Abstract
This study reports a patient with DRESS syndrome, associated with liver failure, treated with orthotopic liver transplantation.
Keywords: case reports, drug hypersensitivity syndrome, liver failure, sulfasalazine
This study reports a patient with DRESS syndrome, associated with liver failure, treated with orthotopic liver transplantation.

1. INTRODUCTION
Drug reaction with eosinophilia and systemic symptoms is an unusual drug reaction–related condition. A case report of sulfasalazine‐induced liver failure is described. The patient required liver transplantation. Liver transplantation is an option when the DRESS syndrome is associated with acute liver failure, but the prognosis remains poor.
Drug reaction with eosinophilia and systemic symptoms (DRESS syndrome) is a rare drug reaction–related condition. 1 Several drugs have been linked to DRESS. It is a severe idiosyncratic drug reaction characterized by erythematous or papulopustular skin eruption associated with lymphadenopathy, fever, and visceral involvement (hepatitis, nephritis pneumonitis, pericarditis, myocarditis, and colitis). 2 , 3 , 4 , 5 , 6 Leukocytosis, eosinophilia (90%), or mononucleosis (40%) may also be identified. 6 Severe acute hepatitis due to sulfasalazine or trimethoprim‐sulfamethoxazole is described in the literature, but the occurrence of DRESS syndrome causing liver failure is rare.
In this study, we report a patient with acute liver failure due to sulfasalazine‐induced DRESS, treated with a liver transplant.
2. CASE REPORT
An 18‐year‐old male patient was treated with sulfasalazine for toxoplasma retinochoroiditis for one month. The patient had no history of allergies or drug intolerance. He reported to a local hospital with fever, vomiting, cervical and inguinal nodules, abdominal pain, and generalized body macular rash. The patient was transferred to our transplant center after the onset of jaundice and encephalopathy. He was admitted to the intensive care unit with facial edema, generalized scaling exanthema, and acute hepatitis. Serological tests for viral hepatitis and all autoimmune antibodies were negative. Laboratory tests showed a total eosinophil count of 3220/mm3 (normal < 500 mm3), high level of transaminases (aspartate aminotransferase = 1303 IU/L; alanine aminotransferase = 1768 IU/L, lactate dehydrogenase level of 2274 IU/L (normal, 240‐480 IU/L), total bilirubin level of 18.47 mg/dL, direct bilirubin level of 14.81 mg/dL, prothrombin time (PT), international normalized ratio (INR) of 5.18, and factor V 17% (normal, 50%‐150%). The MELD score was 43.
An abdominal ultrasound examination identified no chronic liver disease. The RegiSCAR (Registry of Severe Cutaneous Adverse Reaction) 7 system scored 5 points, confirming the DRESS syndrome diagnosis. Skin biopsy observed interface and spongiotic dermatitis, consistent with drug eruption.
Following the Clichy criteria, 8 the patient was worked up for urgent orthotopic liver transplantation (OLT), which was performed 24 hours after admission. At the time, he was under corticosteroids and clinical support, including mechanic ventilation due to progressive encephalopathy and dialysis due to lactic acidosis.
The orthotopic liver transplantation was uneventful. While liver function improved in the postoperative period, the patient developed sepsis requiring high doses of vasopressors. Broad‐spectrum antibiotics were introduced (third‐generation cephalosporin associated with ampicillin and then switched to carbapenem), but the patient remained hemodynamically unstable. The laboratory test showed progressively increasing acidosis and lactate levels, aspartate aminotransferase = 230 IU/L, alanine aminotransferase = 110 IU/L, total bilirubin level of 2 mg/dL, and INR of 1.5. The patient died on the seventh postoperative day. Blood cultures showed growth of Klebsiella pneumoniae resistant to carbapenems.
2.1. Liver and skin histology
The histological analysis demonstrated massive eosinophilic infiltrates compatible with the diagnosis of DRESS syndrome, and the liver explant showed massive necrosis associated with eosinophilic infiltrate (Figures 1 and 2).
Figure 1.
