Abstract
Background
The SARS‐CoV‐2 was first reported in December 2019 in Wuhan, China and has been declared a pandemic in March 2020. COVID‐19 has caused unprecedented and lasting biopsychosocial effects worldwide. All healthcare professionals have faced life‐threatening risks by attending their daily jobs. The daily emergence of advice and guidelines was necessary to ensure the safety of patients and staff. To this effect, all elective services came to a halt to preserve hospitals’ capacity for dealing with the sickest. This retrospective, descriptive review aims to assess the volume and timing of the advice released specifically relevant to UK ENT specialists.
Methods
Two separate searches were performed. One involved online advice published in English by international, national and ENT‐specific organisations between January 1 and May 31. The date, title, source, type of advice and link to the advice were recorded in Excel. The resources were analysed per week of publication. A second separate search for peer‐reviewed publications was conducted using PubMed Central and Cochrane databases.
Findings
COVID‐19‐related guidance was considered, of which 175 were identified. 52/175 (29.7%) articles were published by international organisations. 56/175 (32%) were produced by national organisations, and 67/175 (38.28%) were produced by ENT specific organisations. The peak guidance production took place in the third and fourth week of March (16/03/2020‐29/03/2020) with 72/175 publications. Of these, 27/70 came from the international category, 17/70 from national bodies and 26/70 from ENT‐specific organisations. 13 863 total publications relating to COVID‐19 were found using PubMed and Cochrane search strategies; 76% were relevant to ENT.
Conclusion
The challenges faced by ENT relate to the unprecedented, sudden and daily changes to clinical practice. Multiple bodies interpreted the guidance, giving an opportunity for confusion and delay in treatments for patients. Implementing a system with clear lines of communication and dissemination of information will improve our response to future pandemic events whilst maintaining a commercial awareness to better use the human and financial resources of an already financially restricted NHS.
Keywords: aerosol‐generating procedures, elective, emergency, ENT, head and neck cancer, healthcare, SARS‐CoV‐2, service
Keypoints.
Since the start of the COVID‐19 pandemic, healthcare systems around the world have entered a period of uncertainty having to re‐organise practices to provide safe care for patients and a safe environment for staff.
The daily emergence of guidance as infection rates was climbing represents one of the challenges encountered in practice.
Overall, 175 publications originating from international, national and ENT specific bodies were identified; of which, 70 arose during the peak publication period between 16 March 2020 and 29 March 2020. Of the 13 863 peer‐reviewed publications relating to COVID‐19, the peak occurred in the last week of March.
The timing of these publications, as the mortality from COVID‐19 was also rising, represents a challenge to incorporate all the advice into safe clinical practice.
As the number of COVID‐19‐related cases begins to rise for a second time, we should endeavour to flatten the infection and mortality rates curve and shift the information curve to the left, allowing our healthcare system to prepare and implement changes into practice in a timely manner.
1. INTRODUCTION
The COVID‐19 pandemic caused by the SARS‐CoV‐2 coronavirus infection has challenged the world's healthcare systems in an unprecedented way. 1 , 2 In the UK and wider world, there has been a lot of discussion about how to change the shape of the SARS‐CoV‐2 incidence and associated mortality curve. The aim of this study is to look at the shape and timing of the information curve, in particular with reference to otolaryngology in the UK. Although the broad principles may apply to other specialities and in other countries.
The result of the pandemic has led to a significant reduction in GP cancer referrals, elective otolaryngology and cancer surgery. 3 , 4 , 5 This reduction is due to a number of factors, including access to healthcare and re‐purposing theatre suites, ventilators and staff. Additionally, evidence suggests an unacceptably high morbidity and mortality if patients contract COVID‐19 in the perioperative period. 6 , 7 , 8 , 9
Furthermore, there has been significant concern as to the risks to the surgical team. 10 Early evidence emerged that surgeons, in particular otolaryngologists, as well as other professionals operating on the aerodigestive tract, were at particularly high risk. This is due to the high level of aerosol‐generating procedures involved in the speciality. A number of fatalities among otolaryngologists and other similar practitioners have been reported. 4 , 11
During the pandemic, there have been a significant number of guidelines produced by international sources, UK governmental organisations as well as specialist bodies such as the Royal Colleges and specialist organisations. These guidelines deal with a number of issues, including personal protective equipment, prioritisation of treatment and recovery, and, specific to ENT, cancer, clinics, tracheostomy, rhinology, otology and paediatrics. 4 , 5 , 6 , 12 , 13 , 14 , 15 , 16 , 17
The volume and quantity of guidelines resulted in significant challenges for otolaryngologists to stay up to date and to incorporate the advice into safe practice, both for the patient and the clinician. In addition to published advice, otolaryngologists have been required to assimilate guidance produced by local hospitals, as well as considering government briefings, web‐based discussion, the press and social media.
