Significance
Achieving universal health care access is a key development priority and a target of Sustainable Development Goal number 3. The COVID-19 pandemic has only reinforced this urge. A rapid expansion of public, affordable health care infrastructure is particularly crucial in sub-Saharan Africa (SSA): communicable diseases are the first cause of death, infant mortality rates are above 5%, and lengthy journeys to health care facilities undermine the accessibility to basic health care for millions. This paper provides a planning-oriented, inequality-focused analysis of health care accessibility in SSA based on a state-of-the-art georeferenced database of public health care facilities. We devise a spatial optimization framework to identify the optimal location and required bed capacity of public health care facilities in the region.
Keywords: public health care, accessibility, inequality, GIS algorithm, sub-Saharan Africa
Abstract
Achieving universal health care coverage—a key target of the United Nations Sustainable Development Goal number 3—requires accessibility to health care services for all. Currently, in sub-Saharan Africa, at least one-sixth of the population lives more than 2 h away from a public hospital, and one in eight people is no less than 1 h away from the nearest health center. We combine high-resolution data on the location of different typologies of public health care facilities [J. Maina et al., Sci. Data 6, 134 (2019)] with population distribution maps and terrain-specific accessibility algorithms to develop a multiobjective geographic information system framework for assessing the optimal allocation of new health care facilities and assessing hospitals expansion requirements. The proposed methodology ensures universal accessibility to public health care services within prespecified travel times while guaranteeing sufficient available hospital beds. Our analysis suggests that to meet commonly accepted universal health care accessibility targets, sub-Saharan African countries will need to build ∼6,200 new facilities by 2030. We also estimate that about 2.5 million new hospital beds need to be allocated between new facilities and ∼1,100 existing structures that require expansion or densification. Optimized location, type, and capacity of each facility can be explored in an interactive dashboard. Our methodology and the results of our analysis can inform local policy makers in their assessment and prioritization of health care infrastructure. This is particularly relevant to tackle health care accessibility inequality, which is not only prominent within and between countries of sub-Saharan Africa but also, relative to the level of service provided by health care facilities.
Health care facilities in sub-Saharan African countries are facing a rising pressure from growing populations (1) and the emergence of infectious diseases such as the recent outbreaks of Ebola (2) and COVID-19 (3). Uneven distribution of health care accessibility, in addition to limited public health financial resources and other fiscal constraints, calls for better planning for the next generation of health care facilities. This paper aims to improve the understanding of inequality in health care accessibility in sub-Saharan Africa (SSA) by assessing the current status and proposing an optimal allocation of new health care facilities and expansion needs through a state-of-the-art geographic information system (GIS) optimization framework.
Our contribution counts toward the United Nations Sustainable Development Goal number 3 (SDG 3), which aims at ensuring healthy lives and promoting well-being for all (4). Through its targets, SDG 3 envisions reducing mortality, eradicating epidemics, and most importantly, achieving universal health care coverage. This includes secure provision of health care services, medicines, and vaccines for everyone. Assessment of health care quality is often based on country-level data on morbidity and fatality rates, and access to medicines and vaccines (5, 6), in addition to large household surveys such as the Demographic Health Survey program (7). According to current statistics, communicable diseases are the first cause of death in SSA (8); in the region, people are least satisfied with the health care services they have access to compared with other parts of the world (9, 10). According to the medium variant scenario of the United Nation’s Population Division, the population of SSA is expected to grow fast by an annual average rate of 2.7% to reach 2.2 billion by year 2050 (1), nearly doubling its current size within a few decades. At the same time, the region has one of the highest infant mortality rates in the world (8), which exerts even more pressure on its inadequate health care infrastructure.
Considering various financial and social barriers, proximity to health care per se does not necessarily translate into receiving quality treatment. For instance, a recent survey-based analysis (11) found that within-country wealth distribution inequality remains one of the strongest barriers to health care coverage in SSA countries. Nonetheless, health care accessibility is a necessary condition for enabling access to health care services (12). Unsurprisingly, a review of the literature on health care services location found that the relationship between proximity to health care facilities and health outcome is significant (13). As a specific example, empirical evidence from Nigeria has showed that living far away from health care facilities not only results in lower health insurance enrolment (14) but also, reduces the utilization of these facilities (15). Other than accessibility, availability of hospital beds coherent with local potential hospitalization requirements is crucial to ensure treatment can be provided.
Here, we elaborate a strategy to efficiently abate the measured inequalities based on a GIS-based optimization routine, which identifies the optimal location of future health care facilities of different tiers based on the projected distribution of the population of each country by 2030 in order to satisfy the conditions of SDG 3 targets. Previous work has shown that geospatial analysis is an effective methodology to assess accessibility to health care facilities (16–19), including through the lens of the required travel time to reach dispensaries, clinics, and hospitals (20, 21). To date, the most comprehensive study on SSA has compiled a geocoded inventory of public hospitals in 2015 to analyze the current situation of accessibility to hospital-based emergency care in the region (21). Yet, key limitations of this pioneering study have been identified in a response paper (22), including the fact that it only considers the physical presence of hospitals and not the actual availability of emergency care services. Features such as the availability of intensive care unit beds and surgery capabilities distinguish health care facilities of different tiers. In addition, only few transportation options and barriers have been assessed in this study.
We build upon this work by expanding it and overcoming some of its limitations. We first evaluate the current state of health care accessibility in SSA and show that hospitals that can provide life-saving services such as surgery and specialized treatment are still out of reach (farther than 120 min) (refs. 22 and 23 have threshold justification) for at least (24, 25) 170 million people (>15% of the regional population). Next, we develop a GIS optimization algorithm to estimate the number, location, and typology of the required new health care facilities to ensure universal access within reasonable travel times and sufficient beds to accommodate hospitalizations. The assessment explicitly considers the projected growth in population and urbanization in the next decade and can readily be adapted to longer-run analysis or different targets and facilities classification assumptions (replication data and code are made publicly available) (26). The results of the analysis presented in this paper can also be browsed in an interactive interface at http://ssahealthcare.decatab.com. Detailed description of the proposed algorithm and data used for our analysis are provided in Materials and Methods.
Results
Current Status of Public Health Care Accessibility in SSA.
The World Health Organization (WHO) recently released the most comprehensive georeferenced database of public health care facilities, which goes beyond only hospitals and includes other types of health care facilities as well (25). For our analysis, we categorize health care facilities into four distinct tiers, namely dispensaries and local health posts (Tier 1), health centers (Tier 2), province- and regional-level hospitals (Tier 3), and national and central hospitals (Tier 4). This is consistent with standard health care facilities classification in developing countries (see, e.g., ref. 27 and Materials and Methods). We combine this information on the type and location of health care facilities with spatially explicit data on population distribution and settlement type at a 30-arc s resolution. Population input data are obtained from the dasymetric statistical downscaling of official census data based on remotely sensed data (28) and projected to year 2030 (Materials and Methods) accounting for projected country-heterogeneous population growth and urbanization trends. We use the most recent and the most precise available gridded friction surface data for land-based travel speed (29) and an array of GIS algorithms implemented in a cloud computing framework to evaluate the current and future accessibility to health care facilities in SSA.