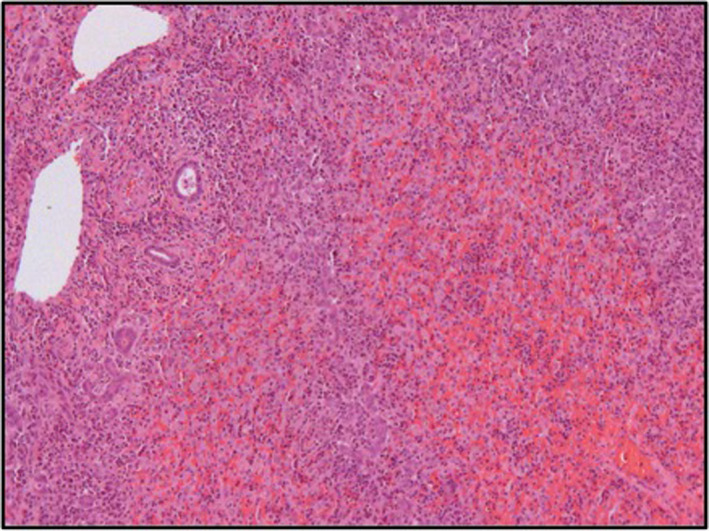
Liver histology. H&E stain. Massive eosinophilic infiltrate with extensive necrosis of the liver compatible with fulminant hepatitis
Figure 2.
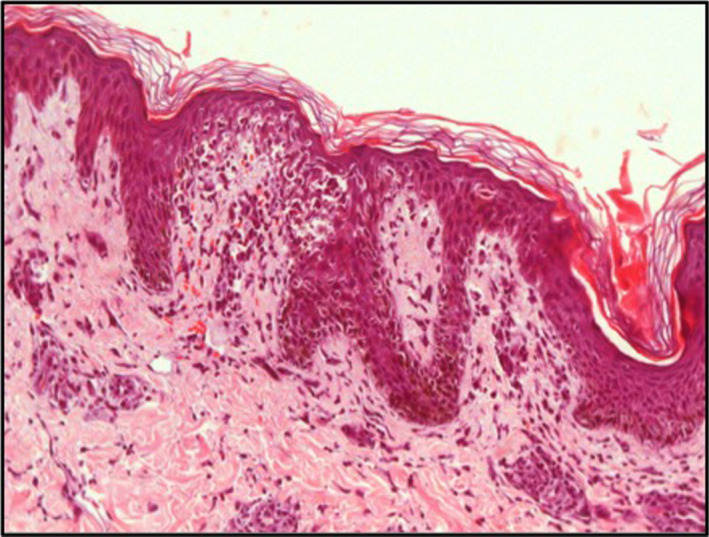
Skin histology. H&E stain. Massive eosinophilic infiltrate compatible with DRESS syndrome
3. DISCUSSION
This report describes an adult patient with DRESS syndrome and liver failure treated with OLT. Liver failure in the setting of DRESS syndrome is quite rare. A few case reports recorded in the literature showed DRESS syndrome and significant hepatic injury (Table 1). In these studies, most of the patients were treated with corticosteroids. 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 Among patients needing liver transplantation, there was approximately 50% perioperative mortality.
Table 1.
