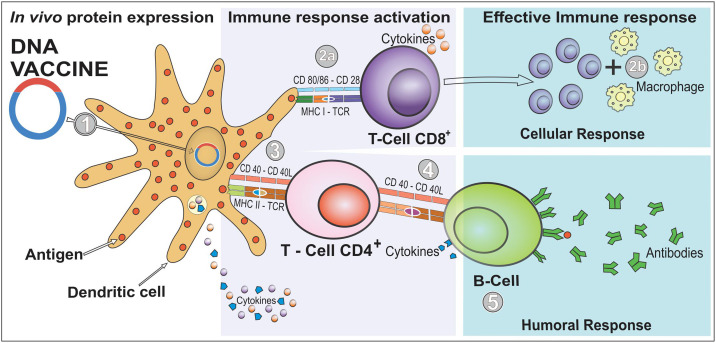
Fig. 1.
Induction of cellular and humoral immunity after immunization with DNA vaccines. A DNA vaccine consists of a plasmid produced in bacteria that encodes the protein of interest (an antigen) in the presence of a mammalian promoter. It is placed in a way that it reaches the cell nucleus, enabling the transcription and translation in the transfected human cells (step 1). After the plasmid uptake in vivo, the encoded protein is expressed in the host's cells, and the vaccine antigen can be then presented to antigen-presenting cells (APCs), such as dendritic cells (DCs), through the major histocompatibility complex (MHC) pathways and be presented to activate naïve T cells. CD8+ T cell immunity is predominantly activated by endogenously expressed antigens presented on MHC class I molecules (step 2a). The active CD8+ T cell stimulates the release of cytokines (e.g., interferon-gamma [IFN-γ] and tumor necrosis factor-alpha [TNF-α]) that inhibit viral replication and increase the expression of MHC I molecules. Therefore, macrophages are also activated to support cell-mediated immune responses (step 2b). However, CD4+ T helper cell activation is triggered through MHC class II from APC (step 3). In case the vaccine proteins are secreted, these targets are recognized by B cell receptors in naïve B cells, which also use MHC-II to get activated (step 4). In this immune pathway, activated B cells will produce different classes of antibodies (mainly IgG) to protect against the disease (step 5). Furthermore, immunization with DNA vaccine expresses proinflammatory cytokines and chemokines. DCs are responsible for producing IL-10, IL-12, and TNF-α that induce the cellular response by activating CD8+ T and IL-4 is involved in activating CD4+ T.