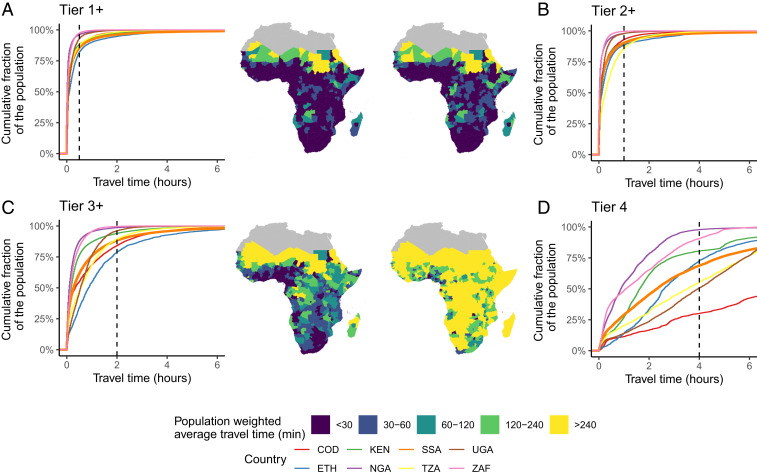
The maps in Fig. 1 show accessibility to the nearest public health care facilities in SSA (i.e., the population-weighted average travel time to the nearest facility in each region). Comparing travel time across different tiers provides several insights into the geographical heterogeneity of public health care accessibility in SSA. First, it shows that the average travel time is increasing with tiers, as a result of the uneven distribution of existing facilities across tiers. Of the existing health care facilities, 33,150 or 34% are in Tier 1; 57,522 or 60% are in Tier 2; 5,491 or 6% are in Tier 3; and only 232 (<1%) are in Tier 4. Second, the bulk of the areas where accessibility to public health care requires long journeys—at least for Tiers 1 and 2—is concentrated in geographically confined areas in the Sahel (one of the global regions with the fastest-growing population and at the same time, with the most vulnerable population), central Africa (where large areas are covered by forests with limited accessibility, such as in the Democratic Republic of the Congo and the Central African Republic), the Horn of Africa, and Madagascar. Third, more than 170 million people in SSA are more than 2 h from the nearest hospital (Tiers 3+), and about 40% of the regional population is more than 4 h away from a Tier 4 hospital facility. This highlights the urgent need to develop new facilities in locations where they can serve most people.
Fig. 1.
Accessibility to the nearest public health care facility (in travel hours), by facility tier (Tier 1 or higher, Tier 2 or higher, Tier 3 or higher, Tier 4). A–D display for Tiers 1+ to 4, respectively, 1) the classification of public health care facilities into the four tiers; 2) population-weighted travel time required to reach—from each 250-m-resolution point—the nearest public health care facility of Tier K or higher accounting for the local travel possibilities [including roads, railways, and physical barriers (30); note that Tier 1 facilities data are unavailable for Niger, Guinea-Bissau, and eastern Angola]; and 3) empirical cumulative distribution curves of the population’s accessibility to the nearest public health care facility in selected countries and the entire sub-Saharan African region (in orange). The x axis describes the travel time to public health care in minutes for Tier K or higher. The y axis describes the cumulative fraction of the population that is living within the travel time of the corresponding x value. The curves thus describe three dimensions of inequality: inequality between the countries in each tier, inequality within each country in each tier, and inequality in accessing health care facilities between the four tiers. Black dashed lines describe the accessibility time thresholds considered in this study. International Organization for Standardization codes: COD, Democratic Republic of the Congo; ETH, Ethiopia; KEN, Kenya; NGA, Nigeria; TZA, Tanzania; UGA, Uganda; ZAF, South Africa.
The empirical cumulative distribution curves in Fig. 1 highlight the inequality in accessing health care facilities both across and within countries for a selected number of countries and for SSA as a whole. The four graphs show the distribution of health care facilities as the cumulative share of the population that has access to a health care facility in each tier within a given travel time. Moving from Tier 1 to Tier 4, the distance to health care facilities become longer as the slope of the curves decreases. This means that >15% of the continent’s population lives 2 or more hours away from a hospital (Tier 3+ facility), while one of eight people is more than an hour away from the nearest health center. Most of the deficit in accessibility to hospital facilities is concentrated in Ethiopia (∼30% of the population or 30 million living more than 2 h away from the nearest hospital), the Democratic Republic of the Congo (∼38% of the population or 29 million), Nigeria (∼10% of the population or 17.7 million), and Sudan (∼31% of the population or 12 million). SI Appendix, Fig. S1 reports the detailed deficit statistics for every country.
Planning Universal Accessibility to Public Health Care.
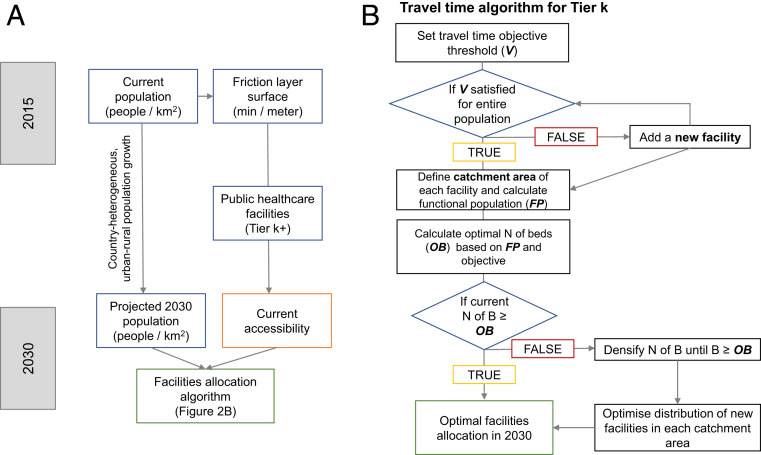
In order to meet SDG 3 by 2030, it is crucial to support planning of the new health care facilities by the means of geospatial assessments tailored to the accessibility and hospitalization needs of local communities. We introduce a multiobjective GIS routine to identify the optimal spatial allocation of the minimum number of new health care facilities that will allow the entire population of SSA to access health care within a range of maximum 30, 60, and 120 min from the nearest public health care facility in Tiers 1+, 2+, and 3+, respectively. A summary of the optimization tree is provided in Fig. 2 (Materials and Methods has further in-depth explanation).
Fig. 2.
Schematic framework of the data inputs and the process of the multiobjective optimal allocation GIS algorithm. (A) Main input data sources and their processing. (B) Tree of the optimization algorithm aiming at identifying the optimal allocation of public health care facilities in 2030. B also describes the main geospatial data inputs required by the algorithm. For each facility in Tier K (or higher), a corresponding travel time threshold objective (V minutes) is set. Then, new facilities are added in Tier K until the condition that the entire (or a user-defined share of) population is served within V minutes. Subsequently, the CA of each facility—the area around each facility where V is satisfied—is identified. The population living within each CA (i.e., FP) is calculated, and where CAs of different facilities intersect, an equal subdivision of the shared population is carried out to avoid double counting. Thereafter, the optimal number of beds (OB) in each CA is calculated based on the local FP and the global hospital beds objective per 1,000 people. Finally, in those CAs where the local facilities are not meeting the beds constraint, a densification process is carried out, where further facilities are added locally. Here, diamond-shaped boxes designate conditional statements and rectangles identify processing steps.