Reported cases who had diagnosis of DRESS syndrome caused by associated sulfasalazine and trimethoprim‐sulfamethoxazole
| Case report | Patient | Drug | Treatment | Follow‐up |
|---|---|---|---|---|
| Brooks H et al 9 | 53‐year‐old man | Sulfasalazine | Corticosteroids | Alive |
| Queyrel V et al 10 | 15‐year‐old girl | Sulfasalazine | Corticosteroids | Alive |
| Mainra RR et al 11 | 24‐year‐old woman | Trimethoprim‐sulfamethoxazole | Corticosteroids | Alive |
| Descloux E et al 12 | 45‐year‐old woman | Sulfasalazine | Corticosteroids | Alive |
| Michel F et al 13 | 63‐year‐old woman | sulfasalazine | Corticosteroids | Alive |
| Teo L et al 14 | 49‐year‐old woman | Sulfasalazine | Corticosteroids | Alive |
| Bejia I et al 15 | 46‐year‐old woman | Sulfasalazine | Corticosteroids | Alive |
| de Aquino RT et al 16 | 47‐year‐old woman | Sulfasalazine | Corticosteroids | Alive |
| Augusto JF et al 17 | 77‐year‐old woman | Sulfasalazine | Corticosteroids | Alive |
| Yeşilova Z et al 18 | 38‐year‐old man | Sulfasalazine | Corticosteroids | Alive |
| Rosenbaum J et al 19 | 11‐year‐old girl | Sulfasalazine | Corticosteroids | Alive |
| van der Mark SC et al 20 | 24‐year‐old woman | Sulfasalazine | Corticosteroids | Alive |
| Piñana E et al 21 | 11‐year‐old boy | Sulfasalazine/naproxen | Corticosteroids | Alive |
| Lau G et al 22 | 34‐year‐old woman | Sulfasalazine | Corticosteroids | Died |
| Daoulah A et al 23 | 56‐year‐old woman | Sulfasalazine | Corticosteroids | Died |
| Ng CT et al 24 | 17‐year‐old boy | Trimethoprim‐sulfamethoxazole | MARS | Alive |
| Yusuf IH et al 25 | 15‐year‐old girl | Sulfasalazine | Corticosteroids | Alive |
| Girelli F et al 26 | 53‐year‐old woman | Sulfasalazine/amoxicillin | Corticosteroids | Alive |
| Hernández N et al 27 | 60‐year‐old woman | Sulfasalazine | Corticosteroids | Alive |
| Zaïem A et al 28 | 45‐year‐old woman | Sulfasalazine | Corticosteroids | Alive |
| Ferrero NA et al 29 | 15‐year‐old boy | Sulfasalazine | Corticosteroids | Alive |
| Pirklbauer M et al 30 | A 53‐year‐old woman | Sulfasalazine | Corticosteroids | Alive |
The management of DRESS syndrome is challenging. It is important to withdraw the suspected drug, and the delay is associated with poorer outcomes. 31 , 32 , 33 Supportive therapy in the intensive care unit should be provided to stabilize the patient. Early administration of systemic corticosteroid therapy is generally recommended. 34 A systemic corticosteroid helps to improve both clinical symptoms and laboratory abnormalities within days. 34 Most of the case reports of DRESS syndrome with liver dysfunction showed success with corticosteroid treatment (Table 1).
Liver transplantation is an option when the DRESS syndrome is associated with acute fulminant hepatic failure, but the prognosis remains poor (Table 2). 35 , 36 , 37 , 38 , 39 Besnard et al 35 reported two pediatric Crohn's disease patients undergoing liver transplantation after sulfasalazine‐induced DRESS syndrome. During follow‐up, one of them developed acute rejection and fatal aspergillosis. Amante et al 36 and Roales‐Gómez et al 39 reported adult patients treated with OLT, with no information on long‐term follow‐up. Mennickea et al 37 reported an adult patient treated with OLT, with mortality in the postoperative period due to massive intra‐abdominal blood loss. Song et al 38 reported living‐donor liver transplantation in a 14‐year‐old patient. The patient showed chronic rejection after a 25‐month follow‐up. A living donation would be an alternative to the OLT, mainly in case of the scarce availability of organs in timely fashion.
Table 2.
Patient diagnosed with DRESS undergoing liver transplantation
| Case report | Patient | Drug | Follow‐up |
|---|---|---|---|
| Besnard M et al 35 | 10‐year‐old boy | Sulfasalazine | Died |
| Besnard M et al 35 | 10‐year‐old girl | Sulfasalazine | Alive |
| Amante MF et al 36 | 21‐year‐old woman | Lamotrigine | Unknown |
| Mennickea M et al 37 | 60‐year‐old man | Sulfasalazine/vancomycin | Died |
| Song S et al 38 | 14‐year‐old girl | Vancomycin | Alive |
| Roales‐Gómez V et al 39 | 22‐year‐old man | Ibuprofen | Alive |
| Present study | 18‐year‐old boy | Sulfamethoxazole | Died |
Recent studies support the use of Molecular Adsorbents Recirculation System (MARS), which uses albumin dialysis to mainly replace the liver's detoxification function as a rescue for liver failure patients. Roales‐Gómez et al 39 described MARS use, although the patient did not respond well, and patients eventually underwent OLT. Ng et al 24 reported a pediatric patient that underwent MARS in the intensive care unit with a satisfactory response.