This study aims to document the volume and timing of advice targeted at ENT practice. The value of this study is to highlight the need for a pathway and establish a framework prior to any future overwhelming medical emergency leading to agreed pathways to disseminate information from high‐level organisations (such as NHS England/WHO) down to area‐specific advice (such as ENT‐UK, BAHNO). This would ensure there are no disparities in the information and a clear message can be communicated. There should be an agreed checking point of the quality of advice and clear guidance on how promptly it should be evaluated in light of emerging information and developments. With the possibility of “second” waves, it is critical that this is implemented.
2. MATERIALS AND METHODS
Two separate searches were conducted. The first considered online advice published in English by official sources between 1 January and 31 May relevant to hospital‐based practitioners involved in aerosol‐generating procedures (Table S2a). The sources were broadly grouped in international, national and ENT‐specific organisations.
The international resources included the World Health Organisation (WHO) and other relevant groups publishing advice relevant to ENT and surgical services (Centre for Medicare and Medicaid Services, American Academy of Otolaryngology and Head and Neck, Stanford Group, ENT Canada, American College of Surgeons). The COVID‐19 advice page compiled by the Cochrane group was used to select relevant international resources. 18
National resources included advice from Public Health England (PHE), National Institute for Clinical Excellence (NICE), National Health Service (NHS) website, Academy of Medical Royal Colleges and Royal Colleges (of Surgeons, Radiologists, Pathology, Speech and Language Therapy).
ENT‐specific organisations included ENT‐UK, British Association of Head and Neck Oncologists (BAHNO), British Laryngology Association (BLA), British Rhinological Society (BRS) and British Society of Otology (BSO).
Microsoft Excel for Mac (version 16.41, Year 2020) was used to record the data by date, title, publishing organisation, type of advice and hyperlink for each day since January 1. The results were subsequently grouped per week; thus, each Monday of the month since January 1 reflects all results from the previous week. The type of advice referred to areas of concern during the pandemic—PPE, service prioritisation, general (advice on treatment and/or investigations), cancer, tracheostomy, otology, rhinology, paediatric ENT and service recovery.
The volume of advice published weekly in each of the three main categories aforementioned was reviewed. The number of SARS‐CoV‐2‐related deaths recorded during the above period was extracted from the government website. 19 This was used to analyse the trajectory of COVID‐19 related deaths and the volume of advice published between 1 January 2020 and 31 May 2020.
The second search included the electronic databases PubMed Central and Cochrane library which were considered separately using the same strategy from the 30 December 2019 to 31 May 2020 (Tables S1,S2b). Initially, all publications related to COVID‐19 were identified, the duplicates were filtered and number of publications by week was calculated.
Next, a subset of these COVID‐19 papers relating to ENT were identified. These papers were categorised according to those describing subspecialties within ENT, common ENT symptoms, anatomical areas relevant to ENT, and research relating to personal protective equipment, service prioritisation and recovery following the COVID‐19 pandemic. The official UK government website was again used to map daily laboratory‐confirmed cases in England and UK deaths across the same time period. 19
Ethical approval was not required as this study was a review, and all data were extracted from published articles.
3. RESULTS
A total of 194 COVID‐19 ENT‐related guidance were identified during the 20 weeks between 1 January 2020 and 31 May 2020. 19 of these 194 were duplicates published by multiple organisations as collaborative work. Of 175 original articles, 52/175 (29.70%) were published by international organisations, 57/175 (32%) by national organisations and 66/175 (38.20%) by ENT specific organisations (Figure 1).
Figure 1.
