Figure 1:
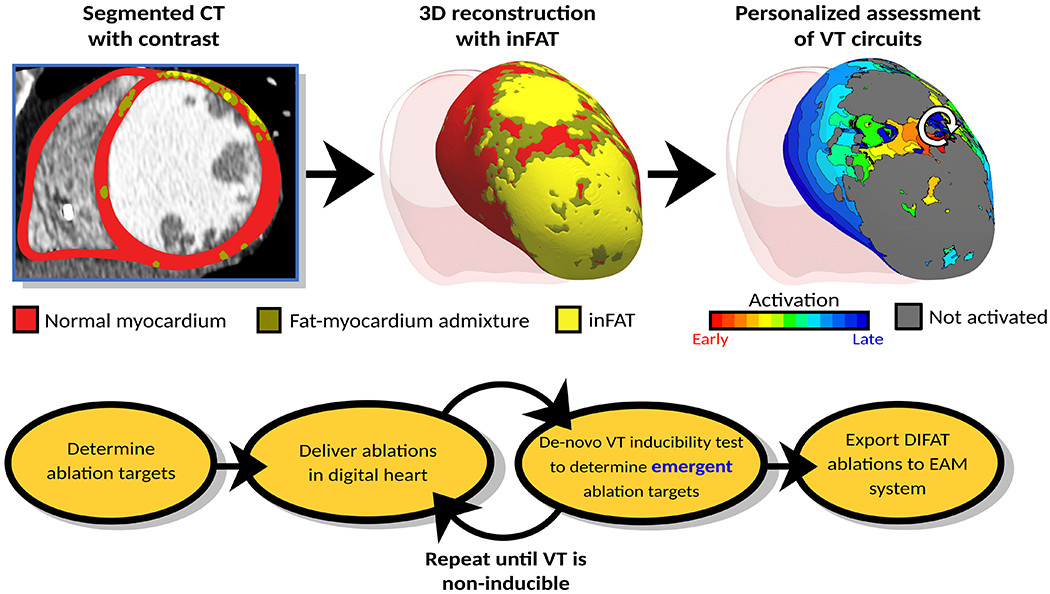
DIFAT Workflow. Top: From computed tomographic images with contrast, the myocardium is segmented into non-injured myocardium, inFAT, and fat-myocardium admixture. Personalized 3D digital hearts are reconstructed from this segmented data and electrophysiological information. inFAT-based arrhythmogenic propensity is assessed to identify all possible VTs the substrate can sustain. White arrow represents direction of induced reentrant propagation. Bottom: All VTs induced in the inFAT-based substrate are analyzed to determine minimum-size ablation targets. These ablation lesions are incorporated in the digital hearts as a mock-up of the clinical procedure. VT inducibility in the post-ablation digital hearts is tested again to determine whether emergent VTs arise in the new substrate. This process is repeated until complete VT non-inducibility is achieved in the personalized digital heart. The DIFAT ablations can then be imported into an EAM system to guide augment the ablation procedure. DIFAT: Digital-heart Identification of Fat-based Ablation Targets, EAM=electroanatomic mapping, inFAT=infiltrating adipose tissue, VT=ventricular tachycardia
