Abstract
Objective:
Previous studies of military veterans have produced mixed findings regarding whether combat exposure is directly related to suicidal ideation or is indirectly related to suicidal ideation via its influence on other factors. The present study used a longitudinal design to test the hypothesis that posttraumatic stress disorder (PTSD) symptom severity mediates the effect of combat exposure on suicidal ideation in veterans
Method:
Participants included 319 post-9/11 Veterans (83.4% male; 42.1% White/52.1% Black; Mage = 39.7) assessed at baseline, 6 months, and 12 months. Structural equation modeling and bootstrapped confidence intervals were employed to examine the direct and indirect relationships between combat exposure, suicidal ideation, and PTSD symptom severity.
Results:
Results from the mediation model, in which demographic variables and non-combat trauma were included as covariates, revealed that the indirect effect of combat exposure on suicidal ideation via PTSD symptom severity was statistically significant, accounting for 64.1% of the covariance between combat exposure and suicidal ideation.
Conclusions:
This study provides longitudinal evidence that the effects of combat exposure on suicidal ideation are mediated by PTSD symptom severity, suggesting the importance of targeting such symptoms in treatment to mitigate suicide risk among veterans with combat exposure.
Keywords: combat exposure, suicidal ideation, trauma, PTSD, veterans
Introduction
In the last 20 years, rates of suicide have increased by 33%, making suicide the 10th leading cause of death for all ages in the United States (Hedegaard, Curtin, & Warner, 2018). Among U.S. military veterans, suicide rates have demonstrated an even greater increase, as recent research has reported that the suicide rate is 50% higher among U.S. veterans as compared to U.S. non-veteran adults (Department of Veterans Affairs, 2019). Although researchers have theorized that the increase in suicide risk is associated with exposure to combat (e.g., Hoge & Castro, 2012; Ramchand, Acosta, Burns, Jaycox, & Pernin, 2011), support for this has been inconsistent (see Reger, Tucker, Carter, & Ammerman, 2018). In a large, longitudinal study of suicide risk among current and former military personnel, combat experience was not associated with suicide risk (LeardMann et al., 2013). Similarly, in a retrospective cohort study among all service members between 2001 and 2007, suicide mortality was not associated with deployment (Reger et al., 2015). Further, in a recent study of U.S. Army soldiers, combat exposure was negatively associated with suicidal ideation and attempts (Naifeh et al., 2019).
A meta-analysis by Bryan et al. (2015) found a significant relationship between combat exposure and suicidal ideation, attempts, and deaths; however, the effect size was very small, suggesting that other factors play a larger role in contributing to suicide risk. The authors of this meta-analysis proposed that these findings were consistent with the fluid vulnerability theory of suicide (Bryan & Rudd, 2006), which divides suicide risk into baseline and acute dimensions. According to fluid vulnerability theory, they posited the combat exposure may serve as a baseline, distal vulnerability factor for suicide but that other more proximal, acute variables (e.g., psychopathology, shame, guilt) play a more prominent role in predicting acute suicidal episodes.
Dillon and colleagues (2018) examined the relationship between combat exposure and suicidal thoughts and attempts in a cross-sectional sample of post-9/11 era veterans and found that combat exposure was indirectly related to suicidal ideation and attempts via a PTSD/depression latent variable. The results are in line with prior research showing a strong association between trauma-related distress and suicidal thoughts and attempts (Kimbrel et al., 2014; Kimbrel, Meyer, DeBeer, Gulliver, & Morissette, 2016). These results also support the fluid vulnerability theory, suggesting that combat exposure may be a distal predictor of suicidal ideation via increased posttraumatic symptom severity, a more proximal risk factor. The results from the study by Dillon and colleagues (2018) were informative, but were limited by the fact that the study was cross-sectional, making it impossible to determine the temporal direction of the relationships.
The objective of the current study was to further clarify the relationship between combat exposure and suicidal ideation in a longitudinal sample with post-9/11 era veterans. Specifically, the current study used a structural equation modeling (SEM) approach to test the hypothesis that self-reported combat exposure assessed at baseline would be associated with PTSD symptom severity assessed six months later, which would, in turn, be associated with suicidal ideation at 12 months. We also hypothesized that the indirect effect of combat exposure on suicidal ideation via PTSD symptoms would be significant. To our knowledge, this is the first study to use a longitudinal design to test these hypotheses.
