box-Jenkins pre-ban and final transfer functions predicting log odds of preterm birth among monthly cohorts born to mothers from banned countries.
| Pre-Ban Estimates 1/2009 through 1/2018 | Final Test Estimates 1/2009 through 9/2018 | |||
|---|---|---|---|---|
| Coefficient | S. E. | Coefficient | S. E. | |
| Log odds of preterm birth among non-Hispanic White women | 1.010** | .001 | 1.010** | .001 |
| Moving Average at t-2 | 0.590** | 0.086 | 0.565** | 0.081 |
| Autoregression at t-1 | −0.199* | 0.101 | −0.229* | 0.093 |
| Cohorts born from 9/2017 through 8/2018 | 0.068** | 0.010 | ||
p < 0.05, two-tailed test
p < 0.001, two-tailed test
Consistent with our hypothesis, Alwan and Roberts (1988) methods detected a sequence of unexpectedly high observed values beginning with infants born in September 2017 and persisting through the cohort born in August 2018. Figure 1 shows the observed (points) and expected (line) odds of preterm birth among women born in countries affected by the ban. The birth cohorts in the outlying sequence appear as X’s. Figure 2 shows our test results by plotting the observed less expected log odds over the test period.
Figure 1.
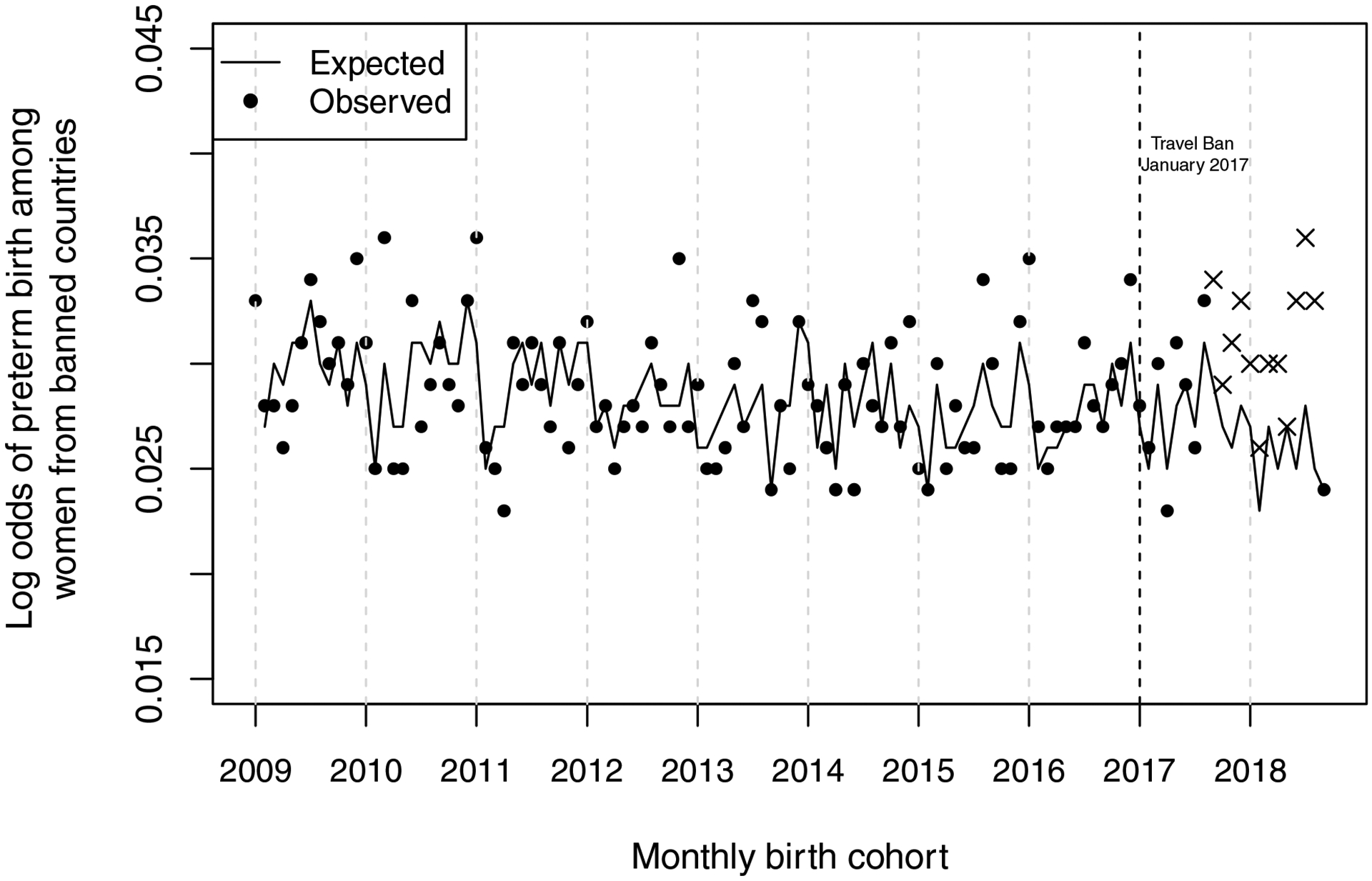
Observed (points) and expected (line) odds of preterm birth among 117 monthly cohorts (1/2009 through 9/2018) born to women born from banned countries. The birth cohorts in the outlying sequence appear as Xs.