The secondary objective of the optimization algorithm is to ensure the availability of sufficient hospital beds (Tiers 3+) in each catchment area (CA). While the WHO does not explicitly recommend a global standard for the density of hospital beds in relation to total population (30), in our baseline scenario we opt for a conservative target of two public beds per 1,000 inhabitants. Given the fact that sub-Saharan African countries are low income with budget constraints, setting such a low target is justified when compared with more advanced economies like the United States, Canada, and the United Kingdom with 2.8, 2.5, and 2.5 beds per 1,000 population, respectively (31).
Furthermore, our assessment only deals with public health care facilities and does not consider the variety of private health care facilities in SSA countries (SI Appendix has a brief discussion of the implications). It must also be noted that the beds availability objective is a minimum requirement constraint in the optimization model. Therefore, the results might suggest outcomes with higher numbers of beds per 1,000 inhabitants since in most cases, the maximum allowed travel time for each tier will be the dominant binding constraint of the optimization process.
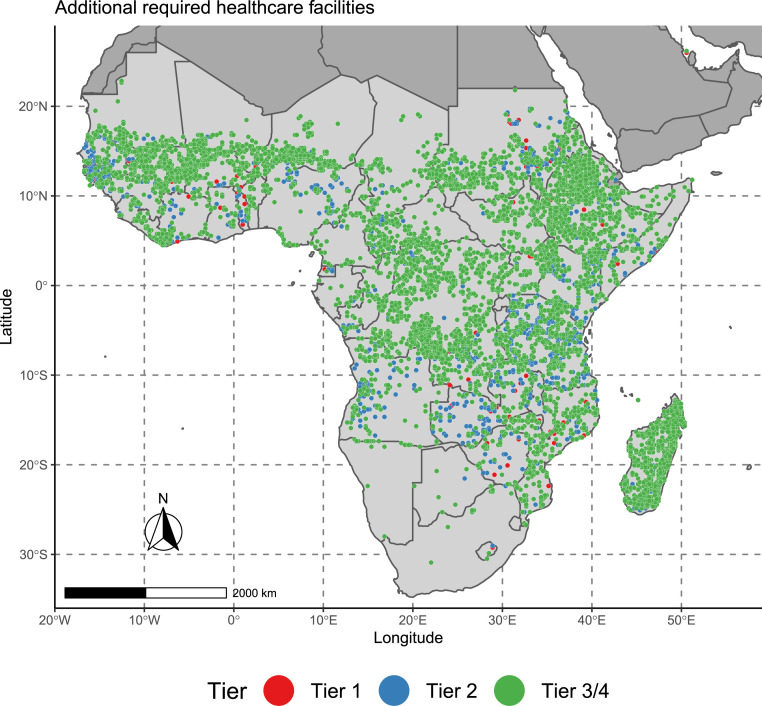
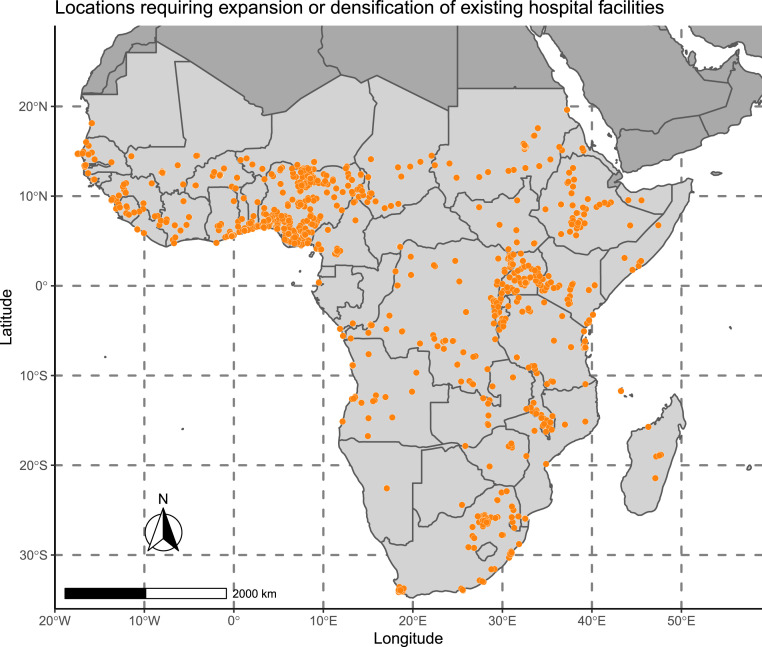
The results maps of the optimization algorithm for the baseline case are reported in Figs. 3 and 4. These depict the identified optimal position of the public health care facilities requiring construction and the locations requiring an expansion or densification of existing hospital facilities. An interactive dashboard of the results is also available online,* together with an animated version of the map of required health care facilities (Movie S1).
Fig. 3.
Map of health care facility construction requirements by 2030 in SSA. The map shows the optimal location of health care facilities (within a 25-km radius of uncertainty) that would ensure accessibility of the entire population of each country in SSA to public health care within a predefined travel time by 2030 while meeting bed density requirements to cope with hospitalization needs. Colors identify the health care tiers.
Fig. 4.
Map of locations where existing health care facility expansion or densification is required to meet the beds availability constraint by 2030 in SSA. The map shows settlements where the existing hospital facilities (Tiers 3 and 4) require an expansion or a densification to meet bed availability requirements.
Fig. 5 summarizes these requirements at the country level. We find that to ensure universal access within reasonable travel times by 2030—considering the projected 45% increase in the regional population in just one decade and the growing urbanization—6,186 new facilities must be built. These new facilities are the minimum requirement to meet accessibility targets in terms of travel time. To satisfy bed availability constraints, 1,078 existing hospitals (Tier 3+ facilities) must be expanded.† To put these numbers in perspective, currently there are 5,723 hospitals in SSA. The bulk of the required new facilities for meeting accessibility purposes is concentrated in the Democratic Republic of the Congo (14.7%, 909 hospitals), Ethiopia (12%, 740 hospitals), Madagascar (7.8%, 480 hospitals), Tanzania (7.6%, 470 hospitals), Mali (7.3%, 453 hospitals), and Sudan (6.9%, 424 hospitals). The majority of the expansion of existing facilities to increase the hospital beds availability must take place in Nigeria (23.7%, 256 hospitals needing expansion), the Democratic Republic of the Congo (9.3%, 100 hospitals), South Africa (7.5%, 81 hospitals), Uganda (5.5%, 59 hospitals), Sudan (4.7%, 51 hospitals), Tanzania (4.4%, 47 hospitals), and Ethiopia (4.1%, 44 hospitals).