This study showed a patient with sulfasalazine and trimethoprim‐sulfamethoxazole severe reaction. Sulfasalazine and trimethoprim‐sulfamethoxazole carry a significant risk of drug toxicity. Yusuf et al 25 reported the first case of DRESS syndrome in a child treated for toxoplasma retinochoroiditis. Rare cases of immunoallergic reactions to sulfasalazine, including DRESS syndromes, have been reported, such as the classic “3‐week sulfasalazine syndrome” occurring three weeks after the first administration. 9 The treatment of this reaction with a hefty dose of steroids, which can depress the immune system and can flare infections, most likely impacted the postoperative outcomes in the present case.
4. CONCLUSION
DRESS syndrome associated with acute liver failure is a life‐threatening condition. Liver transplantation is an option for the management of these patients, although the prognosis remains poor.
CONFLICT OF INTEREST
The authors have no conflict of interest.
AUTHORS CONTRIBUTION
Igor Lepski Calil: analyzed and interpreted the data. Rafael Soares Nunes Pinheiro: acquired the data and drafted the article. Ryan Yukimatsu Tanigawa and Francisco Tustumi: drafted the paper. Rafael Antônio Arruda Pecora: revised the paper critically for relevant intellectual content. Ruy Jorge Cruz Junior: revised the paper critically for valuable intellectual content. Luiz Augusto Carneiro D'Albuquerque: conceptualized and designed the study. Jorge Henrique Bento de Sousa: approved the final version to be submitted.
ETHICAL APPROVAL
Local Ethics Committee approved the study.
Calil IL, Tustumi F, Pinheiro RSN, et al. Liver transplantation after DRESS syndrome: A case report and review of the literature. Clin Case Rep. 2020;8:3008–3012. 10.1002/ccr3.3334
REFERENCES
- 1. Newell BD, Moinfar M, Mancini AJ, Nopper AJ. Retrospective analysis of 32 pediatric patients with anticonvulsant hypersensitivity syndrome (ACHSS). Pediatr Dermatol. 2009;26:536‐546. [DOI] [PubMed] [Google Scholar]
- 2. Bocquet H, Bagot M, Roujeau JC. Drug‐induced pseudolymphoma and drug hypersensitivity syndrome (drug rash with eosinophilia and systemic symptoms: DRESS). Semin Cutan Med Surg. 1996;15:250‐257. [DOI] [PubMed] [Google Scholar]
- 3. Naisbitt DJ, Britschgi M, Wong G, et al. Hypersensitivity reactions to carbamazepine: characterisation of the specificity, phenotype and cytokine profile of drug‐specific T‐cell clones. Mol Pharmacol. 2003;63:732‐741. [DOI] [PubMed] [Google Scholar]
- 4. Naisbitt DJ, Farrell J, Wong G, et al. Characterisation of drugspecific T cells in lamotrigine hypersensitivity. J Allergy Clin Immunol. 2003;111:1393‐1403. [DOI] [PubMed] [Google Scholar]
- 5. Eland IA, Dofferhoff AS, Vink R, Zondervan PE, Stricker BH. Colitis may be part of the antiepileptic drug hypersensitivity syndrome. Epilepsia. 1999;40:1780‐1783. [DOI] [PubMed] [Google Scholar]
- 6. Callot V, Roujeau JC, Bagot M, et al. Drug induced pseudolymphoma and hypersensitivity syndrome. Two different clinical entities. Arch Dermatol. 1996;132:1315‐1321. [PubMed] [Google Scholar]
- 7. Kardaun SH, Sidoroff A, Valeyrie‐Allanore L, et al. Variability in the clinical pattern of cutaneous side‐effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2007;156:609‐611. [DOI] [PubMed] [Google Scholar]