Figure 2.
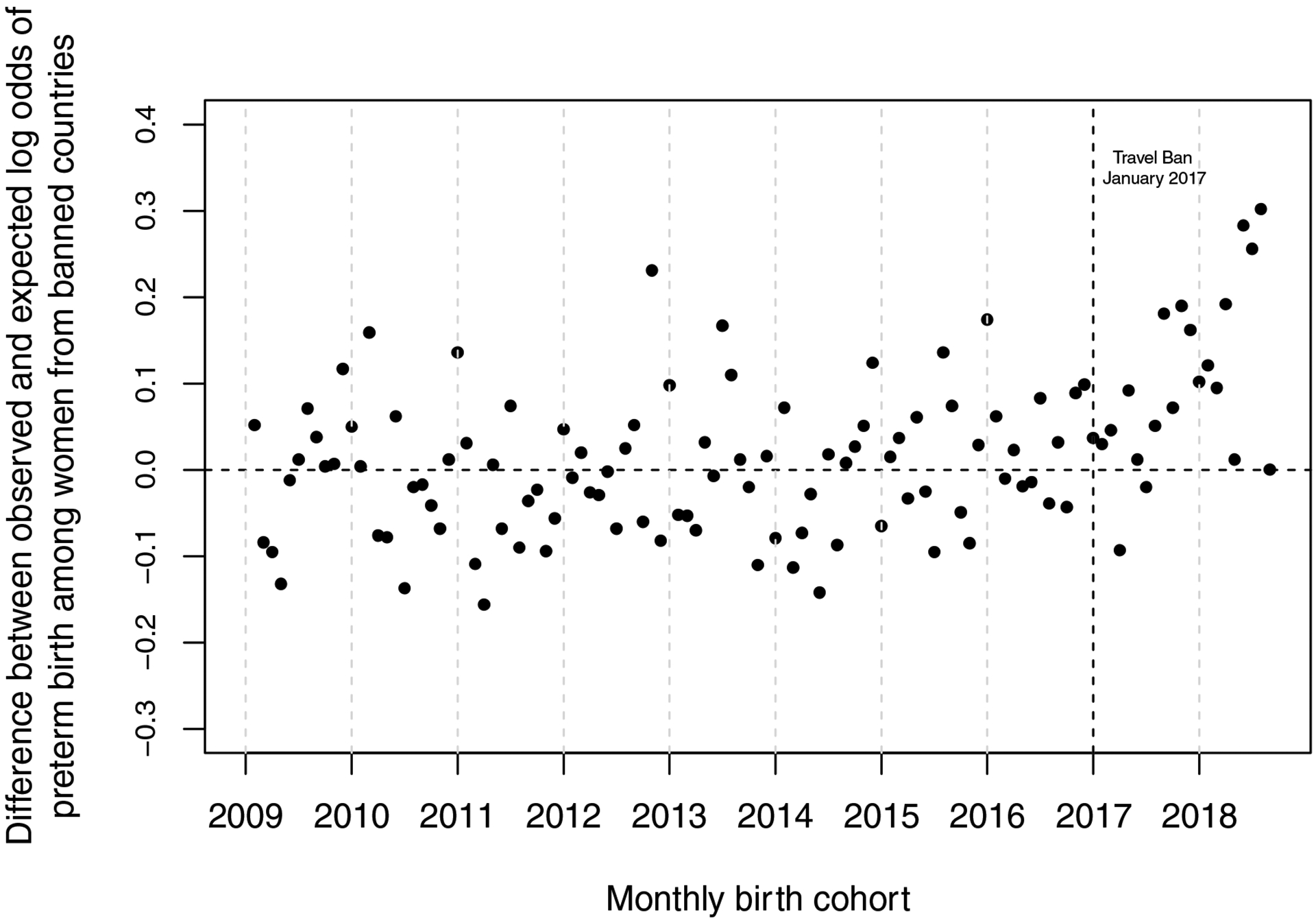
Difference between observed (points) and expected (line) log odds of preterm birth among 117 monthly cohorts (1/2009 through 9/2018) born to women born from banned countries.