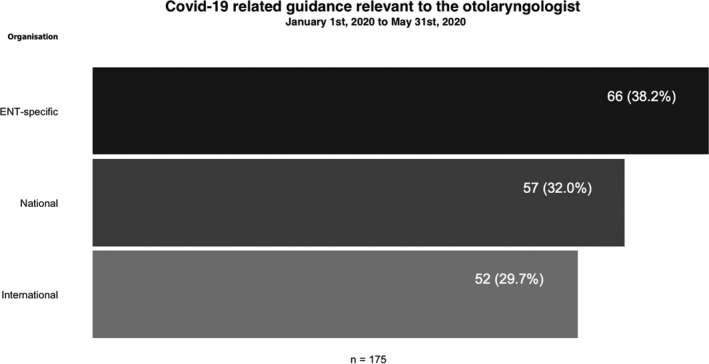
Covid‐19‐related guidance relevant to the otolaryngologist (1 January 2020 to 31 May 2020)
The identified guidance covered multiple topics, separated into 10 main areas. PPE was the subject in 31%, service prioritisation (13%), general advice relating to treating elective otolaryngological conditions either surgically or conservatively (20%), screening (4%), cancer care (8%), tracheostomy (7%) with specific areas of otology (4.1%), rhinology (4%), paediatric ENT (3%) and service recovery (5%). In total, 313 topic areas were covered in the 175 publications (Table 1).
Table 1.
Subject of the advice covered by the Covid‐19‐related guidance relevant to the Otolaryngologist between 1 January 2020 and 31 May 2020
| Area | Advice area covered total 313 |
|---|---|
| PPE | 97 |
| Service prioritisation | 41 |
| General (treatment, investigations and/or prevention) | 63 |
| Screening | 13 |
| Cancer | 26 |
| Tracheostomy | 22 |
| Otology | 13 |
| Rhinology | 13 |
| Paediatric ENT | 9 |
| Service recovery | 16 |
The WHO declared the pandemic on 11 March 2020. 20 Before this date, only 8/175 guidance had been published. Following this, there was a rapid escalation. The peak guidance production, totalling 70/175, took place in the third and fourth week of March (16 to 29 of March 2020) with 33/175 publications in the third week of March and 37/175 in the fourth week (Figure 2).
Figure 2.
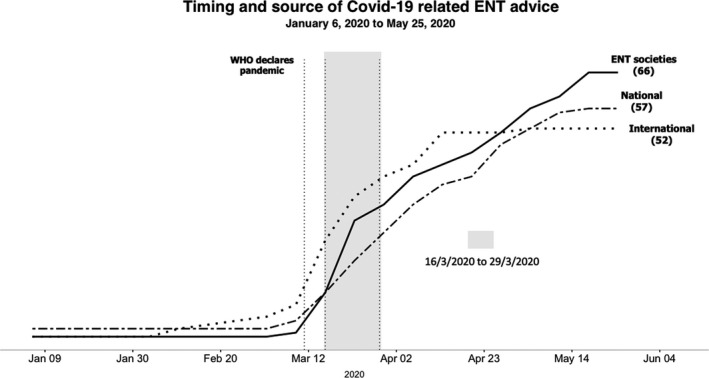
Timing and source of UK advice relating to Covid‐19 by organisation between 6 January 2020 and 25 May 2020 (NB 6 January marks 1st Monday of January thus includes guidance released during the previous 6 d; analysis concludes on 25 May as no guidance was identified between 25 May and 31 May)
Of these 70 publications, 27 came from the international category, 17 from national bodies and 26 from ENT‐specific organisations. During this peak period, the majority of advice related to PPE (48/70, 68.5%) (Table 2).
Table 2.
Advice subject covered by the 70 Covid‐19‐related guidance relevant to the Otolaryngologist during the peak period (16/03/2020‐29/03/2020)
| Area | Number of publications, N = 70 |
|---|---|
| PPE | 48 |
| Service prioritisation | 16 |
| General (treatment, investigations and/or prevention) | 29 |
| Screening | 7 |
| Cancer | 13 |
| Tracheostomy | 13 |
| Otology | 7 |
| Rhinology | 5 |
| Paediatric ENT | 5 |
| Service recovery | 0 |
Publications relating to NHS service recovery began two‐weeks following the peak guidance period. Between the 9 April and the 20 May, 16 guidance on service recovery was identified. During this period, the number of publications increased by an average of 2.2 per week, with a peak of 5 publications during the second week of May.
12 publications came from national and ENT‐specific bodies: 5 from ENT‐UK, 2 from the Royal College of Surgeons, 3 from Public Health England, 1 from the Royal College of Radiologists and 1 from the NHS website. 4 came from international bodies including the American Academy of Otolaryngology and Head and Neck, Centres for Medicare and Medicaid.