- 8. Bernuau J, Goudeau A, Poynard T, et al. Multivariate analysis of prognostic factors in fulminant hepatitis B. Hepatology. 1986;6(4):648‐651. [DOI] [PubMed] [Google Scholar]
- 9. Brooks H, Taylor HG, Nichol FE. The three week sulphasalazine syndrome. Clin Rheumatol. 1992;11:566‐568. [DOI] [PubMed] [Google Scholar]
- 10. Queyrel V, Catteau B, Michon‐Pasturel U, et al. DRESS (Drug Rash with Eosinophilia and Systemic Symptoms) syndrome after sulfasalazine and carmazepine: report of two cases. Rev Med Interne. 2001;22(6):582‐586. [DOI] [PubMed] [Google Scholar]
- 11. Mainra RR, Card SE. Trimethoprim‐sulfamethoxazole‐associated hepatotoxicity ‐ part of a hypersensitivity syndrome. Can J Clin Pharmacol. 2003;10(4):175‐178. [PubMed] [Google Scholar]
- 12. Descloux E, Argaud L, Dumortier J, Scoazec JY, Boillot O, Robert D. Favourable issue of a fulminant hepatitis associated with sulfasalazine DRESS syndrome without liver transplantation. Intensive Care Med. 2005;31(12):1727‐1728. [DOI] [PubMed] [Google Scholar]
- 13. Michel F, Navellou JC, Ferraud D, Toussirot E, Wendling D. DRESS syndrome in a patient on sulfasalazine for rheumatoid arthritis. Joint Bone Spine. 2005;72(1):82‐85. [DOI] [PubMed] [Google Scholar]
- 14. Teo L, Tan E. Sulphasalazine‐induced DRESS. Singapore Med J. 2006;47(3):237‐239. [PubMed] [Google Scholar]
- 15. Bejia I, Ben Hammouda S, Riahi K, et al. DRESS syndrome induced by sulphasalazine in rheumatoid arthritis. Joint Bone Spine. 2006;73(6):764‐765. [DOI] [PubMed] [Google Scholar]
- 16. Aquino RT, Vergueiro CS, Magliari ME, de Freitas TH. Sulfasalazine‐induced DRESS syndrome (Drug Rash with Eosinophilia and Systemic Symptoms). Sao Paulo Med J. 2008;126(4):225‐226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Augusto JF, Sayegh J, Simon A, et al. A case of sulphasalazine‐induced DRESS syndrome with delayed acute interstitial nephritis. Nephrol Dial Transplant. 2009;24(9):2940‐2942. [DOI] [PubMed] [Google Scholar]
- 18. Yeşilova Z, Kantarcioğlu M, Erçin CN, et al. ASulfasalazine‐induced hypersensitivity: a case report of DRESS syndrome. Turk J Gastroenterol. 2009;20(4):298‐299. [DOI] [PubMed] [Google Scholar]
- 19. Rosenbaum J, Alex G, Roberts H, Orchard D. Drug rash with eosinophilia and systemic symptoms secondary to sulfasalazine. J Paediatr Child Health. 2010;46(4):193‐196. [DOI] [PubMed] [Google Scholar]
- 20. van der Mark SC, Segers D, Bakker RC, van Wijngaarden P. DRESS syndrome as a result of sulfasalazine use. Ned Tijdschr Geneeskd. 2010;154(18):A2161. [PubMed] [Google Scholar]
- 21. Piñana E, Lei SH, Merino R, et al. DRESS‐syndrome on sulfasalazine and naproxen treatment for juvenile idiopathic arthritis and reactivation of human herpevirus 6 in an 11‐year‐old Caucasian boy. J Clin Pharm Ther. 2010;35(3):365‐370. [DOI] [PubMed] [Google Scholar]
- 22. Lau G, Kwan C, Meng Chong S. The 3‐week sulphasalazine syndrome strikes again. Forensic Sci Int. 2001;122:79‐84. [DOI] [PubMed] [Google Scholar]
- 23. Daoulah A, Alqahtani AA, Ocheltree SR, Alhabib A, Ocheltree AR. Acute myocardial infarction in a 56‐year‐old female patient treated with sulfasalazine. Am. J Emerg Med. 2012;30(4):638. e1‐3. [DOI] [PubMed] [Google Scholar]