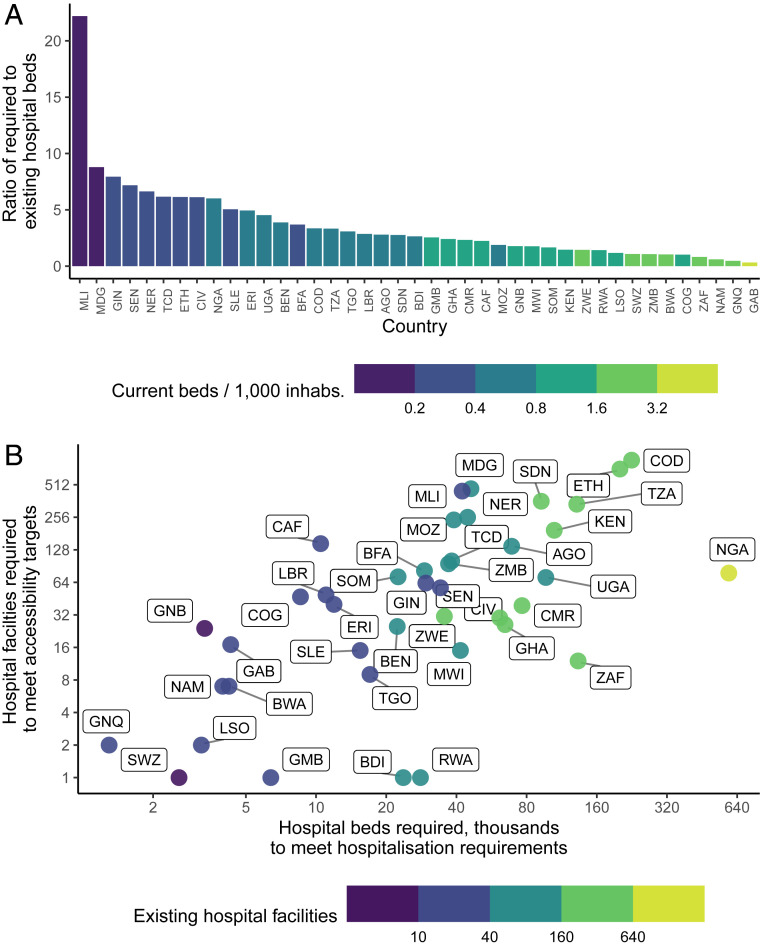
Fig. 5.
Country-level hospitals and beds requirements by 2030 in SSA. (A) Bar plot showing the ratio of new required public hospital beds to achieve an availability of two beds per 1,000 local population by 2030 compared with the currently reported beds in each country (according to the most recent statistics from the WHO supplemented by country data and provided by the World Bank). (B) Logarithmic scatterplot of the required additional hospital beds and hospital facilities (to meet accessibility targets, excluding expansion of existing facilities) to be added by 2030, with the color fill showing the absolute number of existing hospital facilities. AGO, Angola; BDI, Burundi; BEN, Benin; BFA, Burkina Faso; BWA, Botswana; CAF, Central African Republic; CIV, Côte d’Ivoire; CMR, Cameroon; COD, Democratic Republic of the Congo; COG, Republic of the Congo; ERI, Eritrea; ETH, Ethiopia; GAB, Gabon; GHA, Ghana; GIN, Guinea; GMB, Gambia; GNB, Guinea-Bissau; GNQ, Equatorial Guinea; KEN, Kenya; LBR, Liberia; LSO, Lesotho; MDG, Madagascar; MLI, Mali; MOZ, Mozambique; MRT, Mauritania; MWI, Malawi; NAM, Namibia; NER, Niger; NGA, Nigeria; RWA, Rwanda; SDN, Sudan; SEN, Senegal; SLE, Sierra Leone; SOM, Somalia; SSD, South Sudan; SWZ, Swaziland; TCD, Chad; TGO, Togo; TZA, United Republic of Tanzania; UGA, Uganda; ZAF, South Africa; ZMB, Zambia; ZWE, Zimbabwe.
As shown in Fig. 4, the majority of required new additions suggested by our optimization framework are high-tier facilities. This reflects the fact that the bulk of the current accessibility deficit is related to hospitals and hospital beds, while as seen in Fig. 1, only about 10% of the regional census population is outside of dispensary accessibility targets. Interestingly, the results reveal that the tier by tier objectives might be complementary. Satisfying hospital (Tier 3+) availability requirements would also contribute to covering a significant portion of accessibility requirements for Tier 2 and Tier 1 facilities (health centers and dispensaries). This means that in areas where dispensaries and health centers are still inaccessible to large parts of the population, allocating resources to build high-tier facilities that can serve both the basic pharmaceutical needs and more specialized and intensive health care might be beneficial. In other words, fulfilling high-tier accessibility requirements can concurrently achieve low-tier accessibility objectives. This finding does not discourage the construction of a dense network of dispensaries, which is vital: it merely suggests that in SSA, accessibility is mainly a problem affecting higher-tier facilities (Discussion).
With regard to the secondary objective of guaranteeing a sufficient local availability of beds, we estimate that if a universal objective of 2 local public hospital beds per 1,000 population is imposed, 2.5 million new hospital beds are required (with a compound annual growth rate of 11.2% from 2020 to 2030). These beds are distributed unequally among new facilities where currently the local populations are facing accessibility constraints (15.3% of the total) and among existing facilities requiring densification or expansion (the residual 84.7%), namely in areas where hospitals are available but are insufficient to meet hospitalization requirements. This disproportioned distribution is the result of the strongly growing urban populations. Overall, required beds are distributed mostly in Nigeria (23.4% of the total), the Democratic Republic of the Congo (9%), Ethiopia (8%), South Africa (5.3%), and Tanzania (5.2%).
Relative to currently available beds, the strongest need for new beds is found in Mali (with a ratio of required to existing hospital beds of ∼22:1), Madagascar (∼9:1), Guinea (∼8:1), Senegal and Nigeria (∼7:1). On the other hand, the deficit relative to the population (defined as the difference between additional required and existing hospital beds per 1,000 inhabitants) is highest in Nigeria (1.9 beds), Cote d’Ivoire (1.8 beds), Eritrea (1.6 beds), Mali (1.6 beds), Gambia (1.5 beds), Guinea (1.5 beds), Senegal (1.5 beds), and Chad (1.5 beds). The plots in Fig. 5 summarize these results.
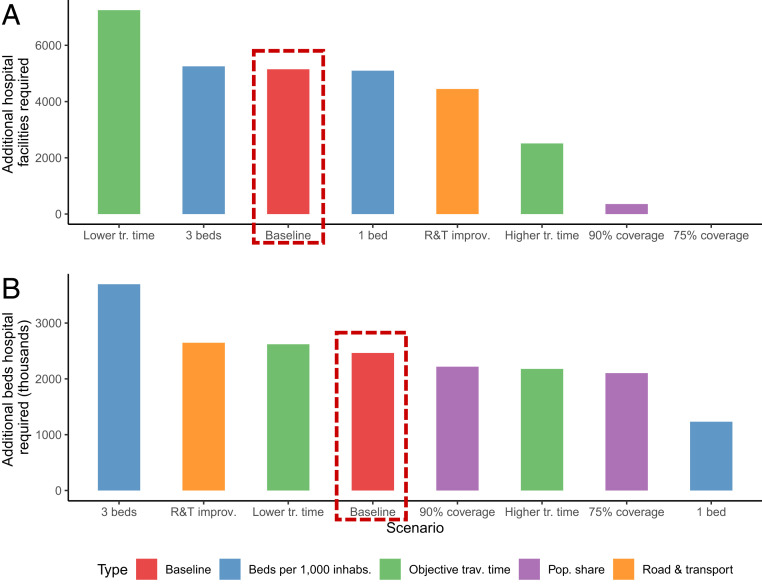
The sensitivity analysis (summarized in Fig. 6 and SI Appendix) shows the impact of changing key objectives and parameters in the optimization process on the number of additional required hospitals (including expansion/densification of existing facilities) and hospital beds.