Method
Participants and Procedures
The current analyses were conducted using data from a larger longitudinal study of veterans’ psychological health (N = 319). Institutional Review Board approval was obtained prior to data collection. In the parent study, data were collected at baseline (Time 1 [T1]), 6-month follow-up (Time 2 [T2]), and 12-month follow-up (Time 3 [T3]) time points between June of 2009 and March of 2013. English-speaking veterans between the ages of 18 and 70 who served in the military after September 11, 2001 were recruited through advertisements, clinician referrals, and mailings to participants enrolled in a large, multi-site study of post-deployment mental health (Brancu et al., 2017). Veterans initiated participation by calling the study phone line and completing a brief telephone screening. There were no psychiatric or medical exclusionary criteria. If eligible, veterans were scheduled for in-person data collection at the Durham VA Health Care System. After providing written informed consent, clinical interviews and self-report measures were administered. Veterans were compensated for participation at each assessment session.
Measures
The Combat Exposure Scale (CES; Keane et al., 1989) was administered at T1 to assess past exposure to various combat situations. The CES is a 7-item self-report measure in which respondents rate items on a 5-point Likert scale (1 to 5) reflecting frequency, duration, or degree of loss of combat exposure. The CES has been used in other research with post-9/11 era veterans and demonstrated good internal consistency (α = 0.88; Dillon et al., 2018). Similarly, for the current sample, internal consistency for the CES at baseline was 0.85. The mean CES score was 11.54 (SD = 10.84; range = 0–41).
The Beck Scale for Suicide Ideation (SSI; Beck & Steer, 1991) was used to assess current suicidal thoughts and behaviors at T3. The SSI is a 20-item self-report questionnaire in which respondents rate the severity of suicidal ideation, plans, and preparations during the past week on a 3-point Likert scale (0 to 2, with higher values indicating greater severity). For the current study, Item 20, which asked about the presence of a past suicide attempt, was excluded from the total score to ensure the SSI captured only current thoughts. Internal consistency reliability for the SSI at Time 3 was good (α = .83). The mean SSI score was 0.52 (SD = 2.07; range = 0–19).
The Davidson Trauma Scale (DTS; Davidson et al., 1997) was used at T2 to assess severity of PTSD symptoms during the past week. The DTS is a 17-item questionnaire that assesses the 17 DSM-IV symptoms of PTSD. Respondents rate the frequency and severity of each item regarding their most bothersome traumatic event on a 5-point Likert scale (0 to 4). Internal consistency in the present study for total symptom severity at T2 was excellent (α = .98). The mean DTS score was 37.47 (SD = 35.40; range = 0–131).
The Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000) was used at T1 to quantify the extent of non-combat trauma experienced by each participant. The TLEQ is a self-report questionnaire that assesses exposure to 22 types of potentially traumatic events (e.g., combat, childhood sexual assault, childhood violence, adult sexual assault, accident) Non-combat trauma was assessed by summing up the number of non-combat trauma items endorsed by a given participant. The mean TLEQ score (not including combat) was 3.55 (SD = 3.22; range = 0–16).
Data Analysis
Structural equation modeling was used to test the hypothesis that PTSD symptom severity mediates the association between combat exposure and suicidal ideation.1 Consistent with MacKinnon’s approach to testing mediation (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002), we constructed a path model examining the effect of combat exposure (assessed retrospectively at T1) on T2 PTSD symptom severity (Path A), and the effect of T2 PTSD symptom severity on T3 suicidal ideation (Path B) independent of the effect of T1 combat exposure (Path C’). The indirect, or mediation, effect of combat exposure on suicidal ideation was calculated as the product of Paths A and B. Age, gender, race, and non-combat trauma exposure were covaried in the path model. To test the significance of mediation, bootstrapped confidence intervals around the indirect effect of combat exposure on suicidal ideation were generated using resampling. This method offers an advantage over conventional tests, such as Sobel’s z, because it takes into account the positive skew inherent to indirect effects (Preacher & Hayes, 2008). As such, bootstrapping methods are more powerful than conventional tests, with mediation deemed significant when the resulting confidence interval does not span 0. In the present analyses, 5,000 resamples were used to generate empirically derived 95% confidence intervals. All analyses were conducted using maximum likelihood estimation, which is robust to data missing at random, available in Mplus 7 (Muthén & Muthén, 2012).