- 24. Ng CT, Tan CK, Oh CC, Chang JP. Successful extracorporeal liver dialysis for the treatment of trimethoprim‐sulfamethoxazole‐induced fulminant hepatic failure. Singapore Med J. 2013;54(5):e113‐e116. [DOI] [PubMed] [Google Scholar]
- 25. Yusuf IH, Sahare P, Hildebrand GD. DRESS syndrome in a child treated toxoplasma retinochoroiditis. J AAPOS. 2013;17(5):521‐523. [DOI] [PubMed] [Google Scholar]
- 26. Girelli F, Bernardi S, Gardelli L, et al. New case of DRESS syndrome induced by sulfasalazine and triggered by amoxicillin. Case Rep Rheumatol. 2013;2013:409152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hernández N, Borrego L, Soler E, Hernández J. Sulfasalazine‐induced linear immunoglobulin A bullous dermatosis with DRESS. Actas Dermosifiliogr. 2013;104(4):343‐346. [DOI] [PubMed] [Google Scholar]
- 28. Zaïem A, Aouinti I, Lakhoua G, et al. Sulfasalazine‐induced DRESS syndrome associated with Epstein Barr virus reactivation. Therapie. 2013;68(5):321‐323. [DOI] [PubMed] [Google Scholar]
- 29. Ferrero NA, Pearson KC, Zedek DC, Morrell DS. Case report of drug rash with eosinophilia and systemic symptoms demonstrating human herpesvirus‐6 reactivation. Pediatr Dermatol. 2013;30(5):608‐613. [DOI] [PubMed] [Google Scholar]
- 30. Pirklbauer M, Gruber J. DRESS syndrome following sulfasalazine treatment. Z. Rheumatol. 2014;73(2):180‐183. [DOI] [PubMed] [Google Scholar]
- 31. Bachot N, Roujeau JC. Differential diagnosis of severe cutaneous drug eruptions. Am J Clin Dermatol. 2003;4:561‐572. [DOI] [PubMed] [Google Scholar]
- 32. Tas S, Simonart T. Drug rash with eosinophilia and systemic symptoms (DRESS syndrome). Acta Clin Belg. 1999;54:197‐200. [PubMed] [Google Scholar]
- 33. Tas S, Simonart T. Management of drug rash with eosinophilia and systemic symptoms (DRESS syndrome): an update. Dermatology. 2003;206:353‐356. [DOI] [PubMed] [Google Scholar]
- 34. Chiou CC, Yang LC, Hung SI, et al. Clinicopathological features and prognosis of drug rash with eosinophilia and systemic symptoms: a study of 30 cases in Taiwan. J Eur Acad Dermatol Venereol. 2008;22:1044‐1049. [DOI] [PubMed] [Google Scholar]
- 35. Besnard M, Debray D, Durand P, Cezard JP, Navarro J. Sulfasalazine‐induced fulminant hepatitis in pediatric Crohn’s disease: report of two cases. J Pediatr Gastroenterol Nutr. 1998;26:119‐120. [DOI] [PubMed] [Google Scholar]
- 36. Amante MF, Filippini AV, Cejas N, Lendoire J, Imventarza O, Parisi C. Dress syndrome and fulminant hepatic failure induced by lamotrigine. Ann Hepatol. 2009;8(1):75‐77. [PubMed] [Google Scholar]
- 37. Mennicke M, Zawodniak A, Keller M, et al. Fulminant liver failure after vancomycin in a sulfasalazine‐induced DRESS syndrome: fatal recurrence after liver transplantation. Am J Transplant. 2009;9(9):2197‐2202. [DOI] [PubMed] [Google Scholar]
- 38. Song SM, Cho MS, Oh SH, et al. Liver transplantation in a child with acute liver failure resulting from drug rash with eosinophilia and systemic symptoms syndrome. Korean J Pediatr. 2012;56(5):224‐226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Roales‐Gómez V, Molero AI, Pérez‐Amarilla I, et al. Colina F DRESS syndrome secondary to ibuprofen as a cause of hyperacute liver failure. Rev Esp Enferm Dig. 2014;106(7):482‐486. [PubMed] [Google Scholar]