Fig. 6.
Sensitivity analysis results. (A) Bar plot for the number of required health care facilities, by facility tier and scenario. (B) Bar plot of the distribution of required hospital beds, in thousands, by scenario. R&T, road and transportation; tr., travel; trav., travel; inhabs., inhabitants; pop., population.
In general, imposing less stringent accessibility objectives for the share of people who live within the baseline travel times from health care facilities implies a large reduction in the number of required hospital facilities. For example, increasing (decreasing) the travel time thresholds‡ will result in −105.2% (+40.8%) change in the number of required hospital facilities and −11.6% (+6.3%) change in the number of required beds. Serving 90 or 75% of the population instead of the whole population leads to drastic reductions in the number of additional hospitals required but conversely, only to a 10 to 15% decrease in the number of required beds. This is because hospital accessibility issues are most harshly affecting about 15% of the regional population (∼170 million people). On the other hand, changing the minimum bed requirement from the baseline of two to one and three beds per 1,000 people leads to −1 and +2% changes in the total number of health care facilities, respectively, and −50 and +50% changes in the total number of required hospital beds, respectively. Finally, if the road infrastructure is improved and the general people transportation friction is reduced by 25% of the current value through a linear reduction on the friction surface raster layer (as detailed in Materials and Methods), achieving the objectives set in the baseline scenario requires 13.6% fewer hospital facilities, suggesting a complementarity between the improvement in different types of infrastructure.
Discussion
Our study sheds light on pervasive inequalities in accessibility to public health care in SSA, a region with the highest premature mortality rate and steep population and urbanization growth rates. The potential socioeconomic benefit of improving health outcomes in the region—where communicable diseases are most widespread in rural areas (31)—cannot be overstated. We showed that inequality in accessibility to public health care is not only prominent within and between countries in this region but also, related to the quality of service provided (i.e., accessibility to different health care tiers). Overall, our results and the methodology we developed here can inform local policy makers in their assessment of current accessibility trends and prioritization of future health care infrastructure.
Through our analysis, we were also able to identify potential locations for new health care facilities to be added by 2030 in order to achieve the universal health care accessibility within reasonable travel times considering the population growth and the rising share of urban population. We find that adding high-tier facilities that are suitable for providing both basic services, such as vaccination, and specialized services, such as surgery, at the same time is more efficient to ensure universal and equal health care accessibility in remote areas and minimize the total number of new facilities while achieving SDG 3 objectives. This indeed requires ramping up investment in large-scale health care infrastructure and other ancillary services such as education and training of medical staff, provision of medical tools and equipment, and developing reliable communication and transportation infrastructure. It is worth mentioning that physical accessibility to health care facilities as outlined in this paper should be considered only one part of a larger coordinated effort to reduce mortality, eradicate epidemics, and achieve universal health care coverage in SSA. Other important public health programs such as Global Health Initiatives are playing an equally important role in reducing mortality and improving life expectancy by controlling and eradicating communicable diseases as well as improving the current health infrastructure. This requires a high-level coordination and collaboration between national health authorities, international organizations such as the WHO, nongovernmental organizations, and international donors (32).
Although the overarching conclusion of our analysis—highlighting the disparity in health care accessibility in SSA and the need for early investment in higher-tier facilities to tackle inequality—remains valid across different scenarios of the future growth of population and urbanization, specific quantitative results should be interpreted with caution. For example, accessibility to health care as defined by travel time does not consider accessibility (including affordability, as health care deficit areas are likely to overlap with high poverty density) to different transportation modes (either public or private) or growing congestion in highly dense areas. As a result, the reported travel times may not realistically represent the effective home to facility time in year 2030. Another important aspect is the management of health care facilities that plays a key role in determining waiting time and subsequently, home to treatment time. We should also emphasize the difference between accessibility and access, as the former is a necessary but not sufficient condition for the latter. In this paper, we have only evaluated accessibility in terms of travel times and have not covered other important factors affecting access to health care. Nevertheless, achieving more equal and accessible health care strongly resonates with the mitigation of transport accessibility inequality (32, 33). Poor road infrastructure in rural areas, insufficient public transport options in periurban areas, and congestions in urban centers all contribute to the current state of unequal accessibility to health care facilities.
Concerning the data-related limitations of our analysis, some remarks are necessary. In the analysis, we adopt the 250-m resolution Global Human Settlement (GHS) population data product (29), which downscales census information to grid-cell population data. Yet, as discussed in Carr-Hill (24, 25), in African countries census data are often a lower bound of the actual population, as census surveys tend to systematically exclude specific population groups. These include nomads and agropastoralists who—to the aims of our analysis—are likely to live remotely from health care-provisioning facilities and refugees who irrespective of their prevalent urban or periurban location are likely to face accessibility constraints owing both to transport and accessibility issues and to legal and economic barriers; similar arguments hold for periurban slum dwellers and homeless who are likely to live in physical proximity to health care and yet, might face significant accessibility constraints. To provide an order of magnitude to this uncertainty, Carr-Hill (24) estimates that the poor missing from census data represent about 11% of the population of SSA (i.e., more than 100 million people). Yet, adjusting the gridded, continent-wide results of our health care accessibility analysis to this gap is challenging. The distribution of these “missing” populations simply cannot be assumed to be homogeneous. As a bottom line, our health care inaccessibility estimates and our required facilities and beds projections are best interpreted as lower-bound values. A crucial little explored research area is the development of a methodology to account for those missing populations in gridded population data products (34), ideally by means of calculation of site-specific adjustment factors.
Finally, a potential extension to the current analysis may include province-specific objectives as a function of local morbidity rates and of additional specific hospitalization requirements. In addition, alternative optimization approaches to minimize costs (i.e., investment costs, operation and maintenance costs, etc.) in the optimization framework can be considered in the future. This would allow policy makers to allocate limited financial resources more efficiently in the public health sector. However, such analysis would require collecting country-specific data on historical and forecasted socioeconomic variables over technology, materials, labor, and energy costs, which is beyond the scope of the current analysis.
Materials and Methods
Input Data and Processing.