Results
A total of 313 veterans had at least partial T1 data available for analysis. Of these, 245 (78.3%) had at least partial T2 data on PTSD symptoms, and 197 (62.9%) had at least partial T3 data on suicidal ideation. Participants were mostly male (83.4%), middle-aged (mean age at baseline = 39.70, SD = 10.61, range = 21 to 67 years), and either Black or White (n = 162 Black, 52.1%; n = 131 White, 42.1%; n = 18 [i.e., Asian, Native American, Pacific Islander, multiracial, other], 5.8%). None of the model variables were predictors of missing data at T2 (all ps > .32). Participants missing data at T3 were younger, t(311) = 2.25, p = .025, and had experienced more intense combat, t(309) = 3.29, p = .001 than those who had not. No other variables were predictors of missing data at T3 (all ps > .32).
The results of the path analysis are depicted in Figure 1. According to those, the total effect of T1 combat exposure on T3 suicidal ideation was moderate and significant (β = .24, p < .001). In turn, T1 combat exposure was also a strong predictor of T2 PTSD symptom severity (β = .46, p < .001), which was a moderate predictor of T3 suicidal ideation (β = .33, p = .001). With T2 PTSD symptom severity in the model, the direct effect of combat exposure on suicidal ideation was rendered non-significant (β = .09, p = .21). According to the bootstrapped analysis, the indirect effect of T1 combat exposure on T3 suicidal ideation via T2 PTSD symptom severity was significant, β = .15 (95% CI: .06 –.24), accounting for 64.1% of the covariance between combat exposure and suicidal ideation.
Figure 1.
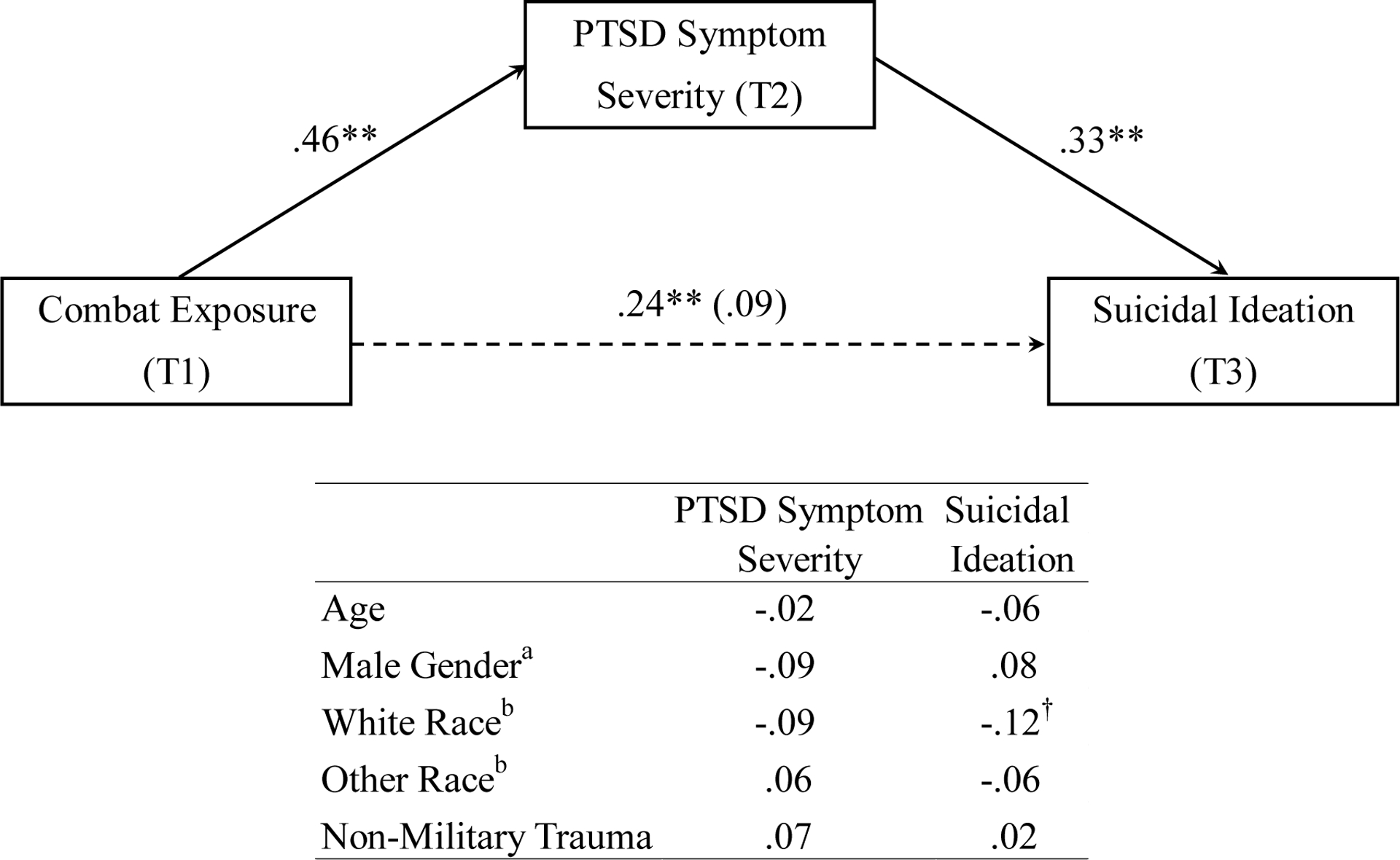
Structural equation model of suicidal ideation. The total (unadjusted) and direct adjusted effect (in parentheses) of combat exposure on suicidal ideation are depicted. All effects are standardized. Covariate effects are presented in the table. The dotted line represents the mediated pathway. †p < .10, **p < .01, aFemale gender was set as the reference group. bBlack race was set as the reference group.