Most guidance targeted at otology, rhinology and paediatric ENT was produced during the peak period, constituting 10%, 7.1% and 7.1%, respectively. During the subsequent four weeks, between one and two pieces of advice were produced per week before the number of publications tailed off.
A total of 13 863 peer‐reviewed publications relating to COVID‐19 were identified using PubMed and Cochrane searches. When the pandemic was announced, there had been 966 COVID‐19‐related publications, of which 610 targeted otolaryngology. The volume increased over time, with a sharp increase occurring at the end of March 2020 when a total of 10 567 publications relating to ENT were identified (Figure 3).
Figure 3.
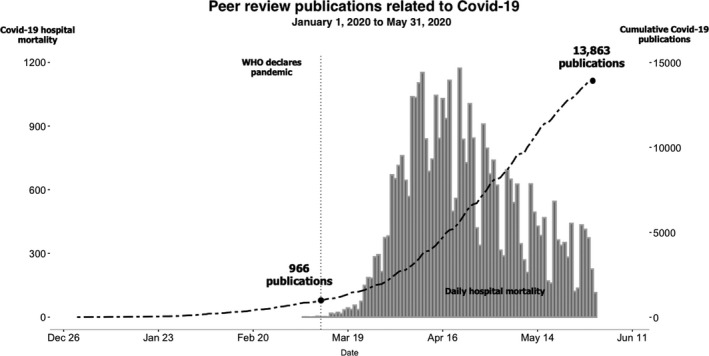
Peer‐review publications related to Covid‐19 (1 January 2020 to 31 May 2020)
4. DISCUSSION
The WHO considered SARS‐cov‐2 infection to be a global pandemic on 11 March 2020. 20 This study documents the advice that ENT allied specialties in the UK would need to read and assimilate to prioritise, protect and triage patients as well as staff during this period.
As we emerge from the first wave of this unprecedented world‐wide pandemic, we must learn lessons. Since the start of this century, there have been a number of epidemics; all have arisen outside the UK, including Ebola, severe acute respiratory syndrome (SARS), H1N1 influenza pandemic, Middle East Respiratory Syndrome (MERS) and H5N1. 21 The COVID‐19 pandemic represents an opportunity to analyse retrospectively the UK’s response in terms of the volume and timing in which information was produced.
The virus, first noticed in Wuhan, spread throughout the world. Whilst the infection was recognised as a pandemic on 11 March, UK incidence numbers did not start to significantly rise until later in March, with a probable peak in mid‐April 2020. By the time, the infection was recognised as a global risk, there had been a significant number of cases reported worldwide.
Otolaryngologists and other medical practitioners performing aerosol‐generating procedures (AGPs) were identified early on as being at a high risk. 4 , 10 While this study is specific to this subset of medical practitioners, the volume of advice and the time it was produced is likely to be applicable to other specialties.
This study has identified 175 guidance‐related publications issued from a number of international, governmental and specialist groups relevant to ENT as per Figure 1. The subject of that advice covered a number of topics included in Table 1. It is likely that this is an underestimate of the total guidance produced.
During this period, medical services have been required to rapidly redevelop to allow for appropriate provision of care for COVID‐19 patients. There has also been a need to limit hospital visits, rationalise procedures and limit surgical operations. 16 , 22 The latter reflects the risks to patients contracting COVID‐19 in the perioperative period and the high rate of pulmonary complications and mortality. In addition to protecting patients, there has been considerable guidance on how best to protect medical staff. As a consequence, a large number of clinical pathways have been changed. The long‐term impact of such changes remains to be assessed. 7 , 23
The peak time for guidance production in the UK was between 16 March 2020 and 29 March 2020. During this time, numbers of COVID‐19 cases in the UK were rising rapidly. Specific advice regarding clinical aspects of care required an assimilation of publicly available information, published data and international experience. This review illustrates that there were a number of rapidly published guidelines which informed clinical practice. Limitations of timescale mean that guidelines have not always been evidence‐based and have been formulated by opinion and consensus, often relying on collaborative approaches. 24 , 25 , 26 , 27
Peer‐review publications have followed the pandemic, with an estimated 13 863 COVID‐19‐related publications, of which 76% related to ENT. It can be seen that there has been an unprecedented number of publications published during the pandemic. Many articles have been released using preprint servers and promoted on social media before peer review. Even after peer review at least two high profile journals have had to retract publications. 28 This reflects the significance of the event but also the challenges in medicine to understand and utilise this information. With infection rates climbing and large volumes of advice being produced on a daily basis, it was challenging to incorporate it into clinical practice safely.