Table 1 summarizes the input data employed in the analysis and the corresponding sources. The GHS population layer (28) is a 250-m-resolution raster dataset reporting the estimated number of people living in each pixel in year 2015. It is estimated with a binary dasymetric approach (i.e., using Landsat-derived built-up areas [which are provided through the GHS-SMOD 2015 dataset] and allocating population data from subnational census data proportional to the settlement extents). The public health care facilities database (25) is a comprehensive spatial inventory of 98,745 public health facilities in SSA assembled with national master health facility lists from a variety of government and nongovernment sources and using multiple geocoding methods to assign coordinates to each facility. The Global Friction Surface (29) enumerates land-based travel speed for all land pixels in minutes per meter. It is based on a broad collection of datasets including roads (Open Street Map and Google roads datasets jointly), railways, rivers, lakes, oceans, topographic conditions, land cover types, and national borders (crossing borders imposes a travel time penalty). The global administrative boundaries (GADMs) (35) provide up-to-date boundary shape files of countries and administrative units.
Table 1.
Data input sources
| Description | Unit | Spatial resolution | Ref. |
| GHS-POP 2015 population | Count | 250 m | 28 |
| Public health care facilities database | Typology | Exact position | 25 |
| GHS-SMOD 2015 settlements classification | Class | 1 km | 28 |
| Global friction surface | Minutes/meter | 1 km | 29 |
| GADM | — | Country level | 35 |
| Population and hospital beds availability statistics | Count | Country level | 31 |
| Population and urbanization projections to 2030 | Count and share | Country level | 1, 36 |
The data are processed in a scientific computing and GIS data processing environment including R 3.6.1 (refer to the public repository linked at the end of this paper for the complete list of dependencies) and Google Earth Engine. The high granularity of the data and computational intensiveness of the geospatial queries carried out require high-performance computing capabilities, which in our case, were accessed through a virtual machine in the Google Cloud Platform (SI Appendix has a detailed account of the specifications selected to successfully run the analysis).
Health Care Facilities Classification.
Health care facilities are classified into four tiers according to the following general criteria: Tier 1: dispensary or basic health post; Tier 2: health center; Tier 3: provincial hospital or regional hospital; and Tier 4: central hospital or national hospital.
Given the heterogeneity in the naming standard across countries of SSA, a manual labeling to classify existing public health care facilities is necessary. This is achieved by extracting unique facility-type names (which are recurrent within countries but diverse across countries), assigning a tier value between one and four depending on the national classification standards for public health care facilities while sticking as closely as possible to the general convention, and finally, by parsing the corresponding tier to each facility in the database. A caveat that needs to be considered is that Tier 1 facilities data (i.e., dispensaries) are unavailable for Niger, Guinea-Bissau, and eastern Angola due to irretrievability, as discussed in Maina et al. (27). Moreover, a very limited share of facilities (2.4% of the total database) lacks precise georeferencing and only has a reference to the facility name and the first level of disaggregation of administrative boundary of belonging. Where possible, the exact location of these facilities is determined using the geocode_OSM function of the R package tmaptools. Where no geocoding can be achieved, the location is approximated to the centroid of the administrative area of belonging. The latter parsing is achieved through a fuzzy merge of the names reported by the GADM level 1 database (37) and the administrative boundary names for the unreferenced health care facilities accomplished with the fuzzyjoin R package.
Accessibility Estimation and Inequality Assessment.
Accessibility is estimated following procedures, code, and data described in Weiss et al. (30). The key external data input is a 1-km-resolution friction surface layer. The friction layer expresses—for each cell—a nominal overall speed of travel (in minutes per meter) based on the types occurring within that pixel, with the fastest travel mode intersecting the pixel being used to determine the speed of travel in that pixel.
The friction layer is converted into a transition matrix, namely a layer obtained through the application of a user-defined function [the default one, referring to Weiss et al. (30), is , with being the set of nine friction values in the cell itself and in the eight adjacent cells] on the friction surface layer given a set number of directions in which cells are connected. This serves to calculate the travel time to move from one cell to the adjacent ones given the infrastructure and barriers found in each cell. Sensitivity analysis on the functional form is carried out (see the corresponding section below). The transition layer is then exploited in combination with the georeferenced location of public health care facilities and the cumulativeCost function in Google Earth Engine (or alternatively, the accCost function from gdistance package in R) to produce a raster layer of the travel time (in minutes) to the nearest facility of each tier (or superior).
To assess accessibility inequality, we estimate the share of the population of each country that is living in cells with a given travel time to the nearest public health care facility of each tier. To visualize the results, we produce an empirical cumulative distribution function of the population-weighted travel time variable.
Spatial Allocation of Population Growth to 2030.
In the location optimization analysis, the time horizon is set at year 2030, that of the SDGs. Thus, to account for the steeply growing population in the region, we refer to the United Nations’ Population Division estimates (1) (medium variant), according to which 1.4 billion people will live in SSA in 2030. At the same time, we refer to recent estimates in, according to which in 2030, the urban population will account for 47% of the regional population World Urbanization Prospects 2018 (38).
To allocate the population growth and population density change by 2030 across 1-km-resolution grid cells, we first classify them as either urban or rural using the GHS-SMOD 2015 settlements classification. Urban areas are defined (29) as cells with GHS-SMOD = 30, rural areas as cells with 11 ≤ GHS-SMOD ≤ 23, and inhabited areas as cells with GHS-POP = 0.
To validate the urban/rural classification criteria and its projection to 2030, we sum the total GHS-POP population for year 2015 in cells classified as urban and divide it by the sum of total regional population. This yields an urbanization rate of 0.42, which is in line with the fraction of urban population in SSA of 0.4 reported by the World Bank (33) and with the value of 0.39 reported by the United Nations Department of Economic and Social Affairs (38).
Then, we refer to urban and rural country-specific population growth rates from the World Urbanization Prospects 2018 (38) to project each cell’s population (conditional on it being urban or rural and on the country of belonging) to 2030. Since the World Urbanization Prospects 2018 (38) data have a 5-y time step, we operate the following projection:
| [1] |
where and are the populations in years 2030 and 2015 at each grid cell i, respectively; is the urban/rural classification; and UPGRc and RPGRc are the yearly average urban and rural population growth rates in 2020 to 2025 and 2025 to 2030 periods in each country c, respectively.
The formula ensures that each country’s total population converges to the projected value for 2030 (1.4 billion), and at the same time, the forecasted urbanization rate (0.476 our estimate; 0.47 United Nations’ projection) is approximated. The main limitation of the approach is that it assumes 1) that areas that have a population of zero in 2015 will also have a population of zero in 2030 and 2) that the classification of urban and rural grid cells remains constant until 2030 (i.e., cells identified as urban or rural in 2015 are also urban or rural in 2030).
Optimization of the Location of Potential Facilities to 2030.
To optimize the location of potential facilities for each health care facility tier (in the optimization, we make no explicit distinction between Tier 3 and 4 facilities; i.e., hospitals§), we develop a multiobjective GIS-based algorithm in the R scientific programming language. First, the algorithm estimates the fraction of population that lies within n minutes (for the base case, set at 30, 60, and 120 min for Tiers 1 to 3/4, respectively) of travel time from the nearest existing health care facility of Tier k or higher. Then, for each tier, it generates a population-weighted kernel density map with a bandwidth of 0.25° (about 28 km at the equator), it selects the single cell that is more than n minutes of travel time from the nearest existing health care facility and has the highest population kernel density value, and it allocates a new facility there. Subsequently, it recalculates the fraction of population that lies within n minutes of travel time from the nearest existing health care facility. The procedure is then reiterated for the kth cell with the highest population kernel density value by adding k new facilities, until the user-imposed condition of a given fraction of the population lying within n minutes of travel time from the nearest existing health care facility is met. We assume that all existing facilities will continue functioning for the next 10 y, and therefore, we do not consider decommissioning the existing facilities.