Discussion
The aim of the present study was to use longitudinal data from a veteran sample to clarify the mixed findings regarding the nature of the association between combat exposure and suicidal ideation. Using three assessment time points (baseline, 6-month follow-up, and 12-month follow-up), results from a mediation model supported the hypothesis that combat exposure indirectly affects suicidal ideation via trauma-related symptoms (severity of current PTSD symptoms). This finding adds new evidence to the growing number of cross-sectional studies implicating mental health symptom severity as an important mechanism by which combat exposure exerts its effect on suicidal ideation (e.g., Dillon et al., 2018; Maguen et al., 2011). This is the first study, to our knowledge, to test the mediating effects of current PTSD symptoms using a longitudinal design.
Exposure to military combat has long been thought to increase suicide risk (e.g., Hoge & Castro, 2012; Ramchand et al., 2011). However, a number of prior studies among military service members and veterans have not found a consistent association (LeardMann et al., 2013; Naifeh et al., 2019; Reger et al., 2015), including a meta-analysis that found a significant but weak relationship (Bryan et al., 2015). This literature suggests that the association between combat exposure and suicidal thoughts/attempts, if any, is likely complex and potentially mediated by other related but distinct factors. In line with the framework of the fluid vulnerability theory of suicide (Bryan & Rudd, 2006), which distinguishes between distal and proximal influences on suicide risk, Dillon and colleagues (2018) found support for the hypothesis that combat exposure serves as a distal factor that indirectly increases suicidal thoughts and attempts via the proximal influence of PTSD and depressive symptoms.
