Figure 1.
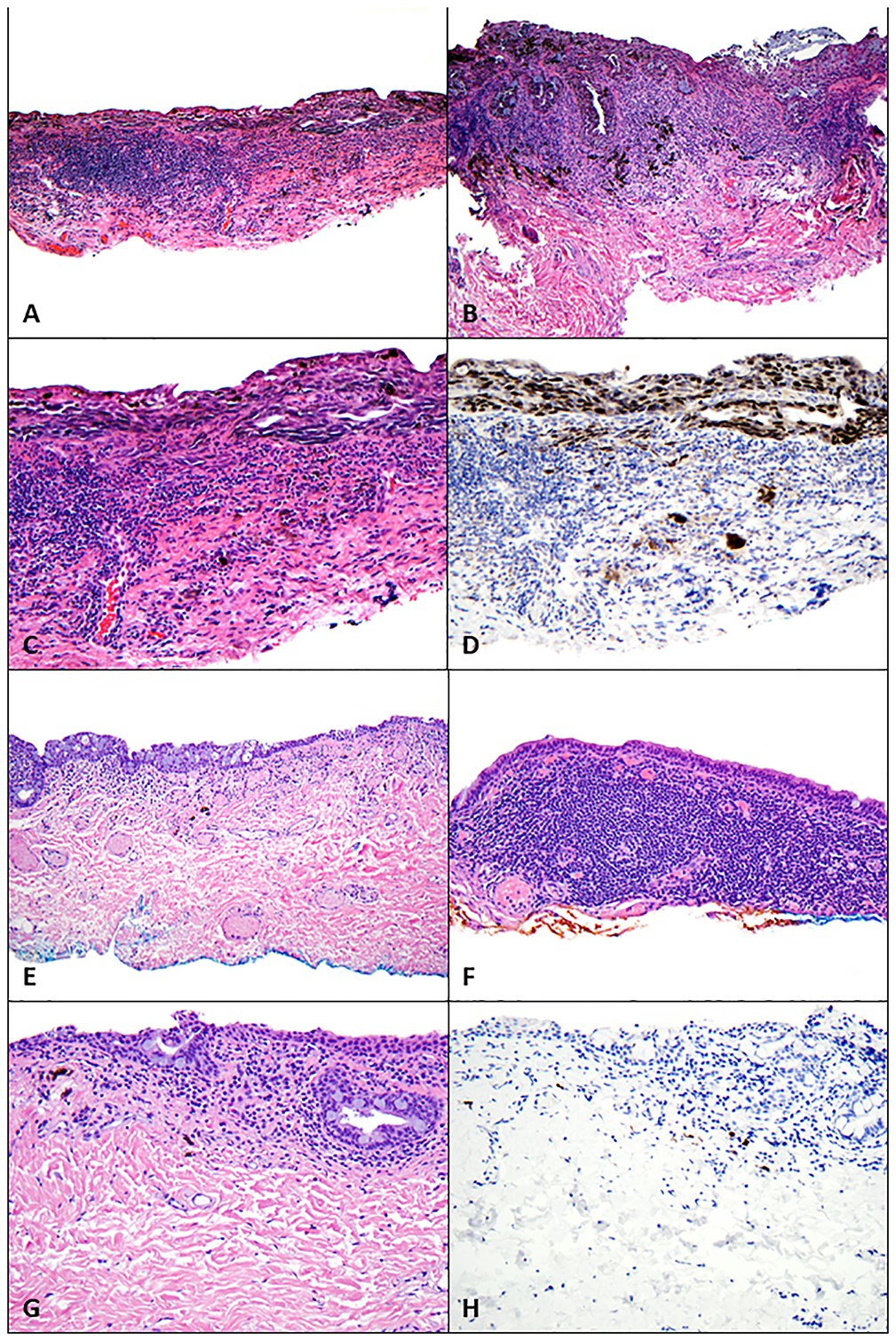
Findings on pathologic examination of conjunctival melanoma at least in situ with underlying regression before and after treatment with immune checkpoint blockade. (A-D) Before treatment with immune checkpoint blockade, biopsies revealed melanoma at least in situ with a dense subjacent lymphohistiocytic inflammatory infiltrate and pigmented macrophages (regression). (A) Scanning magnification shows extensive disease involving the conjunctiva (hematoxylin-eosin [H&E], 40x). (B) A confluent intraepithelial proliferation of atypical melanocytes extends along the glandular epithelium; also present are a dense underlying lymphohistiocytic inflammatory infiltrate and pigmented macrophages (H&E, 100x). (C, D) Atypical melanocytes line the basilar epithelium (C, H&E, 200x) and are highlighted with antibodies for Sox-10 (D, Sox-10, 200x); also present are scattered melanocytes amid the lymphohistiocytic inflammatory infiltrate, which were associated with keratin-positive epithelial cells and thus not interpreted as definitive invasion. (E-H) Following treatment with immune checkpoint blockade, biopsies revealed (E) conjunctiva with a variably dense lymphoplasmacytic inflammatory infiltrate and scattered pigmented macrophages (H&E, 40x). (F) The underlying lymphoplasmacytic inflammatory infiltrate was quite dense in some areas (H&E, 100x). (G) Higher-power magnification did not reveal melanocytes (H&E, 200x), and (I) absence of melanocytes was confirmed with immunohistochemical studies against Sox-10 (Sox-10, 200x).