In the baseline case presented in Results, we assign values of 0.99 for the fraction of 2030 population benefitting from access of each tier (i.e., quasiuniversal access, with a 1% tolerance to cope with very dispersed population pixels that could significantly affect the result and yet, represent input population data errors), and we impose travel time restrictions of 30, 60, and 120 min for Tiers 1+, 2+, and 3/4, respectively. The code allows for easy parameter alteration, replication, or adaptation to other similar optimal facility allocation based on travel time and population-defined accessibility.
CAs and Functional Populations Definition.
In order to estimate the number of new facilities that are needed at each of the sites identified as optimal in order to guarantee a sufficient availability of beds per capita, the following intermediate steps are carried out. Here, only facilities of Tiers 3 and 4, namely those allowing for hospitalization, are considered.
First, the CA of each facility—defined as the area surrounding each facility of Tier K at which the travel time constraint V is satisfied for that facility—is identified. Then, the functional population (FP; the population that is the potential beneficiary of health care at each facility i, calculated as the sum of the population in pixels that is n minutes away from the [potential] location of the facility, namely the CA itself, where in the base case, n corresponds to 120 min) is estimated. This calculation implies that those populations that are living at a longer travel time than the threshold will not be considered as served by facility i. Yet, as a result of the first step of the optimization process, every person will be served by at least one facility of Tier k within n minutes. This is achieved by recursively running the travel time estimation algorithm individually for each facility.
The pixels falling in the CAs are converted to a vectoral shape using the R package sf. Zonal statistics of the population living within each CA (named FP) are calculated. In order to avoid double counting (i.e., allocating the same population to multiple CAs in those cases where those areas intersect or overlap for two or more facilities), the population allocation is split into two substeps:
| [2] |
First, the population living in the portion of the CA i that is exclusive of the facility (i.e., it does not intersect with any of the other CAs −i) is calculated. Then, this is summed to the population living in the other portion of the CA that is shared with CAs of other facilities, divided by the number of facilities sharing that portion of CAs N. In this way, where CAs belonging to different facilities intersect, the local population is equally allocated across facilities.
Beds Availability Constraint.
When the identified potential facilities become sufficient to satisfy the travel time targets, the second functional objective is evaluated. First, a fixed objective of beds per 1,000 inhabitants (in the baseline case set to two) is defined. Then, the algorithm assesses if—at each health care facility location, including both currently existing and potential new facilities—there is a sufficient availability of beds to satisfy the constraint based on the local FP (the population living within each facility’s CA). Current beds are allocated to existing facilities by downscaling national statistics on the total number of beds (reported at the country level by the WHO’s Global Health Observatory database) based on the tier of each facility. This is achieved in two steps. First, we evaluate the average ratio of beds between facilities of Tier 4 and Tier 3 based on the Kenya health care facilities database (the only recent comprehensive country-level dataset providing a list of health care facilities including the local availability of beds and the type; i.e., the tier). This is empirically estimated at 17.8 (i.e., facilities of Tier 4 on average have 17.8× more beds than facilities of Tier 3). Then, generalizing this ratio for SSA, we solve n linear systems of equations of the form
| [3] |
for each country in SSA. The system calculates the number of beds in the average facilities of Tiers 3 and 4 (indicated by ) while ensuring that the result is consistent both with the national officially reported total number of beds and the empirically identified ratio between the number of beds per facility in each tier. Newly added facilities in the optimization to 2030 are assumed to have a number of beds that are equal to the weighted average between the average bed numbers for Tiers 3 and 4 of currently existing facilities and the share of Tier 3 and 4 facilities over the sum of all hospital facilities.
Then, exploiting the FP of each facility calculated in the earlier steps, if the local beds constraint is not satisfied, additional k facilities of the same tier of that examined are added in the surroundings, namely in the k most-populated pixels within the FP area. The densification process reiterated until the constraint is satisfied. This allows us to ensure that newly added facilities are enough to cope with potential hospitalization needs in the area. In actual terms, this process might translate either in the expansion of single larger hospitals or in a densification through the construction of a set of hospitals in the same CA.
Sensitivity Analysis.
To assess the sensitivity of the optimal allocation algorithm results to changes in the target share of the population and the travel time to each facility tier, we produce additional runs at 75 and 90% for the population gaining accessibility and at 30 and 60 min for Tier 1+, 45 and 90 min for Tier 2+, and 90 and 180 min for Tiers 3/4, respectively. We also test the effect on changing the hospital beds per 1,000 people constraint to sensitivity values of one and three. Finally, to evaluate the role of an improving transportation network—in terms of both road availability and quality and of public transportation means—we operate a linear reduction to the friction surface layer by changing the standard transition matrix generation function to the following function:
| [4a] |
where
| [4b] |
This reduction serves to estimate the impact of reducing travel times by 25% (with an improvement proportional to current travel times) on the requirement of new health care facilities. The complete results of the sensitivity analysis are reported in SI Appendix.
Supplementary Material
Acknowledgments
Although this research did not receive any specific funding, G.F. acknowledges financial support from the Italian Ministry of University and Research.
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission.
*The interactive platform is at https://athammad.shinyapps.io/OptimalGIS/.
†Here, by expansion, we mean either an enlargement of a currently existing facility to enable coping with more hospitalizations or the construction of new structures in the proximity of the existing. In either case, the expansion is necessary to increase the bed availability but does not relate to travel times and accessibility targets.
‡From the baseline thresholds of 120, 60, and 30 min for Tiers 3/4, 2, and 1, respectively, to 90, 45, and 30 min and to 180, 90, and 60 min.
§The decision to consider Tier 3 facilities (provincial and regional hospitals) and Tier 4 facilities (central and national hospitals) lies in the need for a regionally homogeneous result, whereby different countries face different standards for hospitals that we classify as Tiers 3 and 4. Concretely, this means that a Tier 3 hospital in one country might be similar to a Tier 4 hospital in another country.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2009172117/-/DCSupplemental.
Data Availability.
Computer code and input data to replicate or update the analysis and the figures and the result data of baseline and sensitivity analysis model runs are publicly hosted at Zenodo (http://doi.org/10.5281/zenodo.3757084). Powerful (or cloud; e.g., Google Earth Engine, RStudio Cloud, or Google Colab) computing facilities are recommended for a successful replication.
References
- 1.United Nations Population Division , World population prospects: The 2017 revision (2017). https://population.un.org/wpp/. Accessed 10 January 2020.
- 2.Aylward B. et al.; WHO Ebola Response Team , Ebola virus disease in West Africa—the first 9 months of the epidemic and forward projections. N. Engl. J. Med. 371, 1481–1495 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gilbert M., et al. , Preparedness and vulnerability of African countries against importations of COVID-19: A modelling study. Lancet 395, 871–877 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United Nations , Resolution adopted by the General Assembly on 25 September 2015: Transforming our world: The 2030 Agenda for Sustainable Development (2015). https://sustainabledevelopment.un.org/post2015/transformingourworld. Accessed 10 January 2020.