The current study reaches similar conclusions to Dillon and colleagues (2018), with a particular focus on PTSD symptoms, but has several methodological advantages that allow for more robust testing of the hypothesis. First, in contrast to cross-sectional examinations by Dillon et al. (2018) and others (e.g., Bryan, Hernandez, Allison, & Clemans, 2013), the longitudinal design of this study made it possible to clarify the direction of associations between variables and to ensure that the mediator (i.e., PTSD symptoms) temporally preceded the outcome variable (i.e., suicidal ideation), a key assumption of formal mediation (see Kazdin & Nock, 2003). Second, and related, whereas Dillon et al. (2018) included lifetime or historical symptomatology in the construction of latent variables (e.g., lifetime PTSD diagnosis, past suicide attempt), the current study used only current or very recently experienced symptoms. This approach not only establishes the temporal relationship between variables but also more cleanly fits within the fluid vulnerability theory framework by directly testing the hypothesis that combat exposure is a distal influence on subsequent suicidal ideation through the proximal influence of current posttraumatic symptoms. The present study thereby provides a compelling mechanistic account for a way in which combat exposure may affect suicidal ideation.
The findings of this study have clinical implications. Results suggest that clinicians working with combat-exposed veterans should explore the extent to which these individuals are currently distressed by this exposure, rather than only focusing on the severity of exposure itself, when determining potential suicide risk. Though preliminary, these findings also indicated that reducing PTSD symptoms associated with combat exposure may lead to a reduction in suicidal ideation. The relationship between combat exposure and suicide appears complex, and prior research suggests there are likely multiple treatment pathways to reducing suicide risk. These include targeting issues associated with specific types of combat, such as moral injury (Maguen et al., 2012; Wisco et al., 2017), or specific types of trauma-related symptomatology (Gradus, Suvak, Wisco, Marx, & Resick, 2013), such as depressive symptoms (Kumpula et al., 2019) and guilt/shame (Cunningham, Davis, Wilson, & Resick, 2017).
The current study had several limitations. First, the longitudinal design of the study was able to establish the temporal order of variables and thereby allowed for more rigorous testing of statistical mediation. However, one of the key variables, combat exposure, was assessed retrospectively at baseline. Given the length of time between combat/deployment and baseline assessment likely varied between individuals (though such information was not accessible in this dataset), it is possible the mediating effect of PTSD on suicide ideation varies as a function of time since trauma exposure. Additionally, prior research has found that reports of trauma exposure can vary as a function of PTSD severity (e.g., Roemer, Litz, Orsillo, Ehlich, & Friedman, 1998). Future research that systematically accounts for such periods of time since combat/deployment and variations in self-reported, retrospective combat exposure over time could provide greater clarity on the particular dynamics of these relationships. Second, though a strength of the study was the sample’s ethnic diversity, with black veterans accounting for nearly half of all participants, the sample was mostly male. Though the models controlled for age and gender, prior research has suggested there are key differences in trauma exposure and symptoms as a function of gender (e.g., Luxton, Skopp, & Maguen, 2010), and it will be important to see if these and other demographic variables affect the relationship between combat exposure and suicidal ideation. Third, the PTSD assessment that was used was based on DSM-IV. Future studies are needed to replicate these findings using a DSM-5 PTSD assessment. Fourth, given the low base rates of suicide attempts and deaths, it was not possible to examine the mediating effect of posttraumatic symptom severity on suicide attempts. Future studies are needed to examine whether similar patterns are observed for suicide attempts as they are suicidal thoughts. Lastly, there was participant attrition (37%), which may have impacted results. This is a common limitation of longitudinal research designs and our rate of attrition was within the range of other studies in veteran populations (58 – 21%, respectively; Benotsch et al., 2000; McAndrew et al., 2018).
The current study extends prior research by helping to clarify the relationship between combat exposure and suicidal ideation and is the first to offer longitudinal evidence that combat exposure indirectly affects suicidal ideation through the mediation of PTSD symptom severity. Taken together, the findings of this study suggested that clinicians and researchers should be aware of the indirect effects of combat exposure on suicidal ideation and offer preliminary evidence to suggest that targeting posttraumatic symptoms in treatment may help mitigate the effects of trauma exposure and thereby reduce suicide risk. Future research is needed to further clarify the causal nature of these complex relationships as a means to provide useful targets for treatment.