The sequence of high outliers detected by the Alwan and Roberts methods could not arise from seasonality or other forms of autocorrelation (controlled by Box-Jenkins parameters), nor from any confounding phenomenon (controlled by the covariate) that also affected preterm births among non-Hispanic White mothers.
Based on the Alwan and Roberts (1988) results, we added a binary variable, scored 1 for the 12 outlying cohorts and 0 otherwise, to the pre-ban transfer function shown in the second column of Table 2 and estimated the model for all 117 cohorts. As shown in Table 2, the binary variable yielded a coefficient of 0.068 with a standard error of 0.010 (p<0.001). This coefficient implies that the odds of preterm birth among these cohorts were 6.8% higher than expected from the odds among non-Hispanic White women and from the history of preterm birth among women born in countries included in the ban.
DISCUSSION
Policies aimed at reducing social inequalities have a salutary effect on health indicators, infant mortality, and life expectancy at birth (Navarro et al., 2006). Therefore, it should not be surprising that xenophobic policies that aim to create social division and further inequality may have an adverse effect on pregnant women’s health and childbearing. This study provides new evidence about the importance of social characteristics of host countries and structurally stigmatizing contexts and reveals the potential public health implications of the global rise in xenophobia and populism. In particular, we find that women from countries impacted by the 2017 travel ban experienced a 6.8% increase in the odds of delivering a preterm infant between September 2017 and August 2018—a period that began approximately eight months after the executive order travel ban was enacted.
Given that past state-specific research has shown a low risk of preterm birth among Arab Americans in the U.S. (El-Sayed & Galea, 2009), the magnitude of increase in preterm birth among women from banned countries in the U.S. is concerning. The results indicate that even for populations that historically experience positive birth outcomes, anti-immigrant and Islamophobic policies are associated with abrupt and detrimental shifts in health outcomes. Prior research has also found elevated for risks for this population after adverse events; in the 6 months after September 11, for example, Arabic-named women were 34% more likely to have a low birthweight infant than during the pre-9/11 period. Thus, our findings add to a growing body of literature showing that sociopolitical stressors are yet another potentially contributing factor to maternal stress and adverse birth outcomes.
The literature suggests several pathways through which prenatal exposure to environmental stressors can affect birth outcomes, including mother’s physiological, neuroendocrine, and immune stress responses, which could affect the developing fetus (Dunkel Schetter, 2011). An important question that we cannot address with the available data is the mechanism(s) accounting for the negative relationship between the Muslim travel ban and preterm birth for women from banned countries in the U.S. A growing body of evidence suggests that the sociopolitical stress associated with the 2016 U.S. presidential election and exclusionary policies that followed led to increased levels of psychosocial stress, anxiety, and preterm births among U.S. immigrants and their co-ethnic family and community members (Eskenazi et al., 2019; Gemmill et al., 2019). Sociopolitical stress may manifest itself through pathways of uncertainty and fear, which have been found to be associated with poorer self-rated health (Patler et al., 2019) and inflammation (Martínez et al., 2018). Recent literature also highlights that anticipatory stress, or the anticipation of discrimination or xenophobia, can also have harmful health effects for immigrant women (García, 2018; Grace, 2020). These factors are linked to stress physiology and in turn, preterm birth (Goldenberg et al., 2008). Further, this stress may be exacerbated if women from banned counties avoided prenatal care out of fears of discrimination in the health care setting, stemming from the shift in the sociopolitical context brought about by the travel ban (Chu et al., 2019). We cannot discriminate among these pathways with the data available to us. Future research should attempt to disentangle these potential connections between sociopolitical stressors and adverse birth outcomes.