This study is illustrative of the challenges faced by ENT in absorbing, assimilating and implementing the advice produced. Much of the advice was produced while the numbers of new cases were increasing. While this is targeted to the otolaryngologist, it is likely that this pattern of advice and timing is relevant to other specialities operating in different regions of the world.
Within the UK much of the discussion has been about flattening the curve of infections. This study suggests that there is also a need to move the information curve to the left. There is also a need to flatten the information curve. National and international guidance advice needs to be assimilated into advice that relates to specific procedures considering the physical setting in which they will occur, local practice and availability of equipment. Having multiple bodies interpreting the guidance is an opportunity for confusion. Ultimately, this may result in a failure to follow the guidance, potentially putting medical personnel or patients at risk, or an over‐interpretation of advice resulting in treatment being withheld.
The number of COVID‐19 infections is on the rise and the possibility of a second wave provides opportunities to generate and co‐ordinate the advice needed by otolaryngologists as well as other medical professionals. Much like the early warning system introduced after the 2004 Tsunami, there is a need to establish a similar system in the UK with clear lines of communication and dissemination of information. 29
An objective framework collating key points from emerging evidence grouped into relevant areas of practice could act as portal for clinicians to use in guiding their daily clinical work. This would ensure a timely update of healthcare practitioners involved in high‐risk procedures during times of declared pandemics.
CONFLICTS OF INTEREST
Professor Winter is a member of International Editorial Board of Clinical Otolaryngology and had received grant funding from NIHR and Oracle Cancer Trust. There are no other disclosures or conflicts of interest to declare.
AUTHOR CONTRIBUTIONS
Dr Cristina Cernei involved in data collection, analysis, project writing, editing and submission. Dr Manu Shrivastava involved in data collection, analysis and results description. Mr William Colquhoun‐Flannery involved in data analysis and figures creation. Professor Stuart Winter involved in overall supervision, discussion and editing.
ETHICAL APPROVAL
This work did not require any patient sensitive data and did not focus on any patient intervention, therefore, ethical approval was not necessary.
Supporting information
Table S1‐S2
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Cernei C, Shrivastava MK, Colquhoun‐Flannery W, Winter SC. Timing and volume of information produced for the Otolaryngologist during the COVID‐19 pandemic in the UK: A review of the volume of online literature. Clin Otolaryngol.2021;46:318–324. 10.1111/coa.13669
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in the Supporting Information of this article.
REFERENCES
- 1. Fontanarosa PB, Bauchner H. COVID‐19—looking beyond tomorrow for health care and society. JAMA. 2020;323(19):1907‐1908. [DOI] [PubMed] [Google Scholar]
- 2. Zhu N, Zhang D, Wang W, et al. A novel Coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727‐733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mahase E. Covid‐19: urgent cancer referrals fall by 60%, showing “brutal” impact of pandemic. BMJ. 2020;369:m2386. [DOI] [PubMed] [Google Scholar]
- 4. Givi B, Schiff BA, Chinn SB, et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID‐19 pandemic. JAMA Otolaryngol Head Neck Surg. 2020;146(6):579–584. [DOI] [PubMed] [Google Scholar]
- 5. Collaborative C. Global guidance for surgical care during the COVID‐19 pandemic. Br J Surg. 2020;107:1097–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Couloigner V, Schmerber S, Nicollas R, et al. COVID‐19 and ENT surgery. Eur Ann Otorhinolaryngol Head Neck Dis. 2020;137(3):161‐166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Day AT, Sher DJ, Lee RC, et al. Head and neck oncology during the COVID‐19 pandemic: reconsidering traditional treatment paradigms in light of new surgical and other multilevel risks. Oral Oncol. 2020;105:104684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID‐19 infection. EClinicalMedicine. 2020;23(100385):1–1. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(20)30129-2/fulltext [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nepogodiev D, Glasbey JC, Li E, et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS‐CoV‐2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bandyopadhyay S, Baticulon R, Kadhum M, et al. Infection and mortality of healthcare workers worldwide from COVID‐19: a scoping review. medRxiv; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vukkadala N, Qian ZJ, Holsinger FC, Patel ZM, Rosenthal E. COVID‐19 and the Otolaryngologist: preliminary evidence‐based review. Laryngoscope. 2020;130(11):2537–2543. [DOI] [PubMed] [Google Scholar]