Acknowledgements
This work was supported by the Department of Veterans Affairs’ (VA) Mid-Atlantic Mental Illness Research, Education, and Clinical Center (MIRECC), Rehabilitation Research and Development Service of the VA, and the Research and Development and Mental Health Services of the Durham VA Health Care System. Dr. Beckham was supported by a Senior Research Career Scientist award (1K6BX003777) from Clinical Sciences Research and Development Service of VA Office of Research and Development (VA ORD). Dr. Elbogen was supported by a grant (R01MH080988) from the National Institute of Mental Health. Dr. Dillon was supported by a Career Development Award (IK2RX002965) from the Rehabilitation Research and Development Service of VA ORD. Manuscript preparation was partially supported by the VA Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment (Glenn). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the United States government or any of the institutions with which the authors are affiliated.
Footnotes
Given prior research indicating a high co-occurrence of PTSD and depression (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995) and that the PTSD and depression may load onto a higher-order “distress” factor (Cox, Clara, & Enns, 2002; Miller, Fogler, Wolf, Kaloupek, & Keane, 2008), initial efforts were made to capture PTSD and depressive symptoms (using the Beck Depression Inventory-II ; Beck, Steer, & Brown, 1996) in a single latent variable, similar to (Dillon et al., 2018), using the four DTS scales and two BDI scales. However, fit statistics of the resulting model were borderline in terms of acceptability (RMSEA = .09, CFI = 0.99, SRMR = .02, and χ2(6) = 21.15, p = .002). Therefore, to ensure a proper measurement model, the decision was made to focus on PTSD symptom severity separate from depression.
References
- Beck AT, & Steer RA (1991). Manual for Beck Scale for Suicide Ideation. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Beck AT, Steer RA, & Brown G (1996). Beck Depression Inventory-II. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Benotsch EG, Brailey K, Vasterling JJ, Uddo M, Constans JI, & Sutker PB (2000). War Zone stress, personal and environmental resources, and PTSD symptoms in Gulf War Veterans: A longitudinal perspective Journal of Abnormal Psychology, 109, 205. [PubMed] [Google Scholar]
- Bryan CJ, Griffith JE, Pace BT, Hinkson K, Bryan AO, Clemans TA, & Imel ZE (2015). Combat exposure and risk for suicidal thoughts and behaviors among military personnel and veterans: A systematic review and meta-analysis. Suicide and Life-Threatening Behavior, 45(5), 633–649. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Hernandez AM, Allison S, & Clemans T (2013). Combat exposure and suicide risk in two samples of military personnel. Journal of Clinical Psychology, 69(1), 64–77. doi: 10.1002/jclp.21932 [DOI] [PubMed] [Google Scholar]
- Bryan CJ, & Rudd MD (2006). Advances in the assessment of suicide risk. Journal of Clinical Psychology, 62(2), 185–200. doi: 10.1002/jclp.20222 [DOI] [PubMed] [Google Scholar]
- Cunningham KC, Davis JL, Wilson SM, & Resick PA (2017). A relative weights comparison of trauma-related shame and guilt as predictors of DSM-5 posttraumatic stress disorder symptom severity among US veterans and military members. British Journal of Clinical Psychology, 57(2), 163–176. doi: 10.1111/bjc.12163 [DOI] [PubMed] [Google Scholar]
- Davidson JRT, Book SW, Colket JT, Tupler LA, Roth S, David D, … Feldman ME (1997). Assessment of a new self-rating scale for posttraumatic stress disorder: The Davidson Trauma Scale. Psychological Medicine, 27, 153–160. [DOI] [PubMed] [Google Scholar]
- Department of Veterans Affairs. (2018). Veteran Suicide Data Report, 2005–2016. Retrieved from https://www.mentalhealth.va.gov/docs/data-sheets/OMHSP_National_Suicide_Data_Report_2005-2016_508-compliant.pdf
- Dillon KH, Cunningham KC, Neal JM, Wilson SM, Dedert EA, Elbogen EB, … Kimbrel NA (2018). Examination of the indirect effects of combat exposure on suicidal behavior in veterans. Journal of affective disorders, 235, 407–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gradus JL, Suvak MK, Wisco BE, Marx BP, & Resick PA (2013). Treatment of posttraumatic stress disorder reduces suicidal ideation. Depression and Anxiety, 30(10), 1046–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H, Curtin SC, & Warner M (2018). Suicide mortality in the United States, 1999–2017. Retrieved from Hyattsville, MD: [PubMed] [Google Scholar]