This study treated the 2017 travel ban as a discrete event by using Executive order 13769 on January 27, 2017 as the date of exposure. For this study, the fact that the effect of exposure to the travel ban’s passage may have been discrete is consistent with an acute stress response experienced during the early first trimester among immigrant mothers. The first trimester encompasses a critical period of gestation that may exhibit heightened vulnerability to maternal stress. For example, prior research (Bond et al., 2019; Zhu et al., 2010) indicates that women with higher levels of life events stress during the first trimester show elevated risks of preterm birth. A plausible mechanism for this observed relationship might be mediated through actions of the placenta, which undergoes critical development during this period, including impairments to the maternal-placental-fetal neuroendrocrine and immune systems (Wadhwa et al., 2011). There are, however, reasons to believe that exposure to the travel ban implementation was in fact a chronic exposure. The first seven months of 2017 included three different iterations of the travel ban, several court filings, protests, and media coverage related to the policy. Chronic stress exposure is also associated with preterm birth (Borders et al., 2007). Thus, the fact the adverse impact of the ban was not seen until months after the initial ban was enacted, may suggest that the accumulating nature of this sociopolitical stressor is of importance. Other plausible pathways for adverse birth outcomes among women from travel ban countries include economic hardship, change in diet, decline in access to and quality of care, and behavioral responses to anxiety and stress like alcohol consumption, that call for further investigation. A priority for future research includes considering the acute and chronic nature of the exposure as well as plausible pathways.
It is important to recognize the possibility of spillover effects of the travel ban on the birth outcomes in other immigrant groups. While this study focuses on women from countries named in the first executive order, it is plausible that there are effects on preterm birth among women from other MENA countries, all immigrant groups, and multiple generations of immigrants in the United States. In particular, the passage of the ban, along with other racist and anti-immigrant rhetoric, may have signaled increasing hostility to different groups of expectant mothers. Given the role of anticipatory stress in health outcomes (García, 2018; Grace, 2020), immigrant mothers as a whole could have internalized stress as a response to these structural policy changes. For an initial examination of the effect of xenophobic policies on birth outcomes, it was important to isolate the targeted populations from travel ban countries. However, future research should consider the implications for additional immigrant populations from MENA and around the world.
We acknowledge several limitations of this study. In order to test the effect of the policy, we rely on country of birth as a way to assess the exposure to the travel ban. The policy may or may not directly affect this group of women from banned countries, but country of origin provides a means of best approximating those impacted. Data that allows for identification of second-generation immigrants could further help approximate impacts on U.S. immigrant communities. We also did not use individual-level information that would otherwise allow us to identify maternal factors, political ideology for example, or gestational risk factors that interacted with the Ban to induce preterm birth. We note, however, that our findings unlikely emerged from a main effect of such risk factors. To spuriously induce our findings via a main effect, an unspecified risk factor would have affected gestations conceived only by women from the banned countries who conceived 20 to 36 weeks prior to ban. We know of no risk factors that could plausibly affect only those pregnancies. Moreover, lack of individual-level factors does not limit our ability to test the hypothesis we offer, nor reduce the contribution of our findings to estimating the health costs of immigration policy. We use a population-level test to answer a population-level question—did women from banned countries, when exposed to the Muslim Ban, produce more preterm births than expected from times prior to the Muslim Ban? The increase we detect was specific to women from banned countries and could not arise from seasonality or author forms of autocorrelation, nor could it occur from population-level shifts in preterm birth among all women giving birth.
Other limitations include that we were unable to examine time since migration, which is an important dimension to consider for birth outcomes (Teitler et al., 2017). We also did not account for other competing events, such as miscarriages or fetal deaths, that could influence our findings. In the case of the latter, however, we note that that if the Muslim Ban led to an increase in fetal loss, then our estimates of preterm birth are likely conservative, since selection in utero often targets small, frail fetuses, which may result in a more robust and healthier birth cohort (Bruckner & Catalano, 2018). Finally, given the small counts of preterm birth observed among women from banned countries, we were not able to examine fetal sex differences in vulnerability to the maternal stress response that have been reported in other studies (Gemmill et al., 2019; Wainstock et al., 2015; Walsh et al., 2019). Future research could explore the sex ratio of births or other sex-specific measures among politically stressed populations to explicitly test for effect modification by fetal sex (R. Catalano et al., 2006; Karasek et al., 2015; Retnakaran & Ye, 2020).