- 12. Mehanna H, Hardman JC, Shenson JA, et al. Recommendations for head and neck surgical oncology practice in a setting of acute severe resource constraint during the COVID‐19 pandemic: an international consensus. Lancet Oncol. 2020;21:16–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Argenziano M, Fischkoff K, Smith CR. Surgery scheduling in a crisis. N Engl J Med. 2020;382(23):e87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Head MA, Consortium NSTG, members C , et al. Head and neck surgical oncology in the time of a pandemic: Subsite‐specific triage guidelines during the COVID‐19 pandemic. Head Neck 2020;42(6):1194‐1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Paleri V, Hardman J, Tikka T, Bradley P, Pracy P, Kerawala C. Rapid implementation of an evidence‐based remote triaging system for assessment of suspected referrals and patients with head and neck cancer on follow‐up after treatment during the COVID‐19 pandemic: model for international collaboration. Head Neck. 2020;42(7):1674–1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dharmarajan H, Anderson JL, Kim S, et al. Transition to a virtual multidisciplinary tumor board during the COVID‐19 pandemic: University of Pittsburgh experience. Head Neck. 2020;42(6):1310‐1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shuman AG, Campbell BH, Ethics A, Service P. Ethical framework for head and neck cancer care impacted by COVID‐19. Head Neck. 2020:1214‐1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cochrane ENT . COVID‐19 (coronavirus disease) – ENT, Hearing & Balance [Internet]. Cochrane Collaboration; [updated 2020 May; cited 2020 May 30]. Available from: https://ent.cochrane.org/news/covid-19-coronavirus-disease-ent-hearing-balance
- 19. Public Health England and NHSX . GOV.UK Coronavirus (COVID‐19) in the UK [Internet]. UK: GOV.UK; [updated 2020 May 30; cited 2020 Jun 6]. Available from: https://coronavirus.data.gov.uk/?_ga=2.237121091.2105726748.1588817632-725862875.1586435801
- 20. General WHOD . WHO Director‐General’s opening remarks at the media briefing on COVID‐19 – 11 March 2020; 2020.
- 21. World Health Organisation . Emergencies preparedness, response. How the 4 biggest outbreaks since the start of this century shattered some long‐standing myths [Internet]. WHO; [Updated 2020; cited 2020 May 30]. Available from: https://www.who.int/csr/disease/ebola/ebola-6-months/myths/en/
- 22. Workman AD, Welling DB, Carter BS, et al. Endonasal instrumentation and aerosolization risk in the era of COVID‐19: simulation, literature review, and proposed mitigation strategies. Int Forum Allergy Rhinol. 2020;10(7):798–805. [DOI] [PubMed] [Google Scholar]
- 23. Richards M, Anderson M, Carter P, Ebert BL, Mossialos E. The impact of the COVID‐19 pandemic on cancer care. Nat Cancer. 2020;1(6):565‐567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Thomson DJ, Palma D, Guckenberger M, et al. Practice recommendations for risk‐adapted head and neck cancer radiation therapy during the COVID‐19 pandemic: an ASTRO‐ESTRO Consensus Statement. Int J Radiat Oncol Biol Phys. 2020;107(4):618–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Topf MC, Shenson JA, Holsinger FC, et al. Framework for prioritizing head and neck surgery during the COVID‐19 pandemic. Head Neck. 2020:1159‐1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yan F, Nguyen SA. Head and neck cancer: high‐risk population for COVID‐19. Head Neck. 2020;42(6):1150‐1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kowalski LP, Sanabria A, Ridge JA, et al. COVID‐19 pandemic: effects and evidence‐based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020;42(6):1259‐1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wise J. Data transparency: “Nothing has changed since Tamiflu”. BMJ. 2020;369:m2279. [DOI] [PubMed] [Google Scholar]
- 29. Zahari RK, Ariffin RNR, Asmawi MZ, Ibrahim AN. Impacts of the 2004 Tsunami: preparedness of the Malaysian coastal communities. ScienceDirect. [Internet] 2013. [cited 2020 May 30];105:569‐576. 10.1016/j.sbspro.2013.11.060 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1‐S2
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Data Availability Statement
The data that support the findings of this study are available in the Supporting Information of this article.