- 5.World Health Organisation , WHO mortality database (2019). https://www.who.int/healthinfo/mortality_data/en/. Accessed 10 January 2020.
- 6.Meara J. G., et al. , Global surgery 2030: Evidence and solutions for achieving health, welfare, and economic development. Lancet 386, 569–624 (2015). [DOI] [PubMed] [Google Scholar]
- 7.USAID , MEASURE DHS STATcompiler (2009). https://www.statcompiler.com/en/. Accessed 10 January 2020.
- 8.World Health Organisation , WHO global health estimates (2019). https://www.who.int/healthinfo/global_burden_disease/en/. Accessed 10 January 2020.
- 9.Deaton A. S., Tortora R., People in sub-Saharan Africa rate their health and health care among the lowest in the world. Health Aff. (Millwood) 34, 519–527 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dechambenoit G., Access to health care in sub-Saharan Africa. Surg. Neurol. Int. 7, 108 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wehrmeister F. C. et al.; on the behalf of the Countdown to 2030 for Women’s, Children’s and Adolescents’ Health regional collaboration in sub-Saharan Africa , Wealth-related inequalities in the coverage of reproductive, maternal, newborn and child health interventions in 36 countries in the African Region. Bull. World Health Organ. 98, 394–405 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Syed S. T., Gerber B. S., Sharp L. K., Traveling towards disease: Transportation barriers to health care access. J. Community Health 38, 976–993 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kelly C., Hulme C., Farragher T., Clarke G., Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open 6, e013059 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ernst & Young, Oxford Economics, Global analysis of health insurance in Sub-Saharan Africa (2018). https://www.ey.com/Publication/vwLUAssets/EY-global-analysis-of-health-insurance-in-sub-saharan-africa/$FILE/ey-global-analysis-of-health-insurance-in-sub-saharan-africa.pdf. Accessed 10 January 2020.
- 15.Awoyemi T. T., Obayelu O. A., Opaluwa H. I., Effect of distance on utilization of health care services in rural Kogi State, Nigeria. J. Hum. Ecol. 35, 1–9 (2011). [Google Scholar]
- 16.Polo G., Acosta C. M., Ferreira F., Dias R. A., Location-allocation and accessibility models for improving the spatial planning of public health services. PLoS One 10, e0119190 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jin M., Liu L., Tong D., Gong Y., Liu Y., Evaluating the spatial accessibility and distribution balance of multi-level medical service facilities. Int. J. Environ. Res. Public Health 16, 1150 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hulland E. N., et al. , Travel time to health facilities in areas of outbreak potential: Maps for guiding local preparedness and response. BMC Med. 17, 232 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weiss D. J. et al., Global maps of travel time to healthcare facilities. Nat Med, 10.1038/s41591-020-1059-1 (2020). [DOI] [PubMed] [Google Scholar]
- 20.Chen B. Y., Wang Y., Wang D., Lam W. H. K., Understanding travel time uncertainty impacts on the equity of individual accessibility. Transp. Res. Part D Transp. Environ. 75, 156–169 (2019). [Google Scholar]
- 21.Wigley A. S., et al. , Measuring the availability and geographical accessibility of maternal health services across sub-Saharan Africa. BMC Med. 18, 237 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ouma P. O., et al. , Access to emergency hospital care provided by the public sector in sub-Saharan Africa in 2015: A geocoded inventory and spatial analysis. Lancet Glob. Health 6, e342–e350 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marsh R. H., Rouhani S. A., Gaps in physical access to emergency care in sub-Saharan Africa. Lancet Glob. Health 6, e240–e241 (2018). [DOI] [PubMed] [Google Scholar]
- 24.Carr-Hill R., Measuring development progress in Africa: The denominator problem. Can. J. Dev. Stud. 35, 136–154 (2014). [Google Scholar]
- 25.Carr-Hill R. A., Measuring progress toward the millennium development goals and the missing millions. World Health Popul. 14, 4–11 (2013). [DOI] [PubMed] [Google Scholar]
- 26.Falchetta G., Hammad A. T., Shayegh S., Planning universal accessibility to public healthcare in sub-Saharan Africa (Version 1.0). Zenodo. 10.5281/zenodo.3757084. Deposited 19 April 2020. [DOI] [PMC free article] [PubMed]
- 27.Maina J., et al. , A spatial database of health facilities managed by the public health sector in sub Saharan Africa. Sci. Data 6, 134 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Action P., Poor People’s Energy Outlook 2013: Energy for Community Services (Practical Action Publishing, Rugby, United Kingdom, 2013). [Google Scholar]
- 29.Pesaresi M., et al. , European Commission, Joint Research Centre, JRC Data Catalogue, GHS built-up grid, derived from Landsat, multitemporal (1975, 1990, 2000, 2014) (2015). https://ec.europa.eu/jrc/en/publication/ghs-built-grid-derived-landsat-multitemporal-1975-1990-2000-2014-ir2017-v10. Accessed 10 January 2020.
- 30.Weiss D. J., et al. , A global map of travel time to cities to assess inequalities in accessibility in 2015. Nature 553, 333–336 (2018). [DOI] [PubMed] [Google Scholar]
- 31.World Health Organisation , Indicator compendium: World health statistics (2014). https://www.who.int/gho/publications/world_health_statistics/WHS2015_IndicatorCompendium.pdf. Accessed 10 January 2020.
- 32.Mwisongo A., Nabyonga-Orem J., Global health initiatives in Africa–Governance, priorities, harmonisation and alignment. BMC Health Serv. Res. 16 (suppl. 4), 212 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Bank, World Bank Data (2019). https://data.worldbank.org/. Accessed 10 January 2020.
- 34.Wardrop N. A., et al. , Spatially disaggregated population estimates in the absence of national population and housing census data. Proc. Natl. Acad. Sci. U.S.A. 115, 3529–3537 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Strazdins L., et al. , Time scarcity: Another health inequality? Environ. Plann. A 43, 545–559 (2011). [Google Scholar]
- 36.Pablo J., Bocarejo S., Ricardo D., Oviedo H., Transport accessibility and social inequities: A tool for identification of mobility needs and evaluation of transport investments. J. Transp. Geogr. 24, 142–154 (2012). [Google Scholar]
- 37.Hijmans R., Garcia N., Wieczorek J., GADM: Database of Global Administrative Areas, Version 3.6 (University of California, Berkely, CA, 2018). [Google Scholar]
- 38.United Nations Department for Economic and Social Affiars , World Urbanization Prospects 2018 (United Nations Department for Economic and Social Affiars, 2018). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Computer code and input data to replicate or update the analysis and the figures and the result data of baseline and sensitivity analysis model runs are publicly hosted at Zenodo (http://doi.org/10.5281/zenodo.3757084). Powerful (or cloud; e.g., Google Earth Engine, RStudio Cloud, or Google Colab) computing facilities are recommended for a successful replication.