Despite these limitations, this study includes many strengths. First, this is a national-level examination of women from Muslim majority and Middle Eastern and North African countries, a population that is typically overlooked and understudied because of how religion and race and ethnicity are defined in health survey research. Other strengths of this study include our use of a quasi-experimental design and time series methods that rule out rival explanations of seasonality, trend, and other patterning of preterm births over time. Finally, our methodological approach presents a conservative test in that we include native-born MENA women in our “unexposed” group, even though this population might be similarly impacted by the ban, as described above.
The World Health Organization acknowledges that reducing preterm birth rates and improving the outcomes of preterm neonates remains a challenging task (Vogel et al., 2015). This study demonstrates that the current sociopolitical climate may hinder the global reduction of preterm birth. If Sustainable Development Goal 3 (SDG 3) to ensure healthy lives and promote wellbeing for all at all ages is to be achieved, the importance of migrant “regimes” in different destination contexts for immigrant pregnancy and birth outcomes cannot be ignored. Further as many countries continue to shut down migration systems because of the COVID-19 pandemic, it is important to understand the secondary and tertiary effects of such restrictions. This study, therefore, is an important contribution to the literature on xenophobia, structural racism, and health and perinatal demography for an often overlooked and understudied immigrant population. This work contributes to prior geographically-focused research by evaluating the impact of the 2017 travel ban on people from Muslim majority countries on preterm birth in the United States by using national vita statistics data from 2009 – 2018 and a quasi-experimental approach that controls for temporal variation. The trends described in this study suggest that policies that are both anti-immigrant and anti-Islamic have public health implications for pregnant women and infants. These estimates and trends might depict caution to policymakers throughout the world as they resist xenophobic and racist populist movements.
Highlights.
The 2017 U.S. Muslim travel ban policy is associated with preterm birth
Women from travel ban countries residing in the U.S. had higher odds of preterm birth
Trends in preterm birth remain unchanged for native-born non-Hispanic White women
Structurally xenophobic policies may have harmful effects on birth outcomes
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Agbemenu K, Auerbach S, Murshid NS, Shelton J, & Amutah-Onukagha N (2019). Reproductive Health Outcomes in African Refugee Women: A Comparative Study. Journal of Women’s Health, 28, 785–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhusen JL, Bower KM, Epstein E, & Sharps P (2016). Racial discrimination and adverse birth outcomes: an integrative review. Journal of midwifery & women’s health, 61, 707–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alwan LC, & Roberts HV (1988). Time-series modeling for statistical process control. Journal of Business & Economic Statistics, 6, 87–95. [Google Scholar]
- Basso O (2020). The fragile foundations of the extended fetuses at risk approach. Paediatric and Perinatal Epidemiology, 34, 80–85. [DOI] [PubMed] [Google Scholar]
- Beniflah JD, Little WK, Simon HK, & Sturm J (2013). Effects of immigration enforcement legislation on Hispanic pediatric patient visits to the pediatric emergency department. Clinical Pediatrics, 52, 1122–1126. [DOI] [PubMed] [Google Scholar]
- Bohn S, & Pugatch T (2015). US border enforcement and Mexican immigrant location choice. Demography, 52, 1543–1570. [DOI] [PubMed] [Google Scholar]
- Bond JC, Mancenido AL, Patil DM, Rowley SS, Goldberg J, & Littman AJ (2019). Residence change during the first trimester of pregnancy and adverse birth outcomes. Journal of Epidemiology and Community Health, 73, 913. [DOI] [PubMed] [Google Scholar]
- Borders AEB, Grobman WA, Amsden LB, & Holl JL (2007). Chronic stress and low birth weight neonates in a low-income population of women. Obstetrics & Gynecology, 109, 331–338. [DOI] [PubMed] [Google Scholar]
- Box GE, Jenkins GM, Reinsel GC, & Ljung GM (2015). Time series analysis: forecasting and control: John Wiley & Sons. [Google Scholar]
- Bruckner TA, & Catalano R (2018). Selection in utero and population health: Theory and typology of research. SSM - Population Health, 5, 101–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano R, Bruckner T, Marks AR, & Eskenazi B (2006). Exogenous shocks to the human sex ratio: the case of September 11, 2001 in New York City. Human reproduction, 21, 3127–3131. [DOI] [PubMed] [Google Scholar]