- Hoge CW, & Castro CA (2012). Preventing suicides in US service members and veterans: concerns after a decade of war. The Journal of American Medical Association, 308(7), 671–672. doi: 10.1001/jama.2012.9955 [DOI] [PubMed] [Google Scholar]
- Kazdin AE, & Nock MK (2003). Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry, 44(8), 1116–1129. [DOI] [PubMed] [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT, Taylor KL, & Mora CA (1989). Clinical evaluation of a measure to assess combat exposure. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 1, 53–55. doi: 10.1037/1040-3590.1.1.53 [DOI] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of general psychiatry, 52(12), 1048–1060. [DOI] [PubMed] [Google Scholar]
- Kimbrel NA, Evans LD, Patel AB, Wilson LC, Meyer EC, Gulliver SB, & Morissette SB (2014). The critical warzone experiences (CWE) scale: Initial psychometric properties and association with PTSD, anxiety, and depression. Psychiatry research, 220(3), 1118–1124. doi: 10.1016/j.psychres.2014.08.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Meyer EC, DeBeer BB, Gulliver SB, & Morissette SB (2016). A 12-month prospective study of the effects of PTSD-depression comorbidity on suicidal behavior in Iraq/Afghanistan-era veterans. Psychiatry research, 243, 97–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumpula MJ, Wagner HR, Dedert EA, Crowe CM, Day KT, Powell K, … Kimbrel NA (2019). An evaluation of the effectiveness of evidence-based psychotherapies for depression to reduce suicidal ideation among male and female veterans. Women’s Health Issues, 29, S103–S111. [DOI] [PubMed] [Google Scholar]
- LeardMann CA, Powell TM, Smith TC, Bell MR, Smith B, Boyko EJ, … Hoge CW (2013). Risk factors associated with suicide in current and former US military personnel. Journal of American Medical Assocation, 310(5), 496–506. doi: 10.1001/jama.2013.65164 [DOI] [PubMed] [Google Scholar]
- Luxton DD, Skopp NA, & Maguen S (2010). Gender differences in depression and PTSD symptoms following combat exposure. Depression and Anxiety, 27(11), 1027–1033. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7(1), 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguen S, Metzler TJ, Bosch J, Marmar CR, Knight SJ, & Neylan TC (2012). Killing in combat may be independently associated with suicidal ideation. Depression and Anxiety, 29(11), 918–923. doi: 10.1002/da.21954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAndrew LM, Helmer DA, Lu SE, Chandler HK, Slotkin S, & Quigley KS (2018). Longitudinal relationship between onset of physical symptoms and functional impairment. Journal of behavioral medicine, 41, 819–826. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2012). Mplus User’s Guide. Seventh Edition In. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Naifeh JA, Mash HBH, Stein MB, Fullerton CS, Kessler RC, & Ursano RJ (2019). The Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS): Progress toward understanding suicide among soldiers. Molecular Psychiatry, 24(1), 34–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- Ramchand R, Acosta J, Burns RM, Jaycox LH, & Pernin CG (2011). The war within: Preventing suicide in the U.S. military. Rand Health Quarterly, 1(1), 2 Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/28083158 [PMC free article] [PubMed] [Google Scholar]
- Reger MA, Smolenski DJ, Skopp NA, Metzger-Abamukang MJ, Kang HK, Bullman TA, … Gahm GA (2015). Risk of suicide among US military service members following Operation Enduring Freedom or Operation Iraqi Freedom deployment and separation from the US military. JAMA Psychiatry, 72(6), 561–569. [DOI] [PubMed] [Google Scholar]
- Reger MA, Tucker RP, Carter SP, & Ammerman BA (2018). Military deployments and suicide: A critical examination. Perspectives on Psychological Science, 13(6), 688–699. [DOI] [PubMed] [Google Scholar]
- Wisco BE, Marx BP, May CL, Martini B, Krystal JH, Southwick SM, & Pietrzak RH (2017). Moral injury in U.S. combat veterans: Results from the national health and resilience in veterans study. Depression & Anxiety, 34(4), 340–347. doi: 10.1002/da.22614 [DOI] [PubMed] [Google Scholar]