- Catalano R, & Serxner S (1987). Time series designs of potential interest to epidemiologists. American Journal of Epidemiology, 126, 724–731. [DOI] [PubMed] [Google Scholar]
- Chu DM, Aagaard J, Levitt R, Whitham M, Mastrobattista J, Rac M, et al. (2019). Cohort Analysis of Immigrant Rhetoric on Timely and Regular Access of Prenatal Care. Obstetrics & Gynecology, 133, 117–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook TD, Shadish WR, & Wong VC (2008). Three conditions under which experiments and observational studies produce comparable causal estimates: New findings from within study comparisons. Journal of Policy Analysis and Management: The Journal of the Association for Public Policy Analysis and Management, 27, 724–750. [Google Scholar]
- Dunkel Schetter C (2011). Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annual review of psychology, 62, 531–558. [DOI] [PubMed] [Google Scholar]
- Edwards GS, & Rushin S (2018). The effect of President Trump’s election on hate crimes. SSRN. [Google Scholar]
- El-Sayed AM, & Galea S (2009). Explaining the low risk of preterm birth among arab americans in the United States: an analysis of 617451 births. Pediatrics, 123, e438–e445. [DOI] [PubMed] [Google Scholar]
- Eskenazi B, Fahey CA, Kogut K, Gunier R, Torres J, Gonzales NA, et al. (2019). Association of perceived immigration policy vulnerability with mental and physical health among US-born Latino adolescents in California. JAMA pediatrics. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García SJ (2018). Living a Deportation Threat: Anticipatory Stressors Confronted by Undocumented Mexican Immigrant Women. Race and Social Problems, 10, 221–234. [Google Scholar]
- Gemmill A, Catalano R, Casey JA, Karasek D, Alcala HE, Elser H, et al. (2019). Association of Preterm Births Among US Latina Women With the 2016 Presidential Election. JAMA Network Open, 2, e197084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldenberg RL, Culhane JF, Iams JD, & Romero R (2008). Epidemiology and causes of preterm birth. The Lancet, 371, 75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace MK (2020). Status Variation in Anticipatory Stressors and Their Associations with Depressive Symptoms. J Health Soc Behav, 61, 170–189. [DOI] [PubMed] [Google Scholar]
- Joseph K (2019). Towards a unified perinatal theory: Reconciling the births based and fetus at risk models of perinatal mortality. Paediatric and Perinatal Epidemiology, 33, 101–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juárez SP, Honkaniemi H, Dunlavy AC, Aldridge RW, Barreto ML, Katikireddi SV, et al. (2019). Effects of non-health-targeted policies on migrant health: a systematic review and meta-analysis. The Lancet Global Health, 7, e420–e435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane JB, Teitler JO, & Reichman NE (2018). Ethnic enclaves and birth outcomes of immigrants from India in a diverse US state. Social Science & Medicine, 209, 67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karasek D, Goodman J, Gemmill A, Falconi A, Hartig T, Magganas A, et al. (2015). Twins Less Frequent Than Expected Among Male Births in Risk Averse Populations. Twin Research and Human Genetics, 18, 314–320. [DOI] [PubMed] [Google Scholar]
- Krieger N, Huynh M, Li W, Waterman PD, & Van Wye G (2018). Severe sociopolitical stressors and preterm births in New York City: 1 September 2015 to 31 August 2017. Journal of Epidemiology and Community Health, 72, 1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale DS (2006). Birth outcomes for Arabic-named women in California before and after September 11. Demography, 43, 185–201. [DOI] [PubMed] [Google Scholar]
- Lopez WD, Kruger DJ, Delva J, Llanes M, Ledon C, Waller A, et al. (2017). Health Implications of an Immigration Raid: Findings from a Latino Community in the Midwestern United States. Journal of immigrant and minority health, 19, 702–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JA, Osterman MJ, Kirmeyer SE, & Gregory EC (2015). Measuring Gestational Age in Vital Statistics Data: Transitioning to the Obstetric Estimate. Natl Vital Stat Rep, 64, 1–20. [PubMed] [Google Scholar]
- Martínez AD, Ruelas L, & Granger DA (2018). Household fear of deportation in relation to chronic stressors and salivary proinflammatory cytokines in Mexican-origin families post-SB 1070. SSM-population health, 5, 188–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason SM, Kaufman JS, Emch ME, Hogan VK, & Savitz DA (2010). Ethnic Density and Preterm Birth in African-, Caribbean-, and US-Born Non-Hispanic Black Populations in New York City. American Journal of Epidemiology, 172, 800–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navarro V, Muntaner C, Borrell C, Benach J, Quiroga Á, Rodríguez-Sanz M, et al. (2006). Politics and health outcomes. The Lancet, 368, 1033–1037. [DOI] [PubMed] [Google Scholar]
- Novak NL, Geronimus AT, & Martinez-Cardoso AM (2017). Change in birth outcomes among infants born to Latina mothers after a major immigration raid. International Journal of Epidemiology, 46, 839–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Management and Budget. (1997). Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity. Washington, DC: The White House. [Google Scholar]
- Patler C, Hamilton E, Meagher K, & Savinar R (2019). Uncertainty About DACA May Undermine Its Positive Impact On Health For Recipients And Their Children. Health Affairs, 38, 738–745. [DOI] [PubMed] [Google Scholar]
- Potochnick S, Chen J-H, & Perreira K (2017). Local-Level Immigration Enforcement and Food Insecurity Risk among Hispanic Immigrant Families with Children: National-Level Evidence. Journal of immigrant and minority health, 19, 1042–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Retnakaran R, & Ye C (2020). Outcome of the 2016 United States presidential election and the subsequent sex ratio at birth in Canada: an ecological study. BMJ Open, 10, e031208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, Mann L, Simán FM, Song E, Alonzo J, Downs M, et al. (2015). The impact of local immigration enforcement policies on the health of immigrant Hispanics/Latinos in the United States. American Journal of Public Health, 105, 329–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabo S, Shaw S, Ingram M, Teufel-Shone N, Carvajal S, de Zapien JG, et al. (2014). Everyday violence, structural racism and mistreatment at the US–Mexico border. Social Science & Medicine, 109, 66–74. [DOI] [PubMed] [Google Scholar]
- Samari G (2016). Islamophobia and Public Health in the United States. American Journal of Public Health, 106, 1920–1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samari G, Alcalá HE, & Sharif MZ (2018). Islamophobia, Health, and Public Health: A Systematic Literature Review. American Journal of Public Health, 108, e1–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tehranian J (2008). Whitewashed: America’s invisible middle eastern minority. New York City: NYU Press. [Google Scholar]
- Teitler J, Martinson M, & Reichman NE (2017). Does Life in the United States Take a Toll on Health? Duration of Residence and Birthweight among Six Decades of Immigrants. International Migration Review, 51, 37–66. [Google Scholar]
- Torche F, & Sirois C (2018). Restrictive Immigration law and birth outcomes of immigrant women. American Journal of Epidemiology, 188, 24–33. [DOI] [PubMed] [Google Scholar]
- United Nations. (2020). International Migration Report. In P.D. Department of Economic and Social Affairs (Ed.). New York, NY: United Nations Secretariat. [Google Scholar]
- Vogel JP, Oladapo OT, Manu A, Gülmezoglu AM, & Bahl R (2015). New WHO recommendations to improve the outcomes of preterm birth. The Lancet Global Health, 3, e589–e590. [DOI] [PubMed] [Google Scholar]
- Wadhwa PD, Entringer S, Buss C, & Lu MC (2011). The contribution of maternal stress to preterm birth: issues and considerations. Clinics in perinatology, 38, 351–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wainstock T, Shoham-Vardi I, Glasser S, Anteby E, & Lerner-Geva L (2015). Fetal sex modifies effects of prenatal stress exposure and adverse birth outcomes. Stress, 18, 49–56. [DOI] [PubMed] [Google Scholar]
- Walsh K, McCormack CA, Webster R, Pinto A, Lee S, Feng T, et al. (2019). Maternal prenatal stress phenotypes associate with fetal neurodevelopment and birth outcomes. Proceedings of the National Academy of Sciences, 116, 23996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K, Yeager VA, Menachemi N, & Scarinci IC (2014). Impact of Alabama’s immigration law on access to health care among Latina immigrants and children: implications for national reform. American Journal of Public Health, 104, 397–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Medlock MM (2017). Health Effects of Dramatic Societal Events - Ramifications of the Recent Presidential Election. N Engl J Med, 376, 2295–2299. [DOI] [PubMed] [Google Scholar]
- Zhu P, Tao F, Hao J, Sun Y, & Jiang X (2010). Prenatal life events stress: implications for preterm birth and infant birthweight. American Journal of Obstetrics & Gynecology, 203, 34.e31–34.e38. [DOI] [PubMed] [Google Scholar]


